Heavy metal poisoning is the toxic accumulation of metals in the body, which can occur due to ingestion or inhalation. These elements are normally found in nature and can have many applications (e.g., agriculture, medicine, industry); however, toxicity Toxicity Dosage Calculation is rare. Common metals that the human body absorbs in toxic amounts are lead, arsenic, and iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements. Presentation is variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables and management involves the use of chelating agents.
Last updated: Apr 27, 2025
Lead poisoning, also known as plumbism, may result from inhalation or ingestion of lead from:
Children:
Adults:
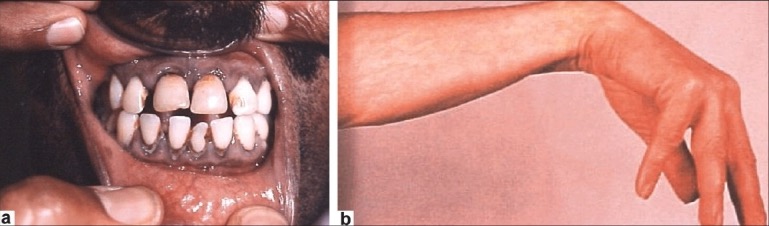
Clinical findings associated with lead poisoning:
a. lead line along the gingival border (Burton lines)
b. wrist drop as a consequence of peripheral neuropathy
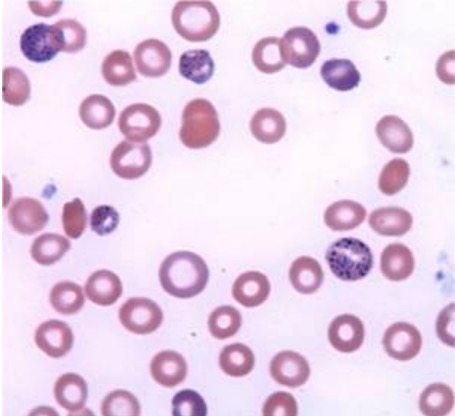
Wright-Giemsa–stained smear of peripheral blood: coarse basophilic stippling of the erythrocytes
Image: “Wright-Giemsa stained smear” by Yale Cancer Center, Section of Hematology, Yale University School of Medicine, New Haven, CT 06511, USA. License: CC BY 2.0Acute:
Chronic:
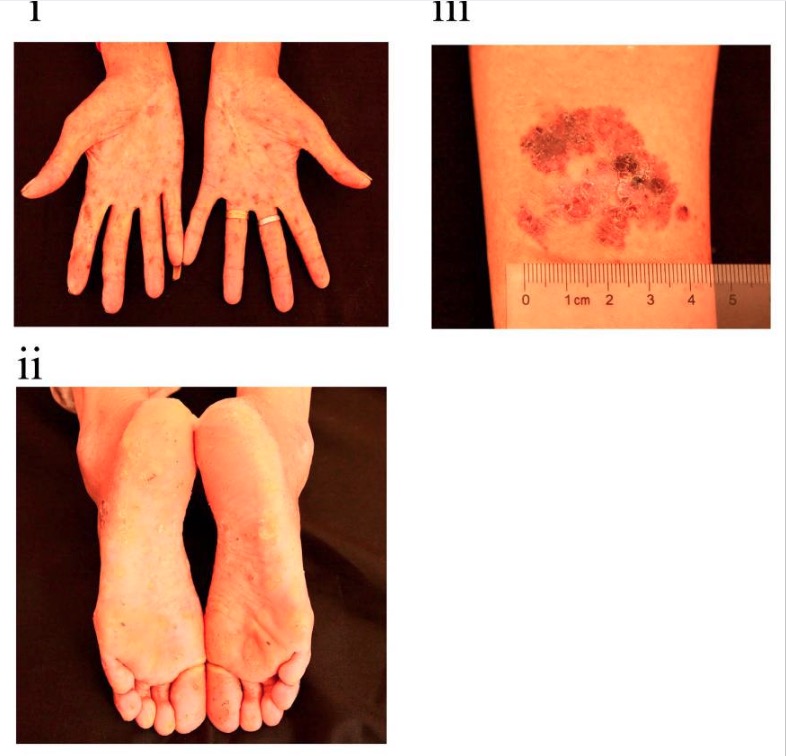
Cutaneous findings in chronic arsenic poisoning
Image: “Clinical appearance of the woman” by Research Center of Environment and Non-Communicable Disease, School of Public Health, China Medical University, No. 77 Puhe Road, Shenyang North New Area, Shenyang, Liaoning 110122, China. License: CC BY 4.0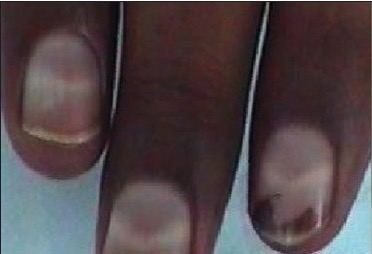
Photograph of a patient with arsenic poisoning showing Mees lines
Image: “Photograph of a patient with arsenic neuropathy” by Department of Neurology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India. License: CC BY 2.0, cropped by Lecturio.Iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements toxicity Toxicity Dosage Calculation is one of the leading causes of deaths by poisoning in children < 6 years.
Absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption of excessive quantities of ingested iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements can lead to: