Endophthalmitis is an inflammatory process of the inner layers of the eye, which may be either infectious or sterile Sterile Basic Procedures. Infectious endophthalmitis can lead to irreversible vision Vision Ophthalmic Exam loss if not treated quickly. Based on the entry mode of the infectious source, endophthalmitis is divided into endogenous and exogenous types. Exogenous endophthalmitis occurs via direct inoculation of infectious organisms during cataract Cataract Partial or complete opacity on or in the lens or capsule of one or both eyes, impairing vision or causing blindness. The many kinds of cataract are classified by their morphology (size, shape, location) or etiology (cause and time of occurrence). Neurofibromatosis Type 2 surgery, ocular trauma Ocular Trauma Cataracts in Children, or intravitreal injection. Endogenous endophthalmitis results from hematogenous seeding Hematogenous Seeding Septic Arthritis. Sterile Sterile Basic Procedures endophthalmitis may result from toxins or retained lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy material after an ocular operation. Clinical features vary depending on the type and course of the disease. Features may include decreased vision Vision Ophthalmic Exam, conjunctival injection, ocular pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, hypopyon Hypopyon Diseases of the Uvea, and corneal edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema. The diagnosis primarily depends on history and ophthalmological examination, and treatment is based upon the underlying cause. Sterile Sterile Basic Procedures endophthalmitis generally resolves spontaneously while infectious endophthalmitis is treated with antimicrobials (antibiotics or antifungals). Vitrectomy Vitrectomy Removal of the whole or part of the vitreous body in treating endophthalmitis, diabetic retinopathy, retinal detachment, intraocular foreign bodies, and some types of glaucoma. Retinal Detachment may be needed in severe disease.
Last updated: May 17, 2024
Endophthalmitis is an inflammatory process of the intraocular cavities (e.g., aqueous and/or vitreous humor Humor Defense Mechanisms) usually caused by bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology or fungi Fungi A kingdom of eukaryotic, heterotrophic organisms that live parasitically as saprobes, including mushrooms; yeasts; smuts, molds, etc. They reproduce either sexually or asexually, and have life cycles that range from simple to complex. Filamentous fungi, commonly known as molds, refer to those that grow as multicellular colonies. Mycology.
Exogenous:
Endogenous:
Normally, the ocular-blood barrier naturally resists invasive organisms.
Pathophysiology:
Risk factors:
Pathophysiology:
In unilateral cases, the right eye Right Eye Refractive Errors is twice as likely as the left eye Left Eye Refractive Errors to become infected.
Risk factors:
Acute:
Chronic:
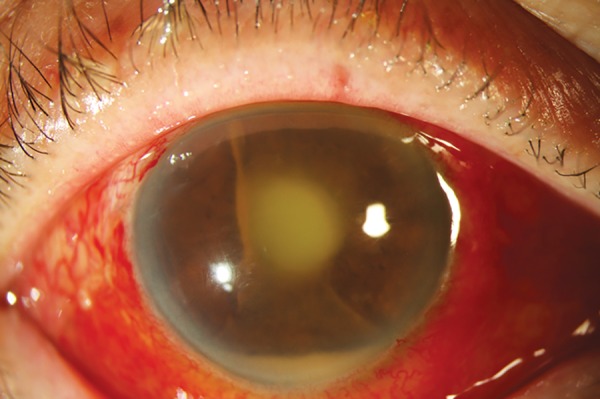
Hypopyon and track of pus with endophthalmitis associated with glaucoma shunt intraluminal stent exposure
Image: “Hypopyon and track of pus from tube at presentation with endophthalmitis” by Jaypee Brothers Medical Publishers (P) Ltd. License: CC BY 3.0Endophthalmitis diagnosis is based on clinical presentation with confirmation by laboratory testing of aqueous and/or vitreous humor Humor Defense Mechanisms.
Fundoscopy Fundoscopy Cranial Nerve Palsies:

A fundoscopic examination of a patient with endogenous fungal endophthalmitis demonstrates a yellow retinal lesion medial to the optic nerve.
Image: “Endogenous fungal endophthalmitis: risk factors, clinical features, and treatment outcomes in mold and yeast infections.” by Sridhar J, Flynn HW, Kuriyan AE, Miller D, Albini T. License: CC BY 2.0Slit-lamp examination Slit-Lamp Examination Blepharitis:
Diagnostic testing supports workup to search for the source of endogenous endophthalmitis:
Management depends on the underlying cause and outcome is extremely dependent on timely diagnosis and treatment.
Fungal:
Bacterial: