Relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever is a vector-borne Vector-Borne Antimalarial Drugs disease caused by multiple species of the spirochete Spirochete Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema Borrelia Borrelia Borrelia are gram-negative microaerophilic spirochetes. Owing to their small size, they are not easily seen on Gram stain but can be visualized using dark-field microscopy, Giemsa, or Wright stain. Spirochetes are motile and move in a characteristic spinning fashion due to axial filaments in the periplasmic space. Borrelia. There are 2 major forms of relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever: tick-borne relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever (caused by multiple species, such as B. hermsii B. hermsii Borrelia, B. miyamotoi B. miyamotoi Borrelia, and B. turicatae B. turicatae Borrelia) and louse-borne relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever (caused by B. recurrentis B. recurrentis Borrelia). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship go through recurrent stages of fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, crisis phase, and afebrile periods. Severe manifestations can include myocarditis Myocarditis Myocarditis is an inflammatory disease of the myocardium, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation and myocyte injury, most often leading to signs and symptoms of heart failure. Myocarditis, ARDS, and meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis. Diagnosis is based on the clinical history and visualization of spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema on a thick and thin blood smear Blood smear Myeloperoxidase Deficiency obtained during a febrile episode. Management of relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever is with antibiotics, such as doxycycline, penicillin Penicillin Rheumatic Fever, or ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should be monitored closely for Jarisch-Herxheimer reaction Jarisch-Herxheimer Reaction Lyme Disease.
Last updated: Nov 7, 2022
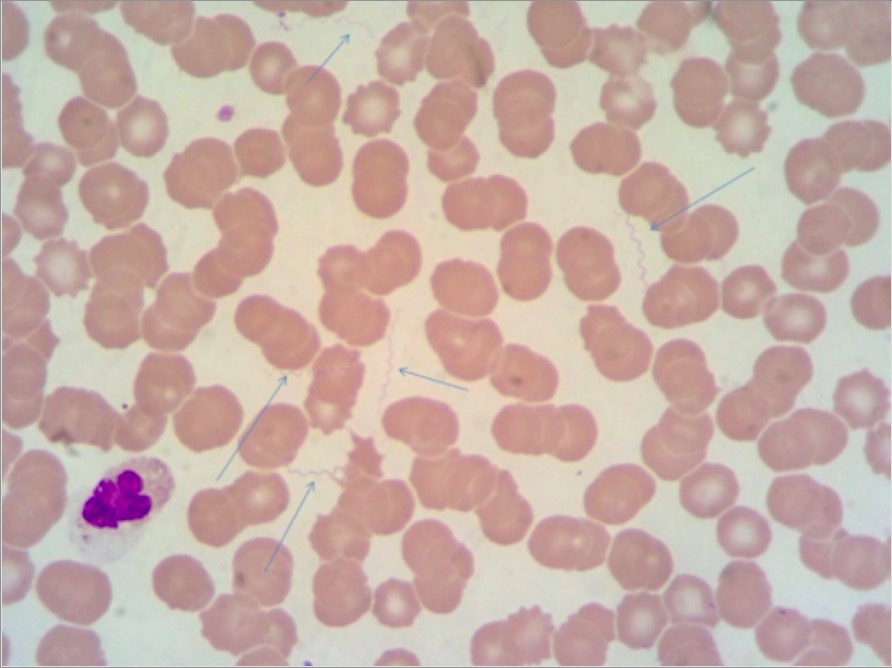
May-Grünwald-Giemsa (MGG)–stained thin blood smear showing numerous spirochetes (arrows) identified as Borrelia recurrentis
Image: “MGG stain” by Department of Clinical and Biomedical Sciences Luigi Sacco, University of Milano, Milano, Italy. License: CC BY 4.0Tick-borne relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever:
Louse-borne relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever:
Findings indicative of poor prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas:
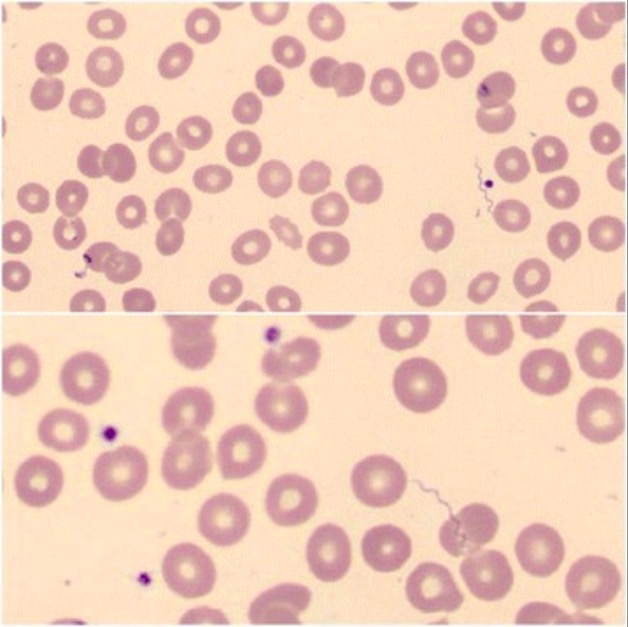
Blood smear showing Borrelia:
Blood smear of a patient with tick-borne relapsing fever secondary to Borrelia hispanica. Irregular coils of spirochetes are seen.
Other supporting tests and findings:
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can be treated with a single dose of: