Listeria spp. are motile, flagellated, gram-positive Gram-Positive Penicillins, facultative intracellular Facultative intracellular Yersinia spp./Yersiniosis bacilli Bacilli Shigella. The major pathogenic species is Listeria monocytogenes. Listeria are part of the normal gastrointestinal flora of domestic mammals and poultry and are transmitted to humans through the ingestion of contaminated food, especially unpasteurized dairy products. Listeria can also infect the fetus in utero or neonates during vaginal birth. Healthy individuals exposed to L. monocytogenes usually do not become ill if the inoculum is small, or may develop only self-limiting Self-Limiting Meningitis in Children gastroenteritis Gastroenteritis Gastroenteritis is inflammation of the stomach and intestines, commonly caused by infections from bacteria, viruses, or parasites. Transmission may be foodborne, fecal-oral, or through animal contact. Common clinical features include abdominal pain, diarrhea, vomiting, fever, and dehydration. Gastroenteritis. Immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis or elderly individuals, neonates, and pregnant women can develop invasive disease, including meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis and bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides. Treatment of invasive listeriosis includes ampicillin Ampicillin Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic. Penicillins and gentamicin Gentamicin Aminoglycosides.
Last updated: Feb 28, 2023
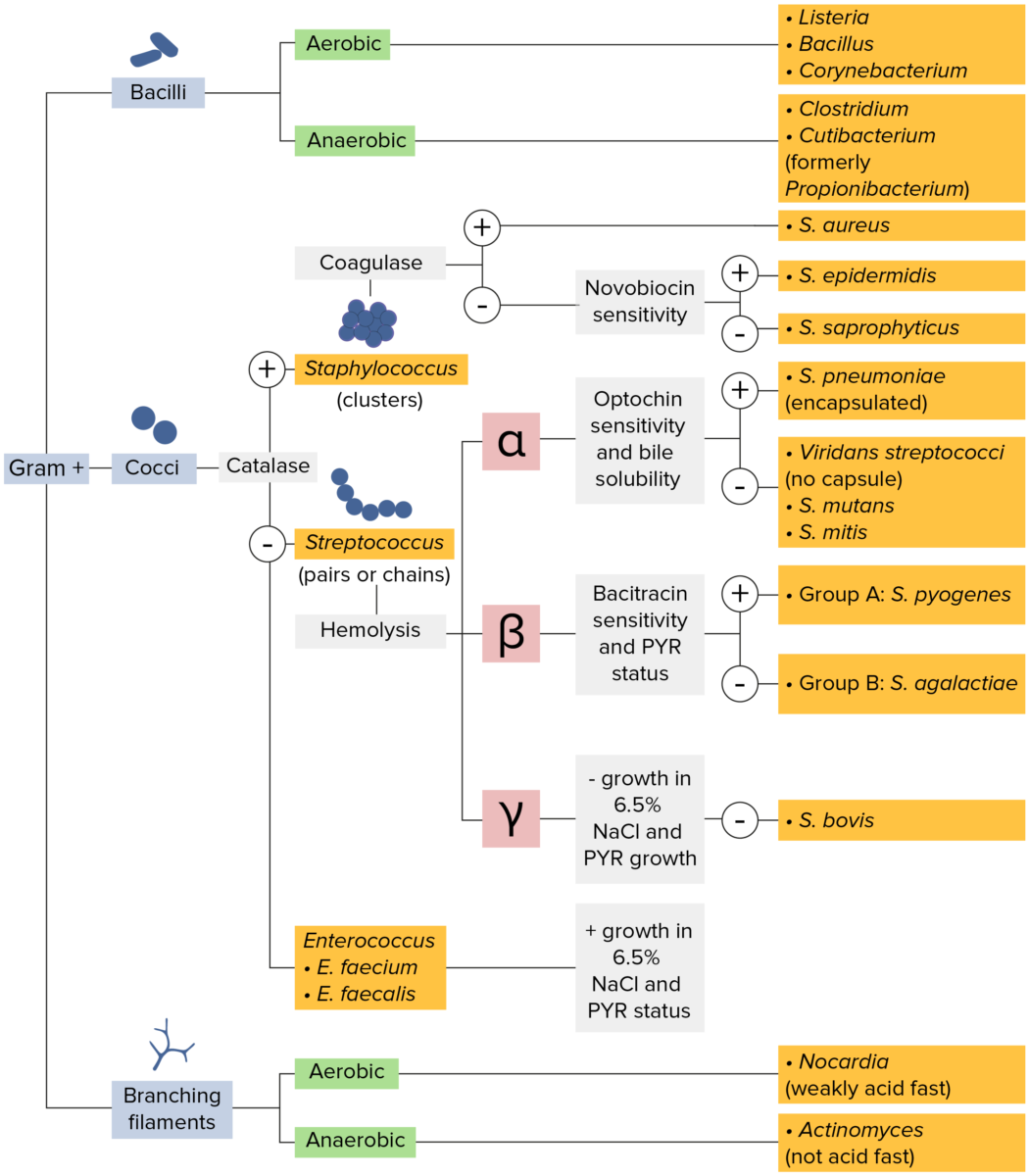
Gram-positive bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thick layer of peptidoglycan retain the crystal violet stain utilized in Gram staining but are not affected by the safranin counterstain. These bacteria appear as purple-blue on the stain, indicating that they are gram positive. The bacteria can be further classified according to morphology (branching filaments, bacilli, and cocci in clusters or chains) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The cocci can also be further identified. Staphylococci can be narrowed down on the basis of the presence of the enzyme coagulase and on their sensitivity to the antibiotic novobiocin. Streptococci are grown on blood agar and classified on the basis of which form of hemolysis they employ (α, β, or γ). Streptococci are further narrowed on the basis of their response to the pyrrolidonyl-β-naphthylamide (PYR) test, their sensitivity to specific antimicrobials (optochin and bacitracin), and their ability to grow on sodium chloride (NaCl) media.
General characteristics of Listeria species include:
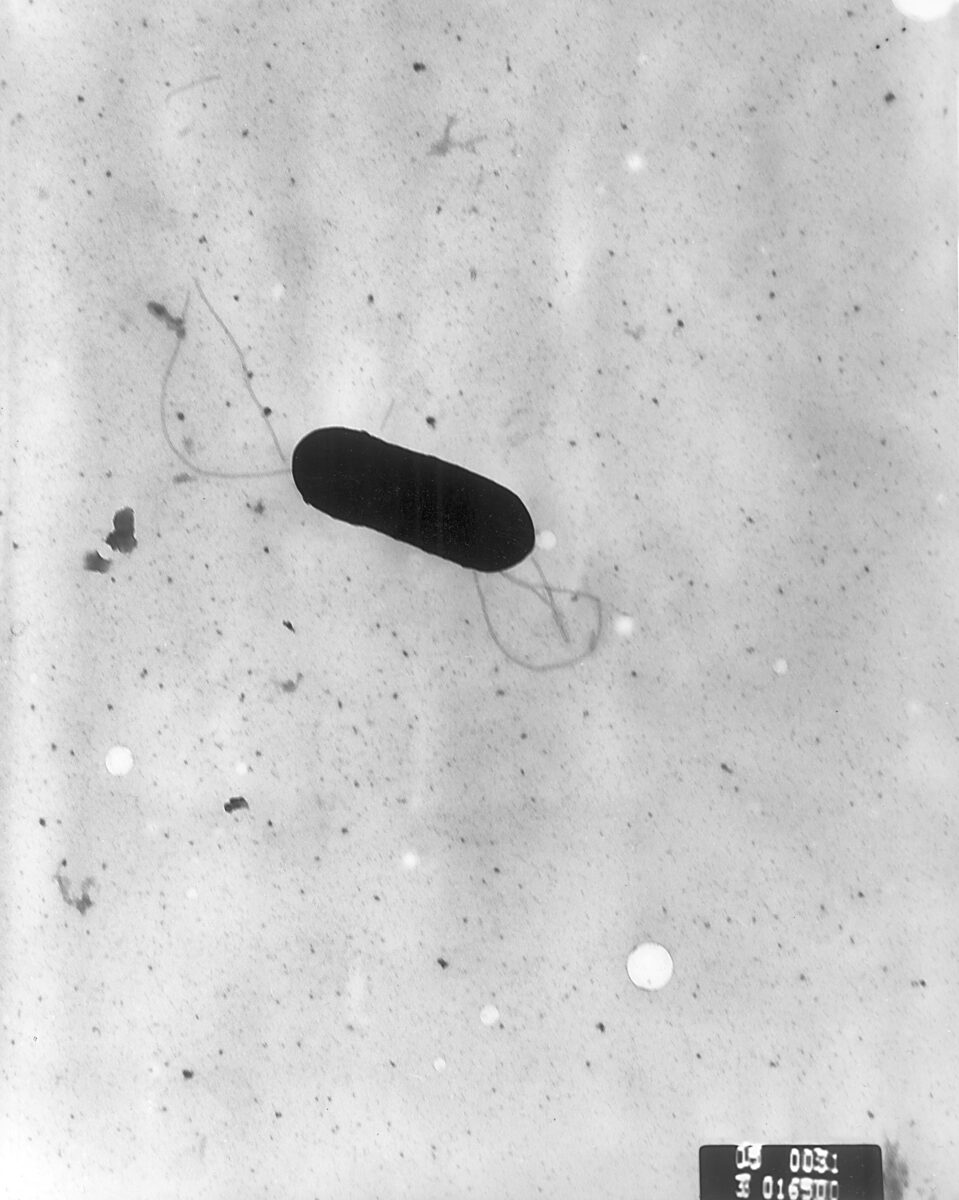
Scanning electron micrograph of Listeria monocytogenes bacterium
Image: “2287” by Elizabeth White. License: Public Domain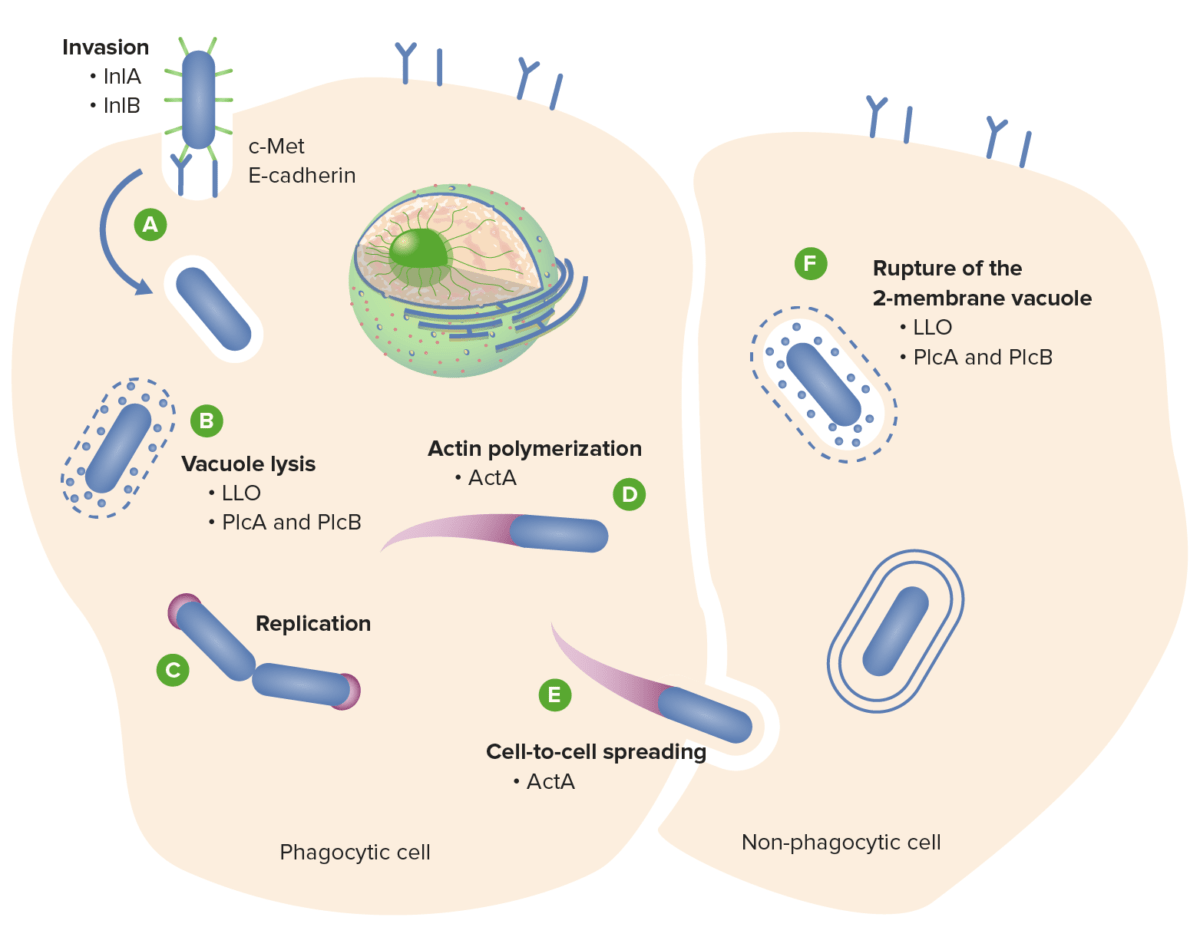
Listeria monocytogenes cycle of infection:
(A) L. monocytogenes invades the host cell via the interaction of surface internalins A and B (InlA and InlB) with the host cell surface receptors E-cadherin and c-Met, respectively.
(B) Listeria escapes from the phagosome via the action of the toxins LLO, PlcA, and PlcB.
(D) Listeria replicates in the cytosol and propels to the cell surface via actin polymerization, (E) promoting cell-to-cell spread.
(F) Rupture of the 2-membrane vacuole is also mediated by the LLO and phospholipase toxins.
InIA: internalin A
InlB: internalin B
LLO: listeriolysin O
PlcA: phospholipase A
PlcB: phospholipase B
ActA: actin-assembly inducing protein A
An invasive form of the disease can develop in certain populations:
Depending on the size of the inoculum and the state of the immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs of the individual, L. monocytogenes infection can present in various ways.
| Type of clinical presentation | Clinical features |
|---|---|
| Self-limited gastroenteritis Gastroenteritis Gastroenteritis is inflammation of the stomach and intestines, commonly caused by infections from bacteria, viruses, or parasites. Transmission may be foodborne, fecal-oral, or through animal contact. Common clinical features include abdominal pain, diarrhea, vomiting, fever, and dehydration. Gastroenteritis |
Presents in healthy individuals < 48 hours after ingesting large inoculum in contaminated food:
|
| Bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides/septicemia | Presents in
immunocompromised
immunocompromised
A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation.
Gastroenteritis or elderly individuals:
|
| CNS infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease | Presents in
immunocompromised
immunocompromised
A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation.
Gastroenteritis or elderly individuals:
|
| Infection in pregnant women |
|
| Infection in fetuses/neonates ( congenital Congenital Chorioretinitis listeriosis) |
|
The differential diagnosis of listeriosis includes all causes of meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis or septicemia.
| Bacterial meningitis Bacterial meningitis Bacterial infections of the leptomeninges and subarachnoid space, frequently involving the cerebral cortex, cranial nerves, cerebral blood vessels, spinal cord, and nerve roots. Meningitis | Viral meningitis Viral meningitis Viral infections of the leptomeninges and subarachnoid space. Togaviridae infections; flaviviridae infections; rubella; bunyaviridae infections; orbivirus infections; picornaviridae infections; orthomyxoviridae infections; rhabdoviridae infections; arenaviridae infections; herpesviridae infections; adenoviridae infections; JC virus infections; and retroviridae infections may cause this form of meningitis. Clinical manifestations include fever, headache, neck pain, vomiting, photophobia, and signs of meningeal irritation. Meningitis | Fungal/tuberculous ( TB TB Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis complex bacteria. The bacteria usually attack the lungs but can also damage other parts of the body. Approximately 30% of people around the world are infected with this pathogen, with the majority harboring a latent infection. Tuberculosis spreads through the air when a person with active pulmonary infection coughs or sneezes. Tuberculosis) meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis | |
|---|---|---|---|
| Glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance | ↓ | Normal | ↓ |
| Protein | ↑ | Normal | ↑ |
| WBC | ↑ Polymorphonuclear leukocytes Leukocytes White blood cells. These include granular leukocytes (basophils; eosinophils; and neutrophils) as well as non-granular leukocytes (lymphocytes and monocytes). White Myeloid Cells: Histology (PMNs) | ↑ Lymphocytes Lymphocytes Lymphocytes are heterogeneous WBCs involved in immune response. Lymphocytes develop from the bone marrow, starting from hematopoietic stem cells (HSCs) and progressing to common lymphoid progenitors (CLPs). B and T lymphocytes and natural killer (NK) cells arise from the lineage. Lymphocytes: Histology | ↑↑ Lymphocytes Lymphocytes Lymphocytes are heterogeneous WBCs involved in immune response. Lymphocytes develop from the bone marrow, starting from hematopoietic stem cells (HSCs) and progressing to common lymphoid progenitors (CLPs). B and T lymphocytes and natural killer (NK) cells arise from the lineage. Lymphocytes: Histology |
| Opening pressure | ↑ | Normal | ↑↑ |
| Color | Turbid | Clear or bloody | Clear or opaque |