Perforated viscus or GI perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis represents a condition in which the integrity of the GI wall is lost with subsequent leakage of enteric contents into the peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy, resulting in peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury. The causes of perforated viscus include trauma, bowel ischemia Bowel ischemia Mesenteric ischemia is a rare, life-threatening condition caused by inadequate blood flow through the mesenteric vessels, which results in ischemia and necrosis of the intestinal wall. Mesenteric ischemia can be either acute or chronic. Mesenteric Ischemia, infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, or ulcerative conditions, all of which ultimately lead to a full-thickness disruption of the intestinal wall. Perforated viscus presents as sudden onset of abdominal pain Abdominal Pain Acute Abdomen, distention, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, obstipation Obstipation Large Bowel Obstruction, and symptoms of peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury. Diagnosis relies on the medical history as well as imaging studies, including abdominal and pelvic CT scan and X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests. Treatment includes bowel rest, the use of a nasogastric tube Nasogastric tube Malnutrition in children in resource-limited countries, antibiotics to avoid severe infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease or sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock, analgesics, and surgical repair.
Last updated: Apr 10, 2025
A perforated viscus, also known as intestinal or bowel perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, is a full-thickness disruption of the intestinal wall, with subsequent leakage of enteric contents into the peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy, resulting in a systemic inflammatory response, peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury, and possibly sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock.
Vitals:
Abdominal exam:
Atypical presentation:

Postoperative CT scan demonstrating a large-volume pneumoperitoneum due to bronchoperitoneal fistula
Image: “Post-operative computed tomography (CT) scan” by Johns Hopkins Hospital, Department of Surgery, Baltimore, MD, USA. License: CC BY 2.0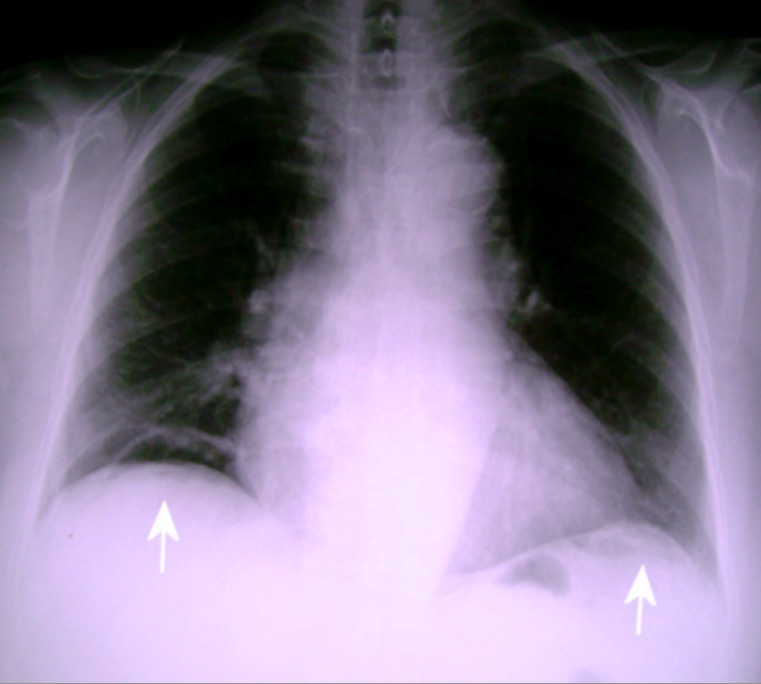
Upright posteroanterior chest X-ray:
Presence of free subdiaphragmatic air bilaterally, which is more clearly noted on the right side (white arrows).