Aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) (AR) is a cardiac condition characterized by the backflow of blood from the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy to the left ventricle during diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle. Aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) is associated with an abnormal aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy and/or aortic root stemming from multiple causes, commonly rheumatic heart disease Rheumatic Heart Disease Cardiac manifestation of systemic rheumatological conditions, such as rheumatic fever. Rheumatic heart disease can involve any part the heart, most often the heart valves and the endocardium. Rheumatic Fever as well as congenital and degenerative valvular disorders. Acute valvular insufficiency, which rapidly progresses to cardiogenic shock Cardiogenic shock Shock resulting from diminution of cardiac output in heart disease. Types of Shock, is an emergency requiring immediate aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy surgery. Chronic AR develops gradually, allowing the left ventricle to adapt to the increased stroke volume Stroke volume The amount of blood pumped out of the heart per beat, not to be confused with cardiac output (volume/time). It is calculated as the difference between the end-diastolic volume and the end-systolic volume. Cardiac Cycle. Thus, echocardiogram Echocardiogram Transposition of the Great Arteries shows left ventricular hypertrophy Ventricular Hypertrophy Tetralogy of Fallot and dilation along with valvular abnormalities. Eventually, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) occurs as the left ventricle is unable to handle the hemodynamic overload. Aortic valve replacement Aortic valve replacement Aortic Stenosis is the mainstay of treatment for AR with left ventricular dysfunction.
Last updated: May 16, 2024
Aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) (AR) or aortic insufficiency:
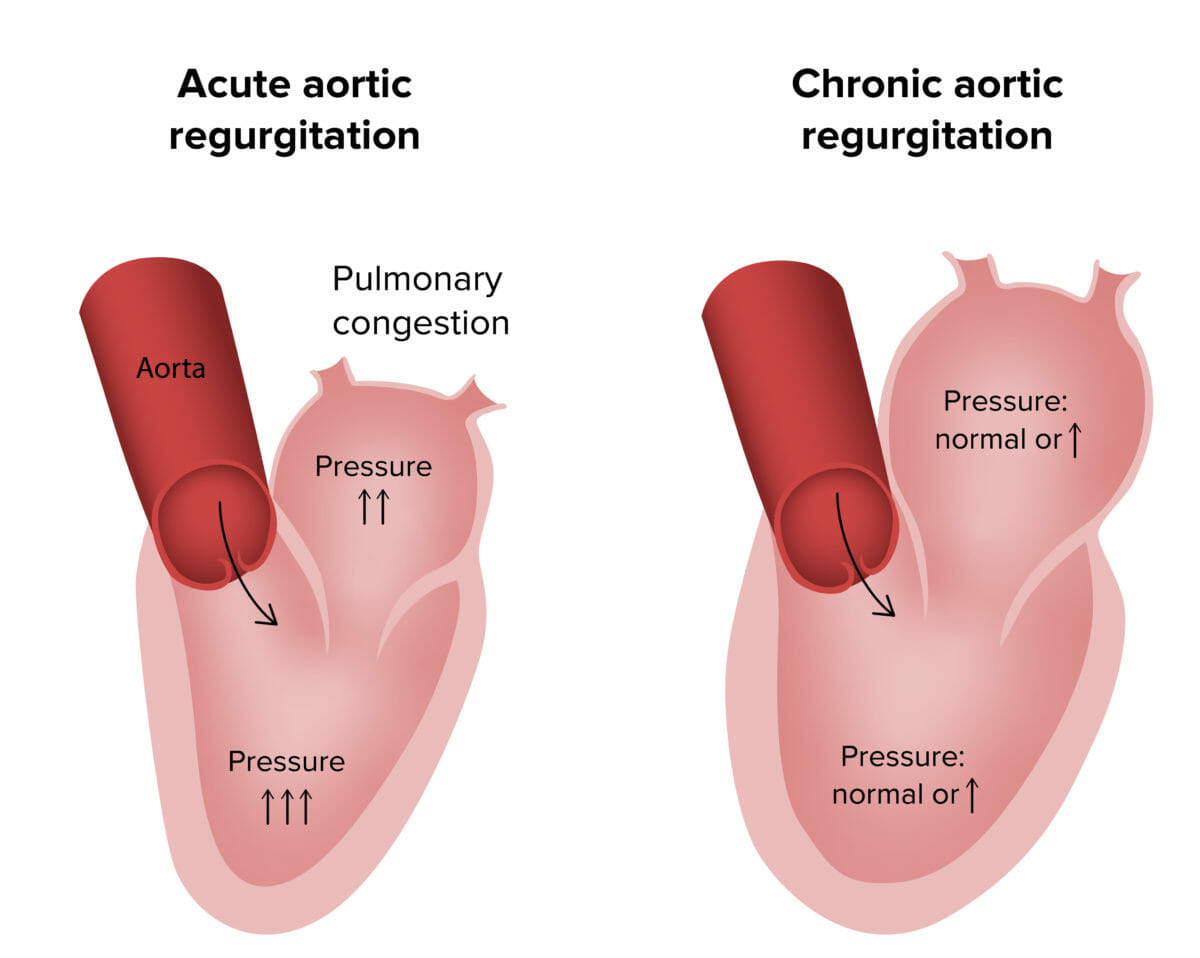
Pathophysiology of acute and chronic aortic regurgitation
Image by Lecturio.Symptoms:
Signs:
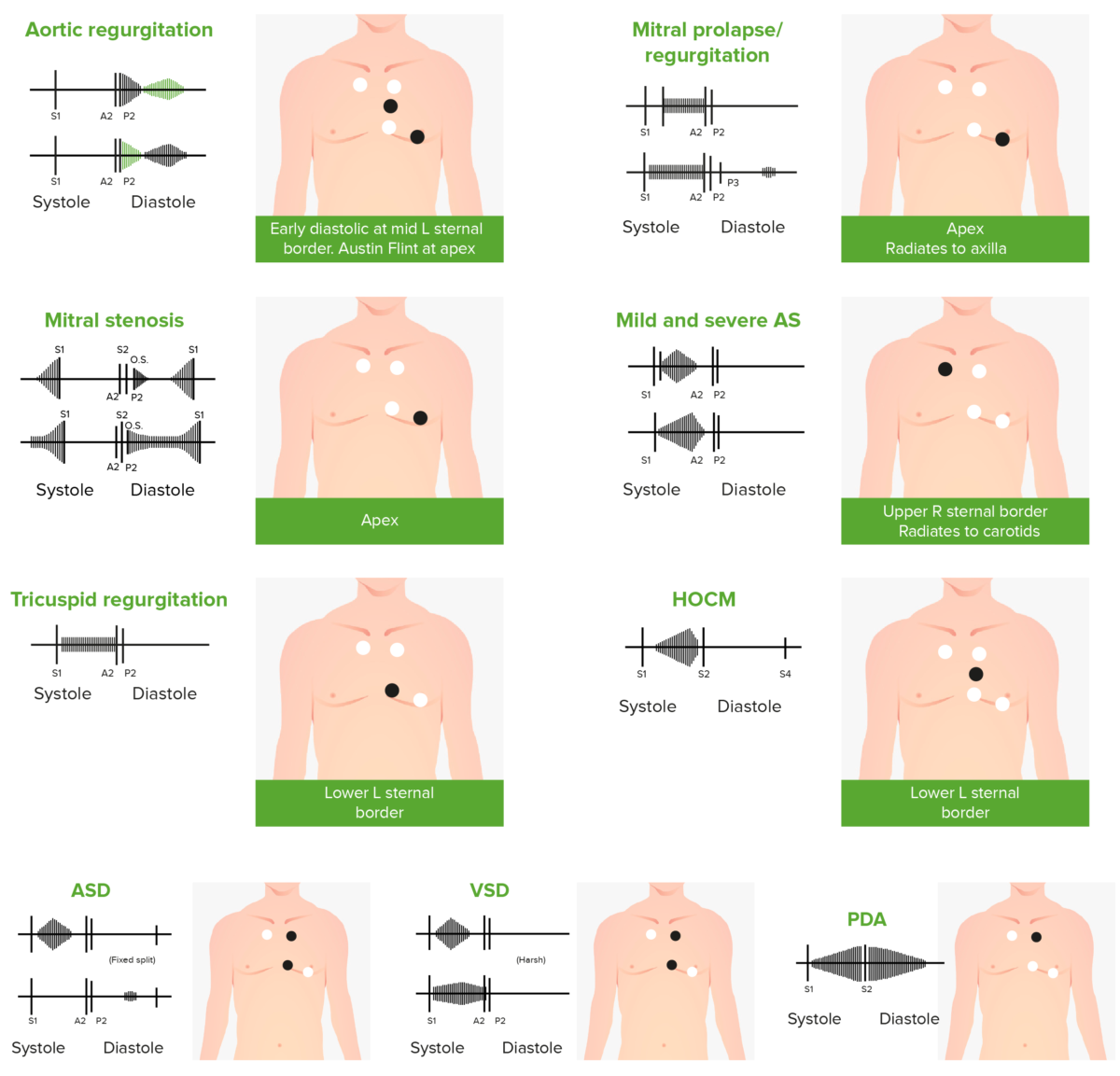
Phonocardiograms of abnormal heart sounds caused by the following cardiac defects:
aortic regurgitation, mitral valve prolapse, mitral stenosis (MS), aortic stenosis (AS), tricuspid regurgitation, hypertrophic obstructive cardiomyopathy (HOCM), atrial septal defect (ASD), ventricular septal defect (VSD), and patent ductus arteriosus (PDA)
Audio:
This audio clip is an example of aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD). It is characterized by a blowing, decrescendo murmur occurring right after S2 S2 Heart Sounds.
