A hordeolum is an acute infection affecting the meibomian, Zeis, or Moll glands of the eyelid. Stasis of the gland secretions predisposes the glands to bacterial infection. Staphylococcus aureus is the most common pathogen. The condition presents as a painful, localized, erythematous nodule in the anterior (external hordeolum) or posterior (internal hordeolum) lamella of the eyelid. A hordeolum usually resolves spontaneously and can be managed with warm compresses, massage, and lid hygiene. In certain cases of significant swelling, topical antibiotics with steroids may be needed. If a hordeolum does not resolve, the patient should be referred to ophthalmology for incision and drainage.
Last updated: May 17, 2024
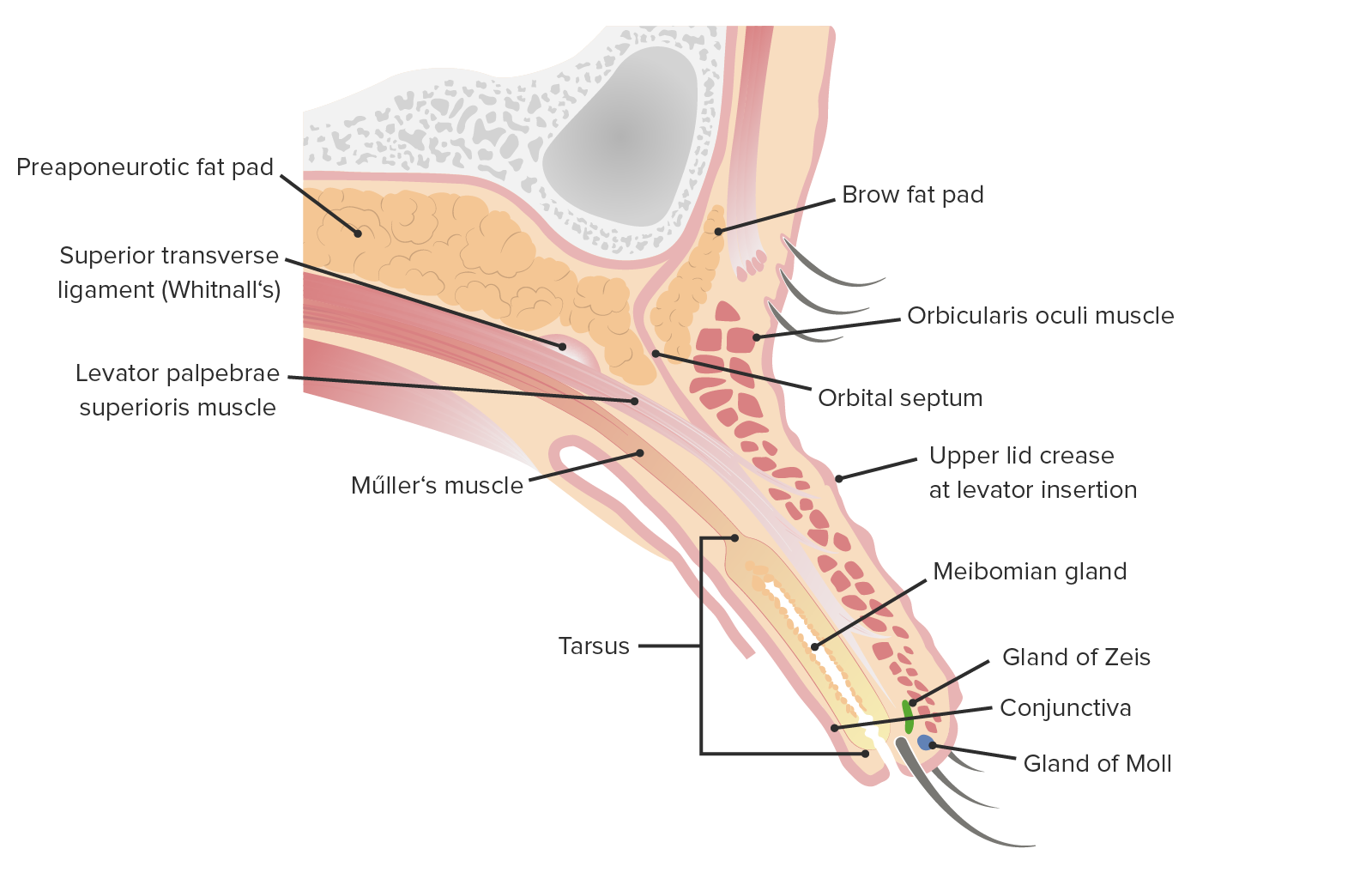
Sagittal cut of the upper eyelid
Image by Lecturio.| Name | Type | Opening location | Infection |
|---|---|---|---|
| Gland of Zeis | Sebaceous gland | Directly into the eyelash follicle | External hordeolum |
| Gland of Moll Gland of Moll Blepharitis | Modified sweat glands Sweat glands Sweat-producing structures that are embedded in the dermis. Each gland consists of a single tube, a coiled body, and a superficial duct. Soft Tissue Abscess | Between adjacent lashes | External hordeolum |
| Meibomian gland Meibomian Gland Chalazion | Modified sebaceous gland | Behind eyelashes | Internal hordeolum |
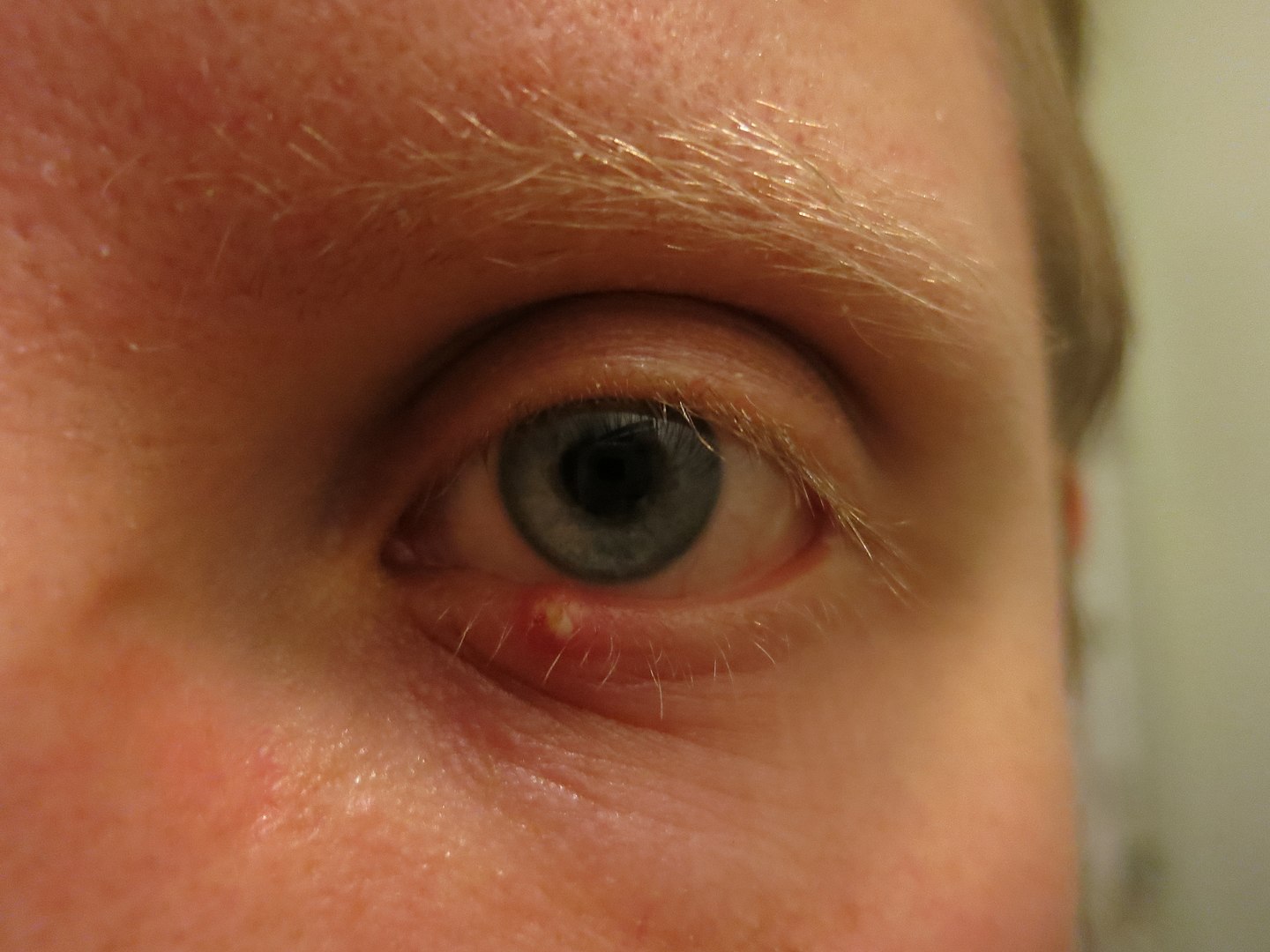
Man suffering from external hordeolum of the lower lid.
Image: “Stye” by Palosirkka. License: CC0 1.0
Upper eyelid hordeolum, illustrating a localized erythematous and swollen area.
Image: “Stye” by Andre Riemann. License: Public Domain
Photograph showing orbital cellulitis, a bacterial infection of the periocular tissues.
Image: “Orbital cellulitis” by Jonathan Trobe. License: CC BY 3.0Most hordeola resolve spontaneously, lasting up to 1–2 weeks.