A cataract Cataract Partial or complete opacity on or in the lens or capsule of one or both eyes, impairing vision or causing blindness. The many kinds of cataract are classified by their morphology (size, shape, location) or etiology (cause and time of occurrence). Neurofibromatosis Type 2 is a condition defined as painless clouding or opacity Opacity Imaging of the Lungs and Pleura of the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy. Cataracts cause visual impairment, as the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy provides part of the eye’s refractive power. The condition is one of the most common causes of pediatric blindness Blindness The inability to see or the loss or absence of perception of visual stimuli. This condition may be the result of eye diseases; optic nerve diseases; optic chiasm diseases; or brain diseases affecting the visual pathways or occipital lobe. Retinopathy of Prematurity. Cataracts can be present from birth ( congenital Congenital Chorioretinitis) or can develop after infancy (acquired). Genetic mutations Genetic Mutations Carcinogenesis, systemic diseases, trauma, and medications can lead to cataract Cataract Partial or complete opacity on or in the lens or capsule of one or both eyes, impairing vision or causing blindness. The many kinds of cataract are classified by their morphology (size, shape, location) or etiology (cause and time of occurrence). Neurofibromatosis Type 2 development. Children present with an abnormal red reflex, leukocoria, or decreased visual acuity Visual Acuity Clarity or sharpness of ocular vision or the ability of the eye to see fine details. Visual acuity depends on the functions of retina, neuronal transmission, and the interpretative ability of the brain. Normal visual acuity is expressed as 20/20 indicating that one can see at 20 feet what should normally be seen at that distance. Visual acuity can also be influenced by brightness, color, and contrast. Ophthalmic Exam. An ophthalmologic examination reveals the morphology and location of the cataract Cataract Partial or complete opacity on or in the lens or capsule of one or both eyes, impairing vision or causing blindness. The many kinds of cataract are classified by their morphology (size, shape, location) or etiology (cause and time of occurrence). Neurofibromatosis Type 2. Management depends on age of presentation and visual defects. When opacity Opacity Imaging of the Lungs and Pleura is of a certain size or is causing visual impairment, strabismus Strabismus Strabismus is the misalignment of the eyes while fixating the gaze on an object. Strabismus can be idiopathic, but it may also be caused by cerebral palsy, uncorrected refractive errors, and extraocular muscle or cranial nerve dysfunction. Strabismus, and nystagmus Nystagmus Involuntary movements of the eye that are divided into two types, jerk and pendular. Jerk nystagmus has a slow phase in one direction followed by a corrective fast phase in the opposite direction, and is usually caused by central or peripheral vestibular dysfunction. Pendular nystagmus features oscillations that are of equal velocity in both directions and this condition is often associated with visual loss early in life. Albinism, cataract Cataract Partial or complete opacity on or in the lens or capsule of one or both eyes, impairing vision or causing blindness. The many kinds of cataract are classified by their morphology (size, shape, location) or etiology (cause and time of occurrence). Neurofibromatosis Type 2 surgery is recommended.
Last updated: May 17, 2024
A cataract Cataract Partial or complete opacity on or in the lens or capsule of one or both eyes, impairing vision or causing blindness. The many kinds of cataract are classified by their morphology (size, shape, location) or etiology (cause and time of occurrence). Neurofibromatosis Type 2 is a painless opacity Opacity Imaging of the Lungs and Pleura of the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy that disrupts the light projecting onto the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy, resulting in a clouding of vision Vision Ophthalmic Exam. Cataracts can cause partial or total blindness Blindness The inability to see or the loss or absence of perception of visual stimuli. This condition may be the result of eye diseases; optic nerve diseases; optic chiasm diseases; or brain diseases affecting the visual pathways or occipital lobe. Retinopathy of Prematurity.
Lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy:
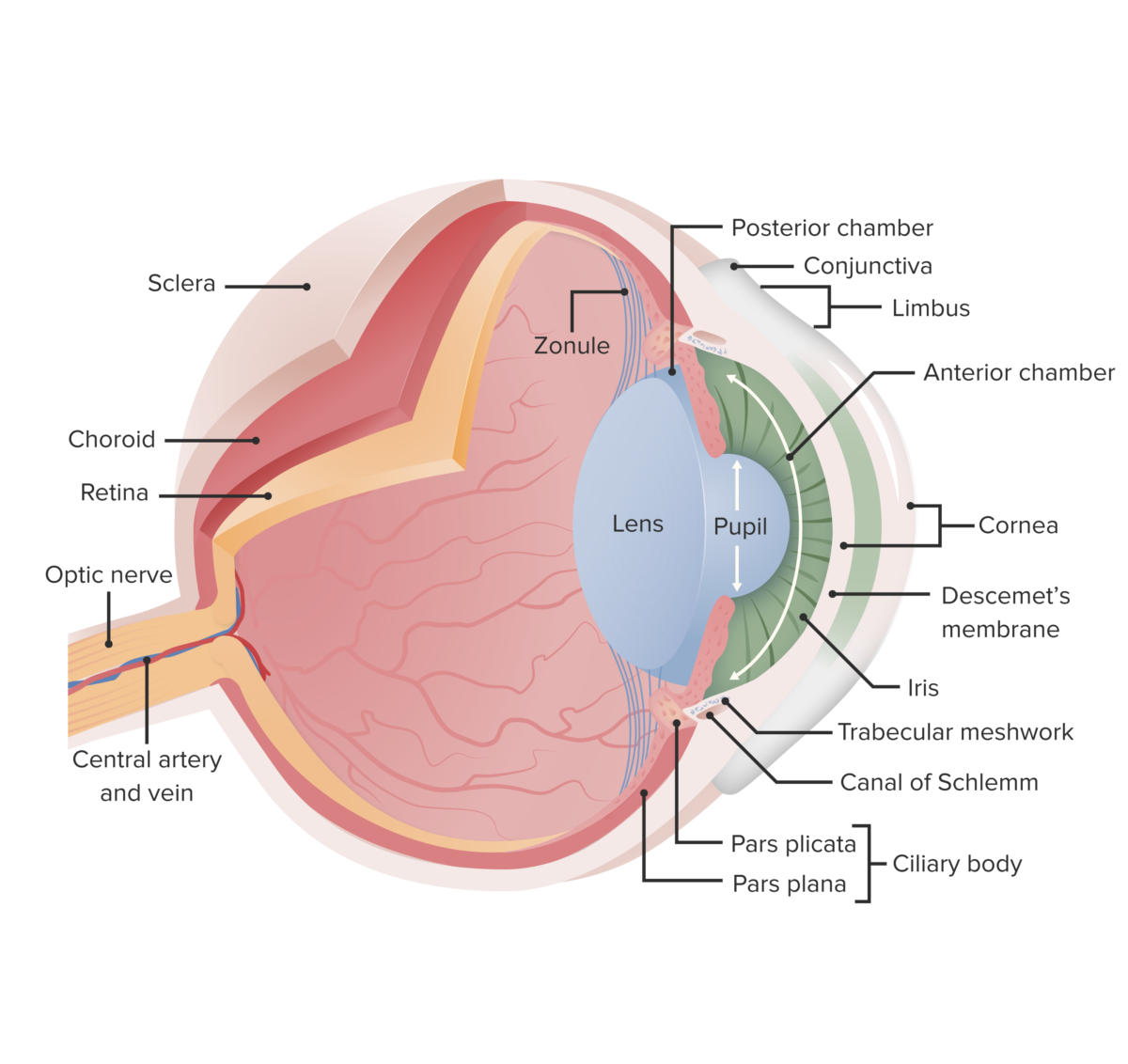
This image displays the essential anatomy of the eye. In cataracts, there is clouding of the lens, which opacifies the light as it projects to the retina; this leads to reduced vision, particularly at night when light levels are low.
Image by Lecturio.
Child who developed a left eye cataract after sustaining a lightning injury
Image: “A dense left cataract” by Division of Ophthalmology, Red Cross War Memorial Children’s Hospital and the University of Cape Town, Klipfontein Road, Rondebosch, Cape Town 7700, South Africa. License: CC BY 3.0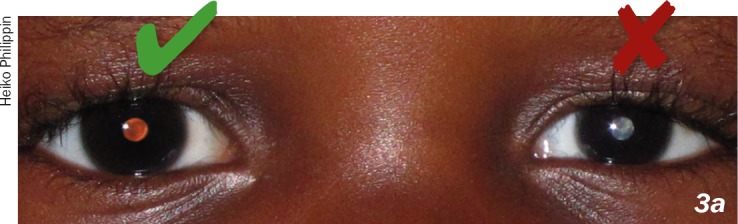
Red reflex is a red-orange reflection from the posterior part of the eye. The absence of this color is abnormal and could indicate a serious condition. The child in this image has a cataract in the left eye.
Image: “How to test for the red reflex” by US National Library of Medicine. License: CC BY 2.0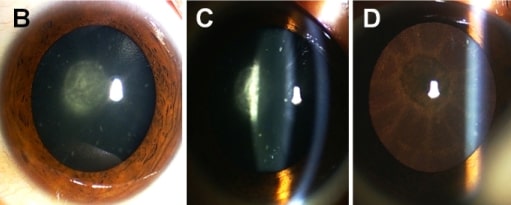
Congenital cataract: Images (B, C, D) of a dilated eye show a posterior subcapsular cataract.
Image: “Clinical features of the family” by Eye Center of the 2nd Affiliated Hospital, Medical College of Zhejiang University, Hangzhou, China. License: CC BY 3.0, edited by Lecturio.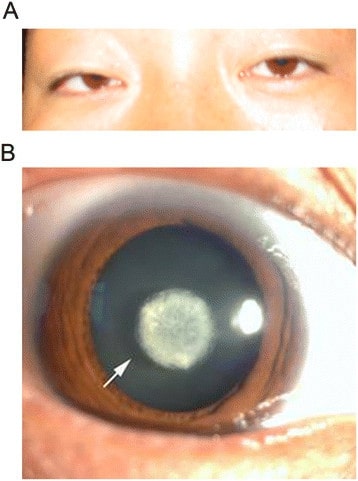
A. Undilated eye examination of a patient with congenital cataract.
B. Dilated examination showed a nuclear cataract with normal cornea and iris.