Rectal prolapse, also known as rectal procidentia Procidentia Pelvic Organ Prolapse, is the protrusion of rectal tissue through the anus. The tissue may include just the mucosa or the full thickness of the rectal wall. Common risk factors include chronic straining, constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation, bowel motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility disorders, and weakening of the pelvic floor Pelvic floor Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy muscles. The diagnosis is primarily clinical. In children, rectal prolapse can be managed conservatively with hydration, fiber, stool softeners, and treatment of any predisposing conditions. In adults, the prolapse is often complete and requires surgical management.
Last updated: Jun 18, 2025
Rectal prolapse is associated with several predisposing conditions and risk factors:
Rectal prolapse is the protrusion of rectal tissue through the anal orifice and is classified as follows:
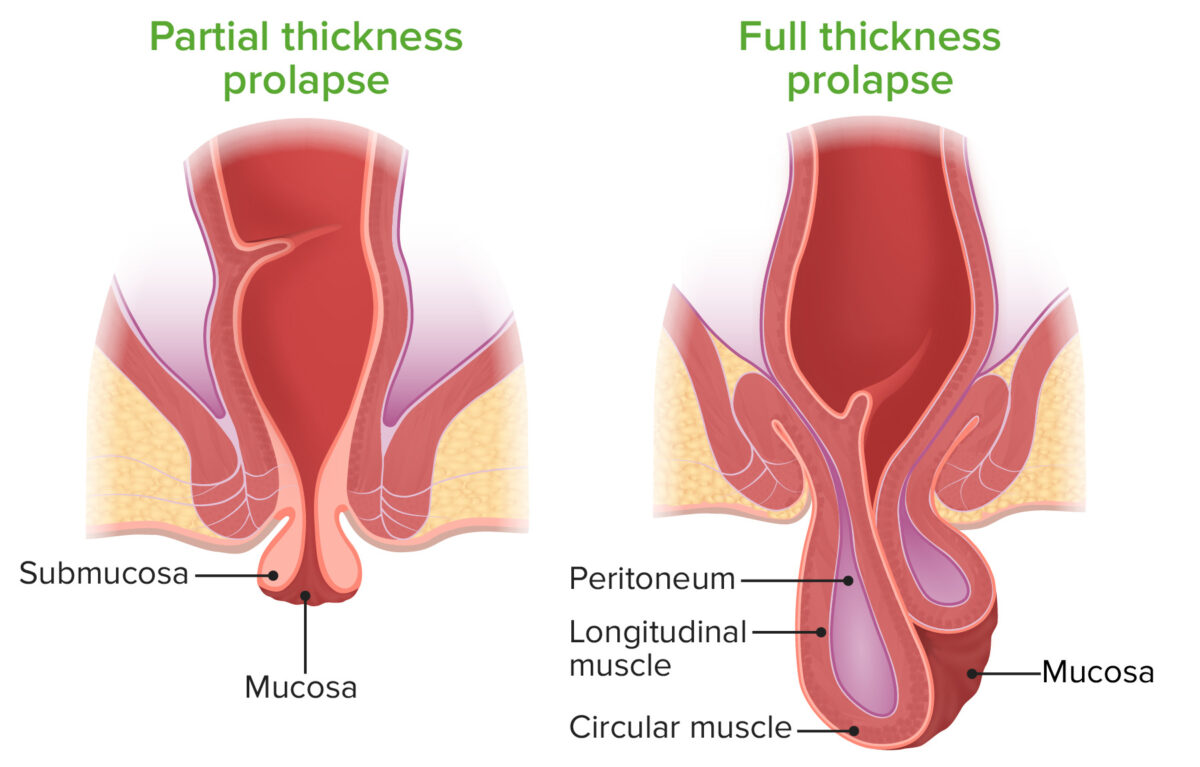
Partial versus complete rectal prolapse:
A partial rectal prolapse (left) is characterized by mucosal tissue protruding through the anal canal. A complete (full-thickness) rectal prolapse (right) is characterized by involvement of the full thickness of the rectal wall.

A full-thickness (complete) rectal prolapse
Image: “Prolapse of rectum 01” by Dr. K.-H. Günther. License: CC BY 3.0Conservative management:
Surgical management: