Internuclear ophthalmoplegia Ophthalmoplegia Paralysis of one or more of the ocular muscles due to disorders of the eye muscles, neuromuscular junction, supporting soft tissue, tendons, or innervation to the muscles. Orbital and Preseptal Cellulitis (INO) is an ocular movement disorder that affects the conjugate horizontal gaze, meaning the eyes are incapable of moving in a simultaneous and coordinated manner on the horizontal plane. This disorder is usually caused by a lesion in the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification stem involving the medial longitudinal fasciculus (MLF) and is characterized by impaired adduction Adduction Examination of the Upper Limbs ipsilateral to the MLF lesion and abduction Abduction Examination of the Upper Limbs nystagmus Nystagmus Involuntary movements of the eye that are divided into two types, jerk and pendular. Jerk nystagmus has a slow phase in one direction followed by a corrective fast phase in the opposite direction, and is usually caused by central or peripheral vestibular dysfunction. Pendular nystagmus features oscillations that are of equal velocity in both directions and this condition is often associated with visual loss early in life. Albinism contralateral to the MLF lesion. Internuclear ophthalmoplegia Ophthalmoplegia Paralysis of one or more of the ocular muscles due to disorders of the eye muscles, neuromuscular junction, supporting soft tissue, tendons, or innervation to the muscles. Orbital and Preseptal Cellulitis is a clinical diagnosis. However, investigations involving neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant, especially MRI, help establish the etiology. Management of INO varies depending on the cause. The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas mainly depends on the etiology. For instance, trauma patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship do not have a very favorable prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas, whereas patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ischemic and demyelinating causes have a favorable recovery.
Last updated: Jun 17, 2025
Internuclear ophthalmoplegia Ophthalmoplegia Paralysis of one or more of the ocular muscles due to disorders of the eye muscles, neuromuscular junction, supporting soft tissue, tendons, or innervation to the muscles. Orbital and Preseptal Cellulitis (INO) is an ocular movement disorder that is due to a lesion of the medial longitudinal fasciculus (MLF), mainly in the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification stem tegmentum (dorsomedial pons Pons The front part of the hindbrain (rhombencephalon) that lies between the medulla and the midbrain (mesencephalon) ventral to the cerebellum. It is composed of two parts, the dorsal and the ventral. The pons serves as a relay station for neural pathways between the cerebellum to the cerebrum. Brain Stem: Anatomy or the midbrain Midbrain The middle of the three primitive cerebral vesicles of the embryonic brain. Without further subdivision, midbrain develops into a short, constricted portion connecting the pons and the diencephalon. Midbrain contains two major parts, the dorsal tectum mesencephali and the ventral tegmentum mesencephali, housing components of auditory, visual, and other sensorimotor systems. Brain Stem: Anatomy).
Internuclear ophthalmoplegia Ophthalmoplegia Paralysis of one or more of the ocular muscles due to disorders of the eye muscles, neuromuscular junction, supporting soft tissue, tendons, or innervation to the muscles. Orbital and Preseptal Cellulitis is mainly due to autoimmune demyelinating disorder and infarction.
The MLF has a very important role in controlling the direction of eye movements.
Internuclear ophthalmoplegia Ophthalmoplegia Paralysis of one or more of the ocular muscles due to disorders of the eye muscles, neuromuscular junction, supporting soft tissue, tendons, or innervation to the muscles. Orbital and Preseptal Cellulitis occurs because of a lesion or dysfunction of the MLF, characterized by:
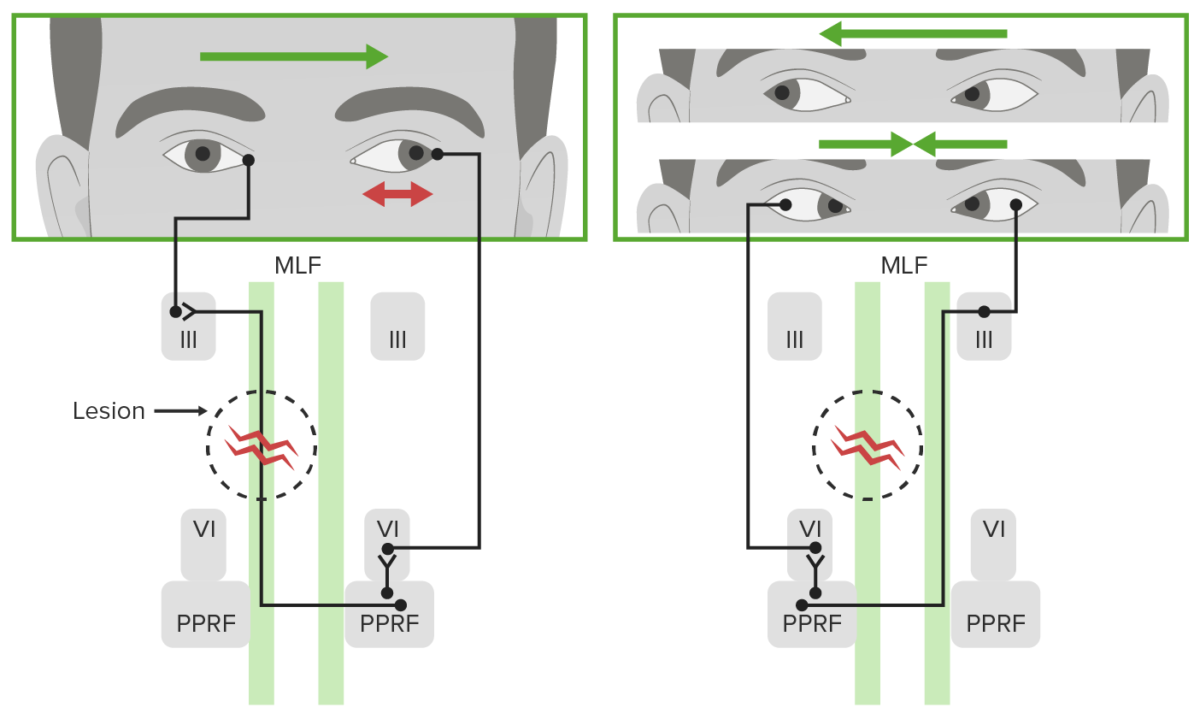
Defect of horizontal gaze in unilateral internuclear ophthalmoplegia:
Note the ipsilateral defective adduction with leftward gaze and contralateral abducting nystagmus (red double arrow in top left image). Normal rightward gaze and convergence would also be seen (right image).
MLF: medial longitudinal fasciculus
III: nucleus of the oculomotor cranial nerve III
VI: nucleus of the abducens cranial nerve VI
PPRF: paramedian pontine reticular formation
The presentation of individuals with INO can vary but includes:
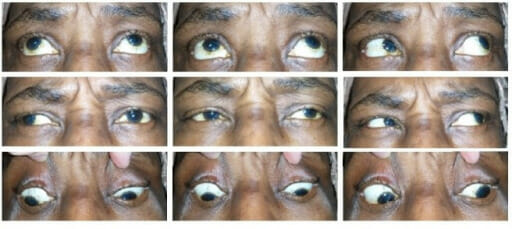
An individual with left internuclear ophtalmoplegia:
Notice that adduction of the left eye is impaired (left column of images) due to a unilateral defect of the medial longitudinal fasciculus.
Management depends on the underlying cause, and clinical improvement can vary.