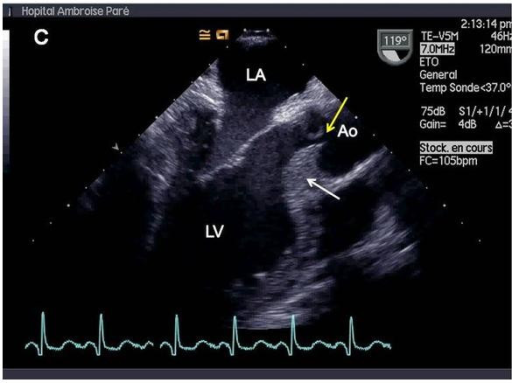
Transesophageal echocardiography showing septal hypertrophy (white arrow) and lack of central coaptation of aortic valve (yellow arrow), resulting in massive aortic regurgitation. Ao = aorta. LA = left atrium. LV = left ventricle.
Image: “Valvular involvement in ANCA-associated systemic vasculitis” by Lacoste C, Mansencal N, Ben M’rad M, Goulon-Goeau C, Cohen P, Guillevin L, Hanslik T. License: CC BY 2.0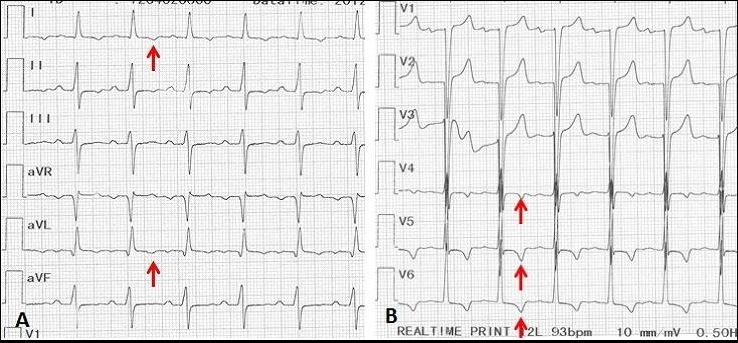
Electrocardiogram of a 70-year-old man with tertiary syphilis complicated by aortic regurgitation. The red arrows show apical-lateral sub-epicardial ischemia with inverted T wave.
Image: “Syphilitic aortic insufficiency ECG” by Yaméogo AA, Andonaba JB, Nikiéma Z, Zabsonré P. License: CC BY 2.0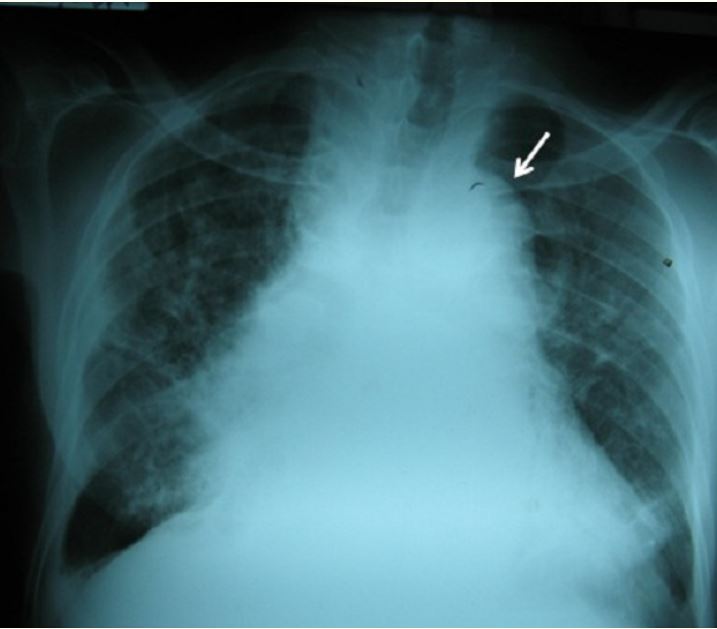
Syphilitic aortic insufficiency
Chest X-ray of a 70-year-old man patient with tertiary syphilis complicated with aortic regurgitation: aortic arch (arrow) and cardiomegaly with widening of the middle mediastinum.
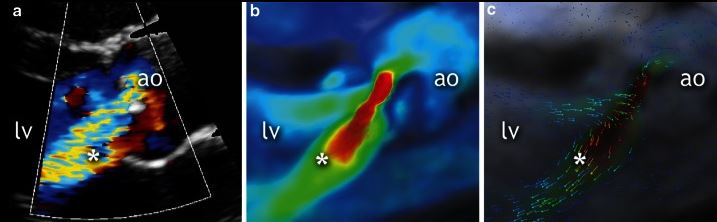
Echocardiography of a 19-year-old patient. Parasternal long axis view of aortic valve in diastole (a) shows moderate regurgitation (*). Corresponding four-dimensional flow cardiovascular magnetic resonance (4D flow CMR) images showing the moderate aortic regurgitation (b and c). *: regurgitant jet.
Image: “Qualitative grading of aortic regurgitation” by Chelu RG, et al. License: CC BY 4.0Differential diagnoses of AR include the following conditions: