Staphylococcal scalded skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions syndrome (SSSS), also known as Ritter disease and staphylococcal epidermal necrolysis, is a toxin-mediated condition caused by Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess. The exfoliative toxin produced disseminates and cleaves desmoglein Desmoglein A group of desmosomal cadherins with cytoplasmic tails that resemble those of classical cadherins. The Cell: Cell Junctions 1 in the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions, causing separation and detachment of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. SSSS most commonly affects young children. Prodromal symptoms precede diffuse cutaneous erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion, tenderness, bullae Bullae Erythema Multiforme formation, and superficial desquamation. The mucous membranes are spared. The diagnosis is made clinically and can be confirmed with culture data (targeting possible primary infection Primary infection Herpes Simplex Virus 1 and 2 sites) and biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. However, cultures of bullae Bullae Erythema Multiforme are not useful. Antibiotics and supportive care should be initiated as soon as the diagnosis is suspected.
Last updated: May 17, 2024
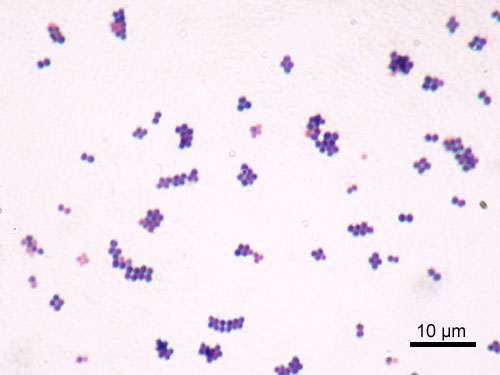
Microscopic image of Staphylococcus aureus
Image: “Staphylococcus aureus Gram” by Y Tambe. License: CC BY-SA 3.0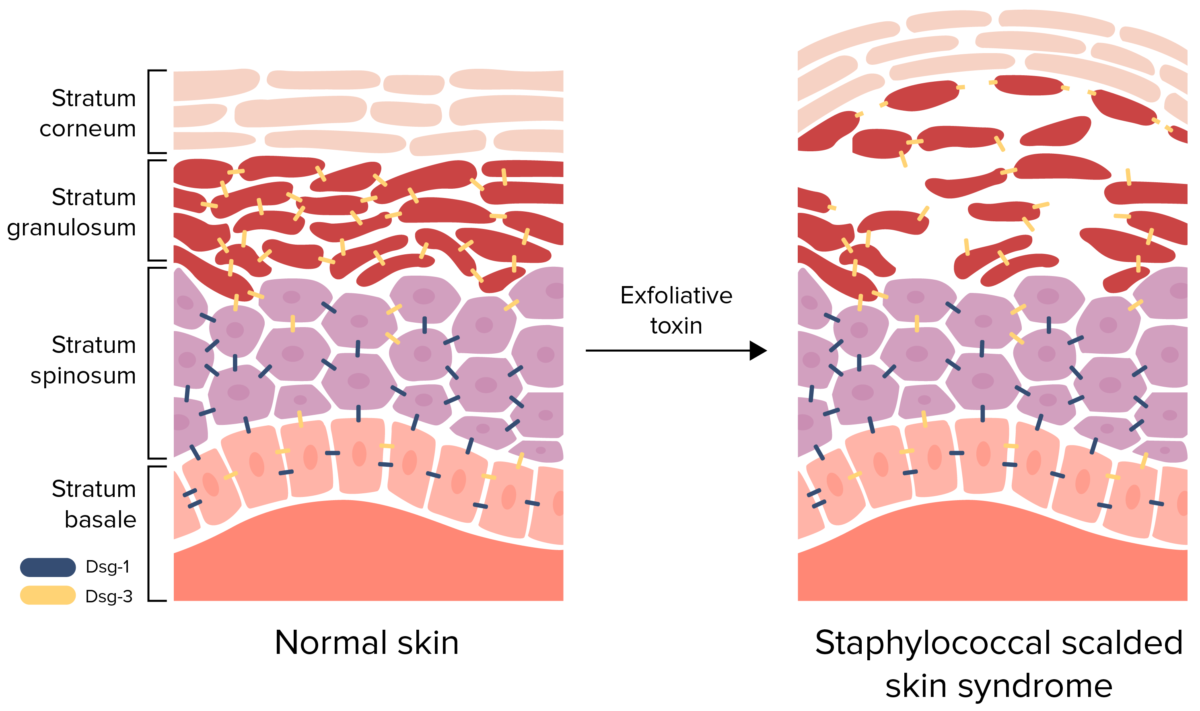
Pathophysiology of staphylococcal scalded skin syndrome:
Exfoliative toxin cleaves desmoglein (Dsg) 1, disrupting the cell-to-cell adhesion of the stratum granulosum. This detachment of the superficial epidermis causes bullae formation and desquamation.

Staphylococcal scalded skin syndrome in a newborn:
This image shows diffuse erythema, bullae formation, and skin peeling.

Cutaneous manifestations of SSSS:
Skin peeling and erythema is noted over the thigh.

Cutaneous manifestations of SSSS:
Erythema, skin peeling, and crusting on the face
Management of SSSS includes aggressive treatment of primary infection Primary infection Herpes Simplex Virus 1 and 2 and supportive care.
| Number | Other names for the disease | Etiology | Description |
|---|---|---|---|
| 1st disease 1st disease Measles (also known as rubeola) is caused by a single-stranded, linear, negative-sense RNA virus of the family Paramyxoviridae. It is highly contagious and spreads by respiratory droplets or direct-contact transmission from an infected person. Typically a disease of childhood, measles classically starts with cough, coryza, and conjunctivitis, followed by a maculopapular rash. Measles Virus |
|
Measles Measles Measles (also known as rubeola) is caused by a single-stranded, linear, negative-sense RNA virus of the family Paramyxoviridae. It is highly contagious and spreads by respiratory droplets or direct-contact transmission from an infected person. Typically a disease of childhood, measles classically starts with cough, coryza, and conjunctivitis, followed by a maculopapular rash. Measles Virus morbillivirus Morbillivirus A genus of the family paramyxoviridae (subfamily paramyxovirinae) where the virions of most members have hemagglutinin but not neuraminidase activity. All members produce both cytoplasmic and intranuclear inclusion bodies. Measles virus is the type species. Measles Virus |
|
| 2nd disease |
|
Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pyogenes |
|
| 3rd disease 3rd disease An acute infectious disease caused by the rubella virus. The virus enters the respiratory tract via airborne droplet and spreads to the lymphatic system. Rubella Virus |
|
Rubella Rubella An acute infectious disease caused by the rubella virus. The virus enters the respiratory tract via airborne droplet and spreads to the lymphatic system. Rubella Virus virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology |
|
| 4th disease |
|
Due to Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess strains that make epidermolytic (exfoliative) toxin |
|
| 5th disease | Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion infectiosum | Erythrovirus or parvovirus B19 Parvovirus B19 Primate erythroparvovirus 1 (generally referred to as parvovirus B19, B19 virus, or sometimes erythrovirus B19) ranks among the smallest DNA viruses. Parvovirus B19 is of the family Parvoviridae and genus Erythrovirus. In immunocompetent humans, parvovirus B19 classically results in erythema infectiosum (5th disease) or “slapped cheek syndrome.” Parvovirus B19 (primate erythroparvovirus Erythroparvovirus Parvovirus B19 1) |
|
| 6th disease |
|
HHV-6B or HHV-7 HHV-7 Human herpesvirus (HHV)-6 and HHV-7 are similar double-stranded DNA viruses belonging to the Herpesviridae family. Human herpesviruses are ubiquitous and infections are commonly contracted during childhood. Human Herpesvirus 6 and 7 |
|