Mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage is a rare, life-threatening condition caused by inadequate blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through the mesenteric vessels, which results in ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage and necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage of the intestinal wall. Mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage can be either acute or chronic. Acute mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage may be caused by an arterial embolism, thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus, non-occlusive disease, or venous thrombosis Venous thrombosis The formation or presence of a blood clot (thrombus) within a vein. Budd-Chiari Syndrome. Chronic mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage is most commonly caused by atherosclerotic disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with abdominal pain Abdominal Pain Acute Abdomen out of proportion to the abdominal examination Abdominal examination The abdominal examination is the portion of the physical exam evaluating the abdomen for signs of disease. The abdominal examination consists of inspection, auscultation, percussion, and palpation. Abdominal Examination. Peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury, sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock, and hematochezia Hematochezia Gastrointestinal Bleeding are concerning for bowel infarction. Computed tomography (CT) with angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery of the abdomen and pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 "hip" bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy is the diagnostic modality of choice. Management is often surgical and focuses on re-establishing blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the intestines, as well as resection of any nonviable bowel.
Last updated: Jun 1, 2025
Mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage is a condition caused by hypoperfusion of the intestine, resulting in ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage and necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage. Mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage is categorized based on the time course:
The main vessels affected in mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage include:
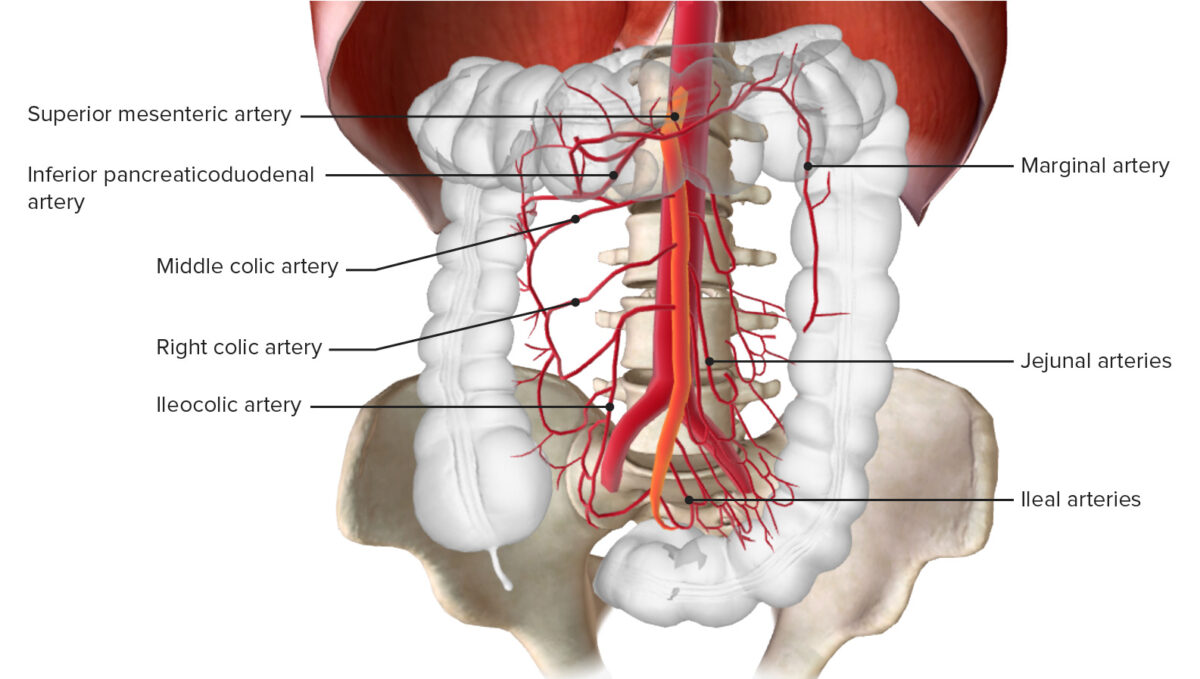
Blood supply of the colon through the inferior mesenteric artery
Image by BioDigital, edited by Lecturio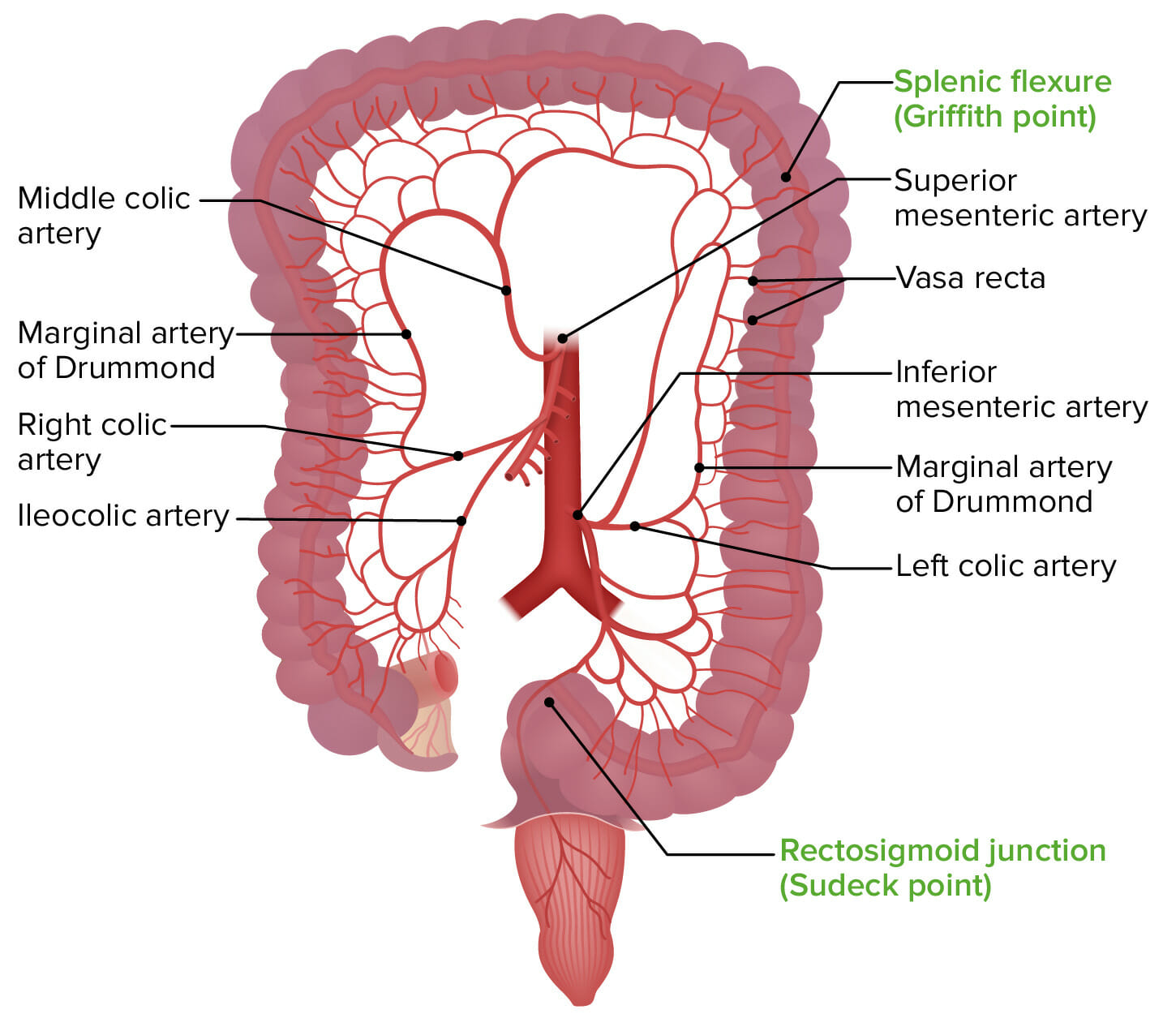
Illustration showing the Griffith point and the Sudeck point, the areas most vulnerable to mesenteric ischemia
Image by Lecturio.Acute mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage requires a high index of suspicion to allow a timely diagnosis.

Computed tomography (CT) angiography in acute mesenteric ischemia: The circle indicates an occlusive embolism of the mid-portion of the SMA.
Image: “Coronal MIP reconstructions of CTA” by Association of Radiology & Oncology. License: CC BY 3.0, edited by Lecturio.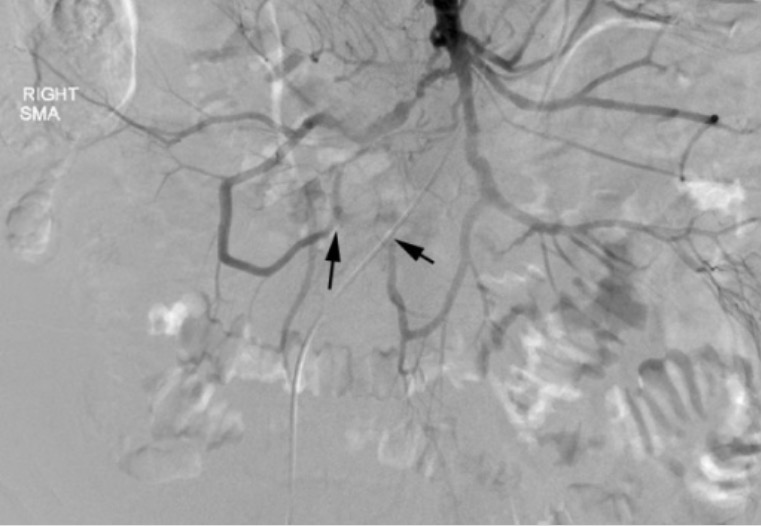
Mesenteric angiogram findings in acute mesenteric ischemia:
Cannulation of the SMA, shown here, reveals severe stenosis or occlusion of multiple SMA branches (black arrows).
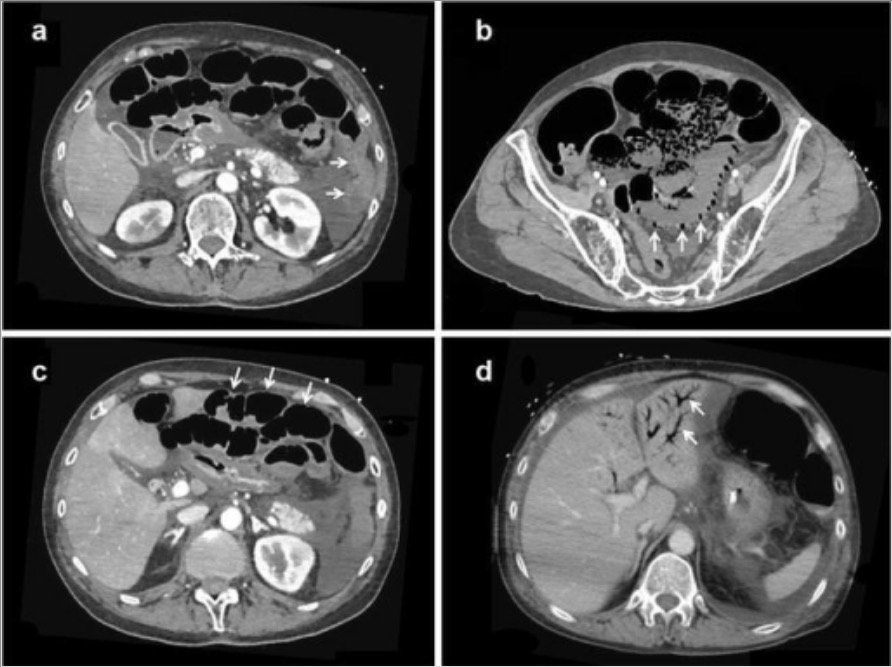
Computed tomography (CT) angiography of non-occlusive mesenteric ischemia:
a: The absence of contrast-induced bowel wall enhancement (arrows)
b: Pneumatosis intestinalis and absence of contrast-induced bowel wall enhancement (arrows)
c: Bowel dilatation and the absence of contrast-induced bowel wall enhancement (arrows)
d: Portal venous gas (arrows)

Computed tomography (CT) image of ischemic bowel due to thrombosis of the superior mesenteric vein:
Note the dilated bowel with a thickened bowel wall.

Surgical findings in mesenteric ischemia:
Picture of eviscerated small bowel during an exploratory laparotomy with healthy pink bowel to the top left and dark, dusky, ischemic bowel to the lower right
Chronic mesenteric ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage is caused by a progressive stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) of ≥ 2 arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, resulting in episodes of blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure supply and demand mismatch (usually after eating).
Vascular imaging studies are used to make the diagnosis.