Congenital duodenal obstructions are a group of inborn conditions that cause obstruction of the lumen of the duodenal segment of the small intestine Small intestine The small intestine is the longest part of the GI tract, extending from the pyloric orifice of the stomach to the ileocecal junction. The small intestine is the major organ responsible for chemical digestion and absorption of nutrients. It is divided into 3 segments: the duodenum, the jejunum, and the ileum. Small Intestine: Anatomy, impeding the passage of food and gastric juices. The condition may have intrinsic etiologies, such as duodenal atresia Atresia Hypoplastic Left Heart Syndrome (HLHS) (most common) and/or extrinsic etiologies, such as an annular Annular Dermatologic Examination pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy. The hallmark of duodenal obstruction is bilious vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. The condition can be diagnosed through prenatal or postnatal ultrasound. Associated anomalies, including congenital heart disease, are common. Treatment includes fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome and surgical duodenoduodenostomy.
Last updated: Jun 27, 2025
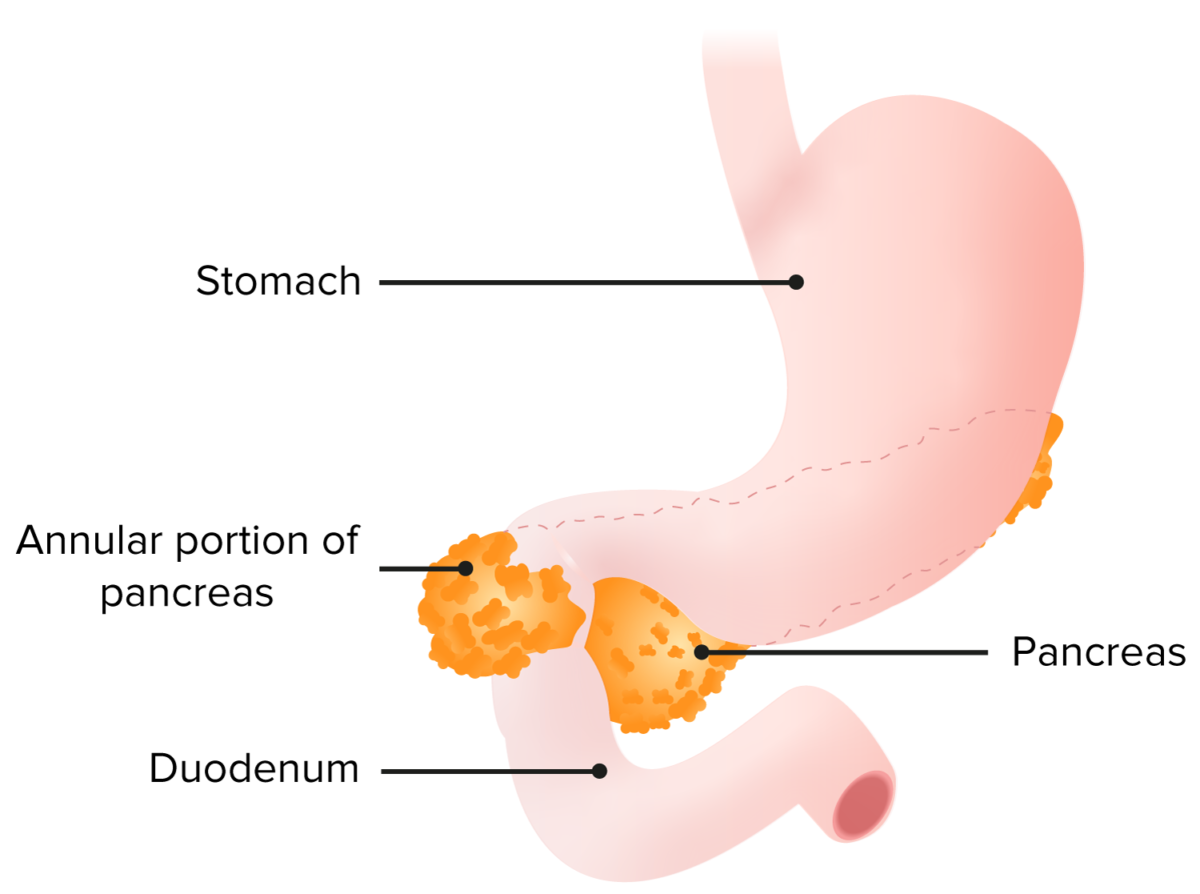
Annular pancreas with a band of pancreatic tissue surrounding the duodenum leading to obstruction caused by a malrotation of the pancreatic bud during development
Image by Lecturio.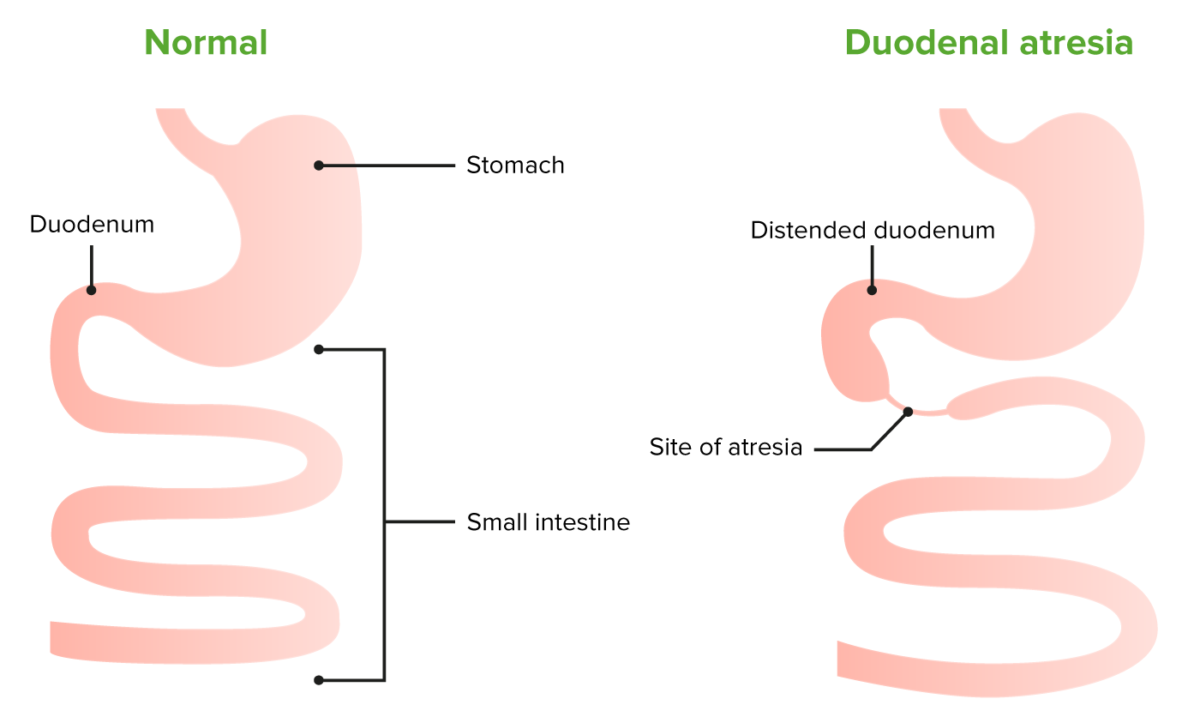
Anatomical comparison between a healthy small intestine and duodenal atresia.
Duodenal atresia is caused by the failure of the duodenum to recanalize during embryonal development.
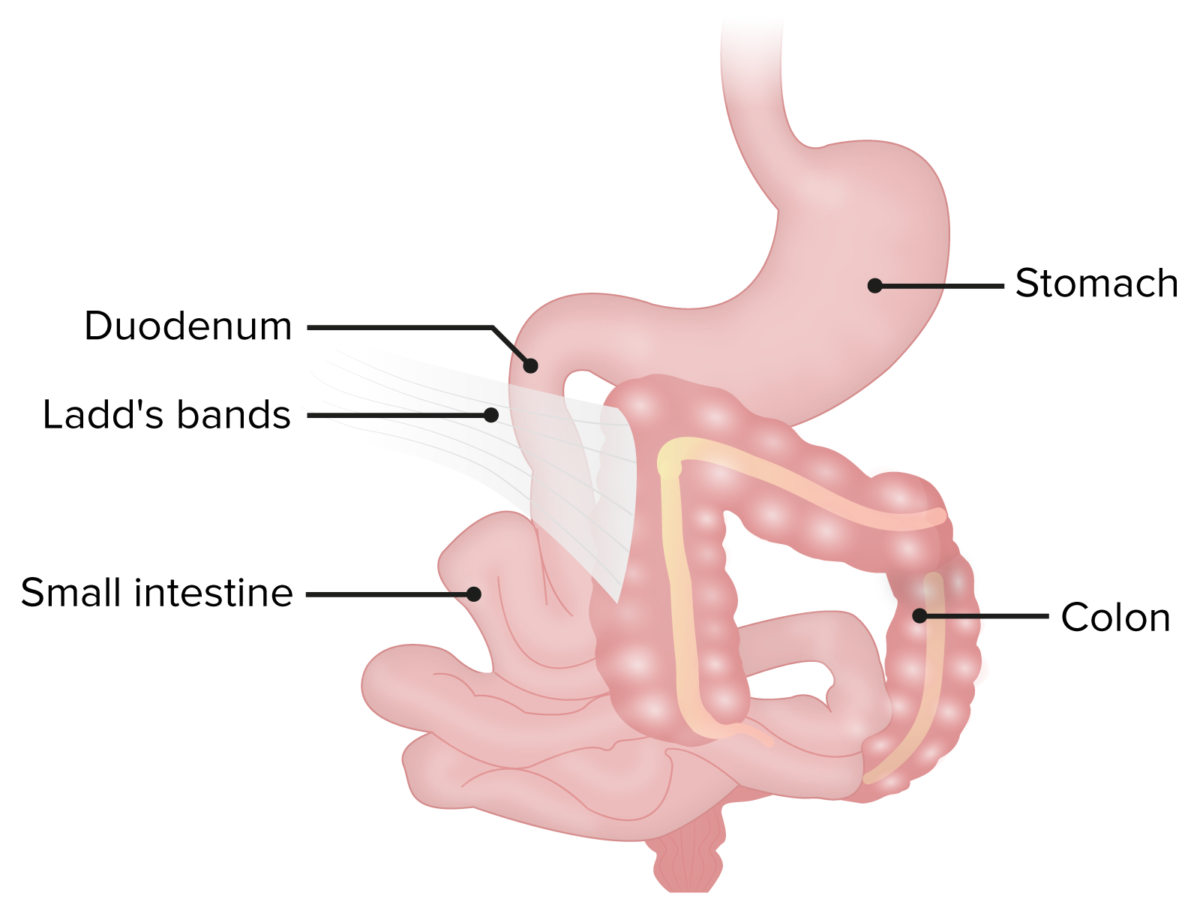
Ladd bands in a patient with malrotation.
The bands of fibrous peritoneal tissue can put pressure on and obstruct the duodenum.
Signs and symptoms of intestinal obstruction Intestinal obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis:
Associated abnormalities:
History
Physical exam
Imaging

Prenatal ultrasound showing fetal double bubble sign with polyhydramnios
Image: “Congenital Duodenal Obstruction in Neonates” by Journal of Neonatal Surgery. License: CC BY 3.0
Double bubble sign in a patient with duodenal atresia
Image: “Alimentary Tract Atresias associated with Anorectal Malformations” by Journal of Neonatal Surgery. License: CC BY 3.0Medical therapy
Surgical management
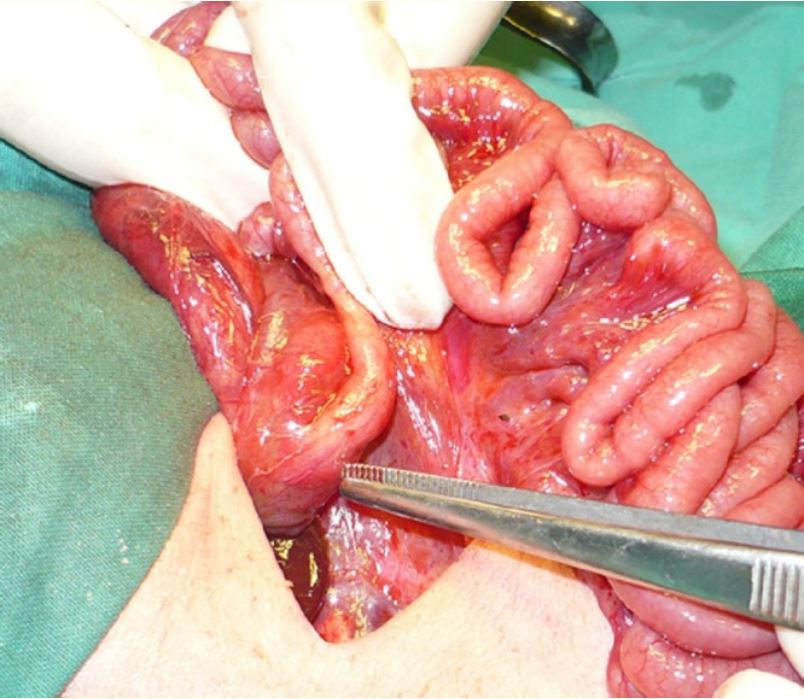
Duodenal atresia
Image: “Multiple associated anomalies in patients of duodenal atresia: a case series” by Mirza B, Sheikh A. License: CC BY 3.0