Cholelithiasis (gallstones) is the presence of stones in the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy. Most gallstones are cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism stones, while the rest are composed of bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism (pigment stones) and other mixed components. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are commonly asymptomatic but may present with biliary colic (intermittent pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in the right upper quadrant Right upper quadrant Anterior Abdominal Wall: Anatomy). The diagnosis is established by ultrasound. Management options include supportive care to prevent and control associated symptoms. When indicated, cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy is the definitive treatment. Gallstones may lead to complications such as choledocholithiasis (a stone trapped in the common bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy duct), cholecystitis Cholecystitis Cholecystitis is the inflammation of the gallbladder (GB) usually caused by the obstruction of the cystic duct (acute cholecystitis). Mechanical irritation by gallstones can also produce chronic GB inflammation. Cholecystitis is one of the most common complications of cholelithiasis but inflammation without gallstones can occur in a minority of patients. Cholecystitis ( inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy), or cholangitis (biliary sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock). These conditions require urgent medical attention Attention Focusing on certain aspects of current experience to the exclusion of others. It is the act of heeding or taking notice or concentrating. Psychiatric Assessment.
Last updated: May 17, 2024
Cholelithiasis is the presence of gallstones in the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy.

Opened gallbladder with gallstones
Image: “Opened gall bladder containing numerous gallstones” by Emmanuelm. License: CC BY 3.0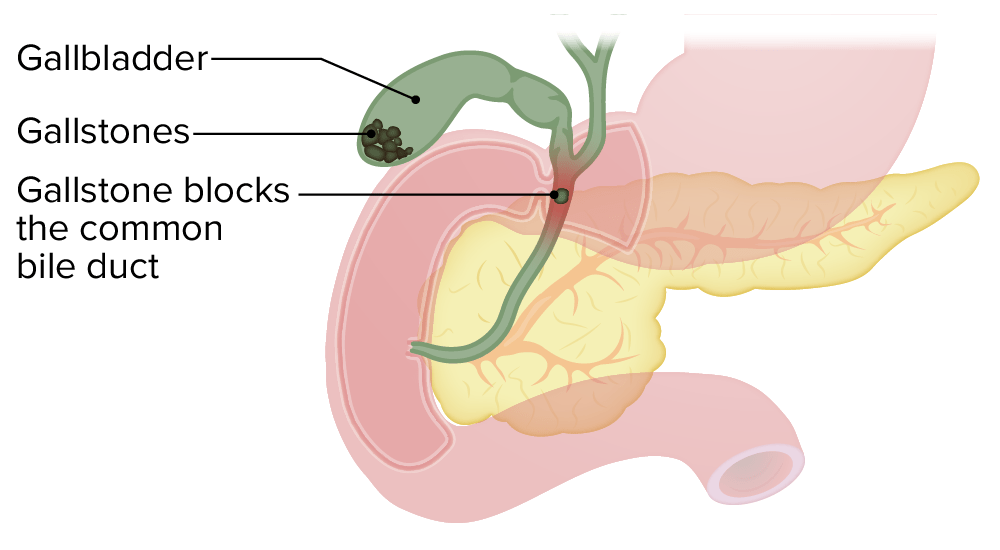
Gallstones are formed in the gallbladder. Obstruction of the biliary tract by a gallstone can lead to symptoms.
Image by Lecturio.Risk factors for cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism stones: 4 Fs
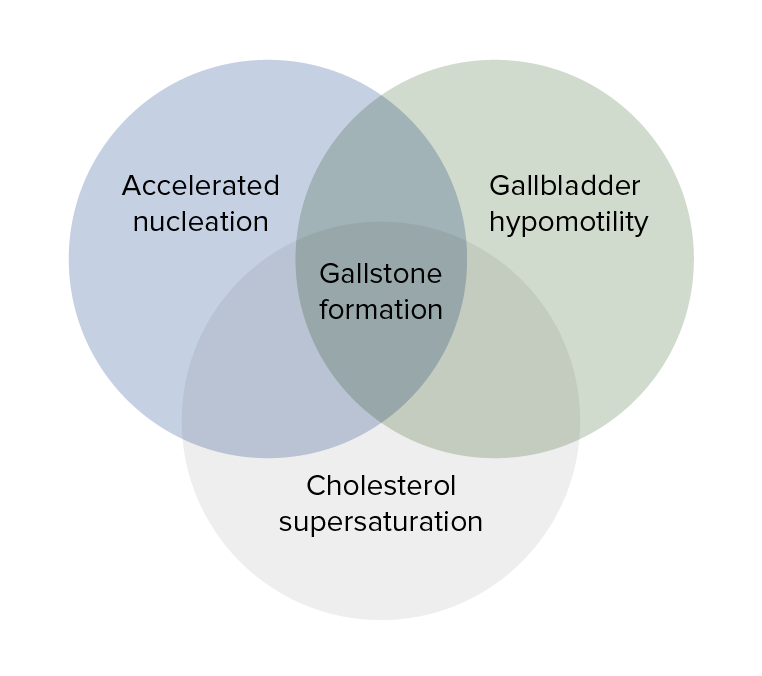
Overlapping mechanisms that produce gallstones: cholesterol supersaturation, gallbladder hypomotility, and accelerated nucleation
Image by Lecturio.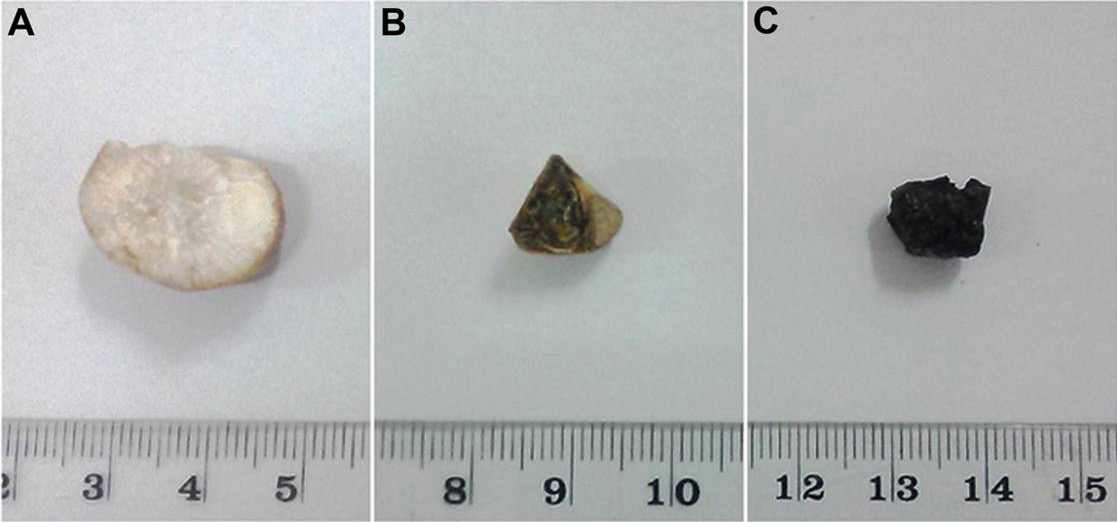
A: cholesterol gallstone
B: mixed gallstone
C: black pigment gallstone

Ultrasound showing gallstone (arrow) within the gallbladder
Image: “Anterior/posterior abdominal radiograph” by Division of Pediatric Surgery, Children’s Hospital Los Angeles, 4650 Sunset Blvd Mailstop 100, Los Angeles, CA 90027, USA. License: CC BY 2.0
Ultrasound showing gallstone (green highlight) with posterior acoustic shadow
Image: “Cholecystitis” by Mazzei et al. License: CC BY 2.0, edited by Lecturio.| Condition | Pathology | Clinical presentation | Laboratory studies | Diagnostic imaging | Management |
|---|---|---|---|---|---|
| Cholecystitis Cholecystitis Cholecystitis is the inflammation of the gallbladder (GB) usually caused by the obstruction of the cystic duct (acute cholecystitis). Mechanical irritation by gallstones can also produce chronic GB inflammation. Cholecystitis is one of the most common complications of cholelithiasis but inflammation without gallstones can occur in a minority of patients. Cholecystitis | Cystic Cystic Fibrocystic Change duct obstruction with inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation | Constant RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways (> 6 hours), Murphy’s sign | ↑ WBC | US | Urgent cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy |
| Choledocholithiasis | Gallstone in
CBD
CBD
Atypical Parkinsonian Syndromes causing obstruction
|
Postprandial colicky RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways > 6 hours; others: jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice, acholic stool, dark urine, pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema) | ↑ Bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism, ALP ALP An enzyme that catalyzes the conversion of an orthophosphoric monoester and water to an alcohol and orthophosphate. Osteosarcoma | US, MRCP MRCP Non-invasive diagnostic technique for visualizing the pancreatic ducts and bile ducts without the use of injected contrast media or x-ray. Mri scans provide excellent sensitivity for duct dilatation, biliary stricture, and intraductal abnormalities. Primary Sclerosing Cholangitis | ERCP ERCP Fiberoptic endoscopy designed for duodenal observation and cannulation of vater’s ampulla, in order to visualize the pancreatic and biliary duct system by retrograde injection of contrast media. Endoscopic (vater) papillotomy may be performed during this procedure. Primary Sclerosing Cholangitis for stone removal → cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy to prevent recurrence |
| Acute cholangitis Acute Cholangitis Acute cholangitis is a life-threatening condition characterized by fever, jaundice, and abdominal pain which develops as a result of stasis and infection of the biliary tract. Septic shock, liver abscess, and multi-organ dysfunction are potential serious complications. Acute Cholangitis | Choledocholithiasis with infection; with biliary sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock (E. coli, Klebsiella Klebsiella Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli. They form pink colonies on MacConkey agar due to lactose fermentation. The main virulence factor is a polysaccharide capsule. Klebsiella pneumoniae is the most important pathogenic species. Klebsiella, Pseudomonas Pseudomonas Pseudomonas is a non-lactose-fermenting, gram-negative bacillus that produces pyocyanin, which gives it a characteristic blue-green color. Pseudomonas is found ubiquitously in the environment, as well as in moist reservoirs, such as hospital sinks and respiratory equipment. Pseudomonas, Enterococcus Enterococcus Enterococcus is a genus of oval-shaped gram-positive cocci that are arranged in pairs or short chains. Distinguishing factors include optochin resistance and the presence of pyrrolidonyl arylamidase (PYR) and Lancefield D antigen. Enterococcus is part of the normal flora of the human GI tract. Enterococcus) |
|
↑ WBC, ↑ bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism, ALP ALP An enzyme that catalyzes the conversion of an orthophosphoric monoester and water to an alcohol and orthophosphate. Osteosarcoma | US, MRCP MRCP Non-invasive diagnostic technique for visualizing the pancreatic ducts and bile ducts without the use of injected contrast media or x-ray. Mri scans provide excellent sensitivity for duct dilatation, biliary stricture, and intraductal abnormalities. Primary Sclerosing Cholangitis | ERCP ERCP Fiberoptic endoscopy designed for duodenal observation and cannulation of vater’s ampulla, in order to visualize the pancreatic and biliary duct system by retrograde injection of contrast media. Endoscopic (vater) papillotomy may be performed during this procedure. Primary Sclerosing Cholangitis → emergent cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy |
| Gallstone pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis | Small stones transiently obstructing pancreatic duct | Epigastric pain Epigastric pain Mallory-Weiss Syndrome (Mallory-Weiss Tear), nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics/ vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia | ↑ WBC, ↑ amylase Amylase A group of amylolytic enzymes that cleave starch, glycogen, and related alpha-1, 4-glucans. Digestion and Absorption/ lipase Lipase An enzyme of the hydrolase class that catalyzes the reaction of triacylglycerol and water to yield diacylglycerol and a fatty acid anion. It is produced by glands on the tongue and by the pancreas and initiates the digestion of dietary fats. Malabsorption and Maldigestion, ↑ bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism, ALP ALP An enzyme that catalyzes the conversion of an orthophosphoric monoester and water to an alcohol and orthophosphate. Osteosarcoma | MRCP MRCP Non-invasive diagnostic technique for visualizing the pancreatic ducts and bile ducts without the use of injected contrast media or x-ray. Mri scans provide excellent sensitivity for duct dilatation, biliary stricture, and intraductal abnormalities. Primary Sclerosing Cholangitis/CT scan | Delayed cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy |
| Gallstone ileus Ileus A condition caused by the lack of intestinal peristalsis or intestinal motility without any mechanical obstruction. This interference of the flow of intestinal contents often leads to intestinal obstruction. Ileus may be classified into postoperative, inflammatory, metabolic, neurogenic, and drug-induced. Small Bowel Obstruction | Large stone (> 2.5 cm) passing into the small bowel Small bowel The small intestine is the longest part of the GI tract, extending from the pyloric orifice of the stomach to the ileocecal junction. The small intestine is the major organ responsible for chemical digestion and absorption of nutrients. It is divided into 3 segments: the duodenum, the jejunum, and the ileum. Small Intestine: Anatomy through a cholecystoduodenal fistula Fistula Abnormal communication most commonly seen between two internal organs, or between an internal organ and the surface of the body. Anal Fistula → obstruction | Small bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis (diffuse abdominal pain Abdominal Pain Acute Abdomen, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics/ vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia) | ↑ WBC | CT scan | Surgery to extract the stone ( cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy not performed in the same setting) |