Splenic rupture is a medical emergency that carries a significant risk of hypovolemic shock Hypovolemic Shock Types of Shock and death. Injury to the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy accounts for nearly half of all injuries to intra-abdominal organs. The most common reason for a rupture of the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy is blunt abdominal trauma, specifically, motor vehicle accidents Motor Vehicle Accidents Spinal Cord Injuries. For individuals with splenomegaly Splenomegaly Splenomegaly is pathologic enlargement of the spleen that is attributable to numerous causes, including infections, hemoglobinopathies, infiltrative processes, and outflow obstruction of the portal vein. Splenomegaly, however, even minimal trauma may result in splenic injury or rupture. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship often present with LUQ abdominal pain Abdominal Pain Acute Abdomen; however, pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways may be referred to the left shoulder. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are at risk for hemodynamic instability due to blood loss. The diagnosis is generally made with CT imaging, and management, ranging from observation to splenectomy, depends on the patient’s hemodynamic stability.
Last updated: Jan 11, 2024
Splenic rupture is often associated with trauma (e.g., motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology vehicle accident) that causes a laceration Laceration Torn, ragged, mangled wounds. Blunt Chest Trauma of the organ.
Splenic rupture can have serious consequences because of the unique physiologic function of the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy.
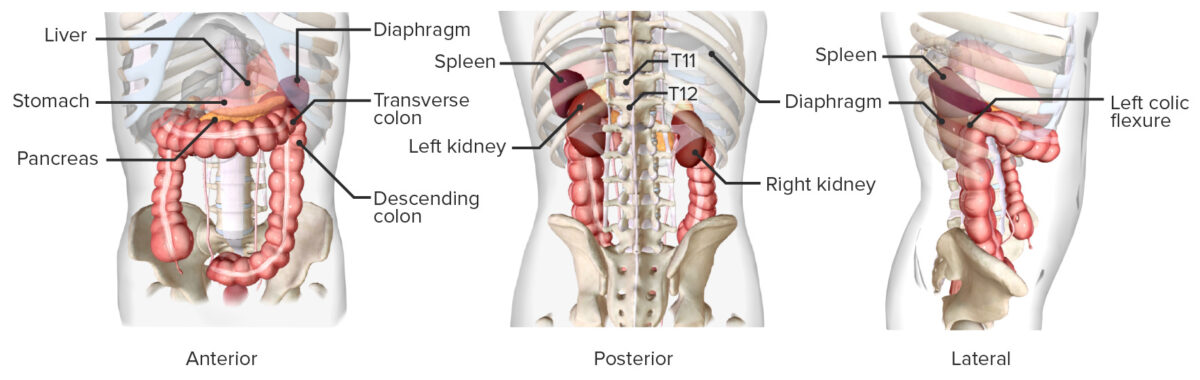
Location of the spleen
Image by BioDigital, edited by LecturioPhysical examination and history may be useful, but not all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with splenic rupture present with clinically significant findings.
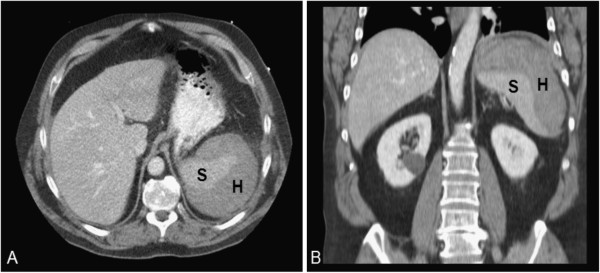
CT of abdomen of patient with splenic rupture:
Splenic rupture has multiple possible etiologies. Clinical exam and history are often insufficient for diagnosis. A CT of the abdomen can reveal areas of hematoma (H) or free blood.
S: spleen
Management of splenic rupture depends on the patient’s hemodynamic status:
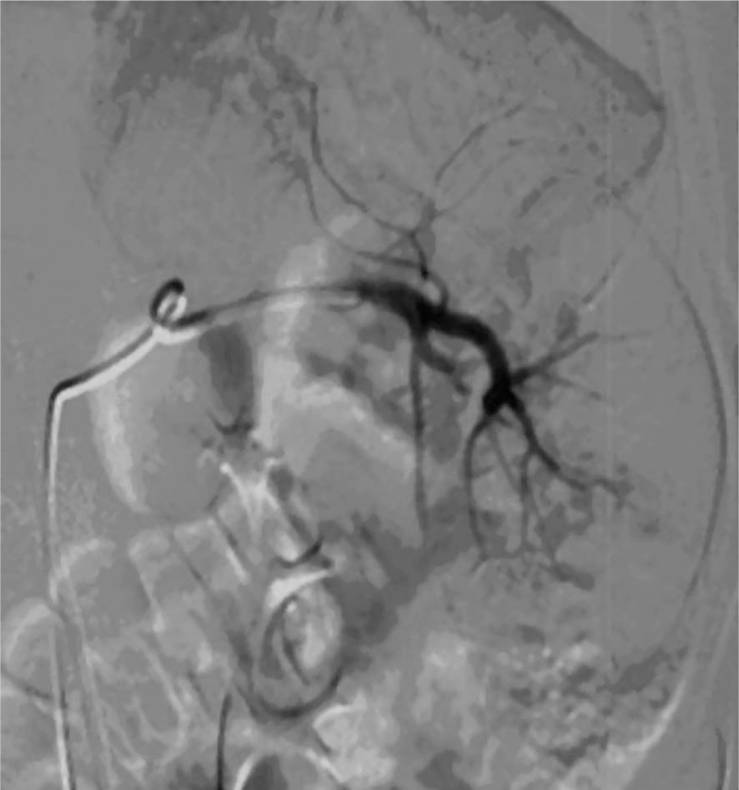
Splenic artery embolization:
This image shows angiographic embolization in the setting of splenic injury. Great improvements have been made in outcomes with nonsurgical treatment of hemodynamically stable patients.
Postsplenectomy:
Asplenic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship require vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination against encapsulated Encapsulated Klebsiella bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology: