Dilated cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types (DCM) is the most common type of non-ischemic cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types and a common cause of heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) (HF). The cause may be idiopathic Idiopathic Dermatomyositis, familial, or secondary to a variety of underlying conditions. The disease is characterized by the enlargement of 1 or both ventricles and reduced systolic function. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with symptoms of HF such as shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, weakness, and peripheral edema Peripheral edema Peripheral edema is the swelling of the lower extremities, namely, legs, feet, and ankles. Edema. Blood tests, ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), X-rays X-rays X-rays are high-energy particles of electromagnetic radiation used in the medical field for the generation of anatomical images. X-rays are projected through the body of a patient and onto a film, and this technique is called conventional or projectional radiography. X-rays, echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA), and other cardiac studies and procedures are typically done to obtain the diagnosis. Treatment includes medications used to reduce volume overload (e.g., diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication) and manage HF (e.g., beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers)). Devices such as pacemakers and cardioverter-defibrillators may also be needed. In severe cases, a heart transplant is required. Complications include thromboembolic events and sudden cardiac death Sudden cardiac death Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest.
Last updated: May 16, 2024
Dilated cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types (DCM) is a disease of the cardiac muscle Cardiac muscle The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Muscle Tissue: Histology:
Symptoms may develop and progress slowly over time, or develop abruptly. Symptoms are similar to those seen with HF.

Pitting edema of the lower extremity:
Fluid accumulation in the soft tissue of the lower extremities can be a sign of HF of multiple etiologies.
Diagnosis is primarily through history and physical examination, laboratory examination, ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), and imaging (confirmatory or to exclude other etiologies).
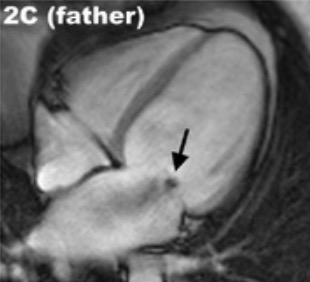
Imaging of DCM with MRI:
Dilated cardiomyopathy (DCM) with functional mitral regurgitation (black arrow) can be more finely quantified and studied thanks to advanced imaging modalities.
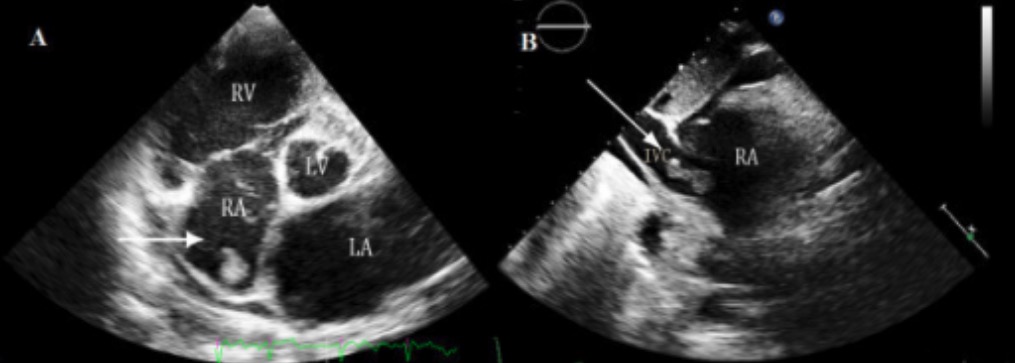
Echocardiogram of DCM:
Echocardiogram is often a 1st-line tool utilized to assess cardiomyopathy, giving extensive information regarding the heart’s size, structure, and function. An echocardiogram can also identify complications (such as the right atrial thrombus viewed here) through real-time 3D transthoracic echocardiography in a patient with dilated cardiomyopathy.
Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is generally poor for individuals with this condition.