Advertisement
Advertisement
Advertisement
Advertisement
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome or infantile polyarteritis, is a medium-sized necrotizing vasculitis that predominantly affects children < 5 years of age. The etiology is currently unknown, but it is postulated to involve a combination of environmental and genetic factors. Multiple systems are involved, but the disease displays a predilection for the coronary arteries, which may lead to serious complications. The diagnosis can be made based on clinical criteria. In cases where incomplete KD may be suspected, the diagnosis may be supported by laboratory studies and echocardiography. Management involves intravenous immunoglobulin and high-dose aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs). Follow-up requires serial echocardiograms to monitor for coronary artery Coronary Artery Truncus Arteriosus aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms.
Last updated: May 16, 2024
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
The etiology of Kawasaki disease (KD) is unknown. There are several theories:
Immunologic response theory:
Infection theory:
Genetic predisposition theory:
Environmental factors theory:
Kawasaki disease is a systemic, inflammatory illness that affects medium-sized arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, especially the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology.

Edema and a polymorphous rash on the hands and feet in a 3-month-old patient with KD
Image: “Patient’s limbs” by Unit of Broncho-Pneumology and Cystic Fibrosis, Department of Medical and Pediatric Science, University of Catania, Via Santa Sofia 78, Catania 95123, Italy. License: CC BY 2.0
Lip fissuring alongside a polymorphous rash in KD
Image: “Patient’s face” by Unit of Broncho-Pneumology and Cystic Fibrosis, Department of Medical and Pediatric Science, University of Catania, Via Santa Sofia 78, Catania 95123, Italy. License: CC BY 2.0
Bilateral, non-exudative conjunctivitis observed in a patient with KD
Image: “Kawasaki symptoms A” by Dong Soo Kim. License: CC BY 2.0
Desquamation of the fingertips observed in KD at 10–14 days
Image: “Desquamation of the fingers” by Dong Soo Kim. License: CC BY 2.0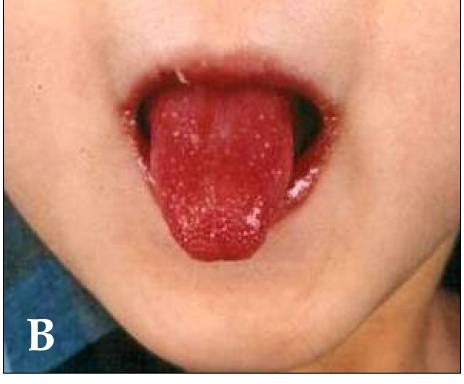
Strawberry tongue and bright-red, swollen lips with vertical cracking and bleeding in a patient with KD
Image: “Kawasaki disease” by Dong Soo Kim. License: CC BY 2.0| System | Manifestations |
|---|---|
| Gastrointestinal | Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea, abdominal pain Abdominal Pain Acute Abdomen, vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy dysfunction, pancreatitis Pancreatitis Inflammation of the pancreas. Pancreatitis is classified as acute unless there are computed tomographic or endoscopic retrograde cholangiopancreatographic findings of chronic pancreatitis. The two most common forms of acute pancreatitis are alcoholic pancreatitis and gallstone pancreatitis. Acute Pancreatitis, hydrops Hydrops Cholecystitis gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy, ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites, splenic infarction Splenic Infarction Insufficiency of arterial or venous blood supply to the spleen due to emboli, thrombi, vascular torsion, or pressure that produces a macroscopic area of necrosis. . Imaging of the Spleen |
| Musculoskeletal | Polyarthritis Polyarthritis Rheumatoid Arthritis, arthralgia Arthralgia Pain in the joint. Rheumatic Fever |
| Cardiovascular system | Myocarditis Myocarditis Myocarditis is an inflammatory disease of the myocardium, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation and myocyte injury, most often leading to signs and symptoms of heart failure. Myocarditis, pericarditis Pericarditis Pericarditis is an inflammation of the pericardium, often with fluid accumulation. It can be caused by infection (often viral), myocardial infarction, drugs, malignancies, metabolic disorders, autoimmune disorders, or trauma. Acute, subacute, and chronic forms exist. Pericarditis, tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, valvular heart disease |
| Genitourinary | Urethritis Urethritis Inflammation involving the urethra. Similar to cystitis, clinical symptoms range from vague discomfort to painful urination (dysuria), urethral discharge, or both. Urinary Tract Infections (UTIs), prostatitis Prostatitis Prostatitis is inflammation or an irritative condition of the prostate that presents as different syndromes: acute bacterial, chronic bacterial, chronic prostatitis/chronic pelvic pain, and asymptomatic. Bacterial prostatitis is easier to identify clinically and the management (antibiotics) is better established. Prostatitis, cystitis Cystitis Inflammation of the urinary bladder, either from bacterial or non-bacterial causes. Cystitis is usually associated with painful urination (dysuria), increased frequency, urgency, and suprapubic pain. Urinary Tract Infections (UTIs), interstitial nephritis, nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome |
| Central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification | Lethargy Lethargy A general state of sluggishness, listless, or uninterested, with being tired, and having difficulty concentrating and doing simple tasks. It may be related to depression or drug addiction. Hyponatremia, increased irritability, aseptic meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis, sensorineural deafness |
| Respiratory | Shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, influenza-like illness, pleural effusion Pleural Effusion Pleural effusion refers to the accumulation of fluid between the layers of the parietal and visceral pleura. Common causes of this condition include infection, malignancy, autoimmune disorders, or volume overload. Clinical manifestations include chest pain, cough, and dyspnea. Pleural Effusion, cough, rhinorrhea Rhinorrhea Excess nasal drainage. Respiratory Syncytial Virus |
| Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions | Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion and induration Induration Dermatologic Examination at BCG BCG An active immunizing agent and a viable avirulent attenuated strain of Mycobacterium bovis, which confers immunity to mycobacterial infections. It is used also in immunotherapy of neoplasms due to its stimulation of antibodies and non-specific immunity. Cancer Immunotherapy (bacille Calmette-Guérin) vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination site, Beau’s lines, finger gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction |
| General | Irritability, decreased PO intake, lethargy Lethargy A general state of sluggishness, listless, or uninterested, with being tired, and having difficulty concentrating and doing simple tasks. It may be related to depression or drug addiction. Hyponatremia |
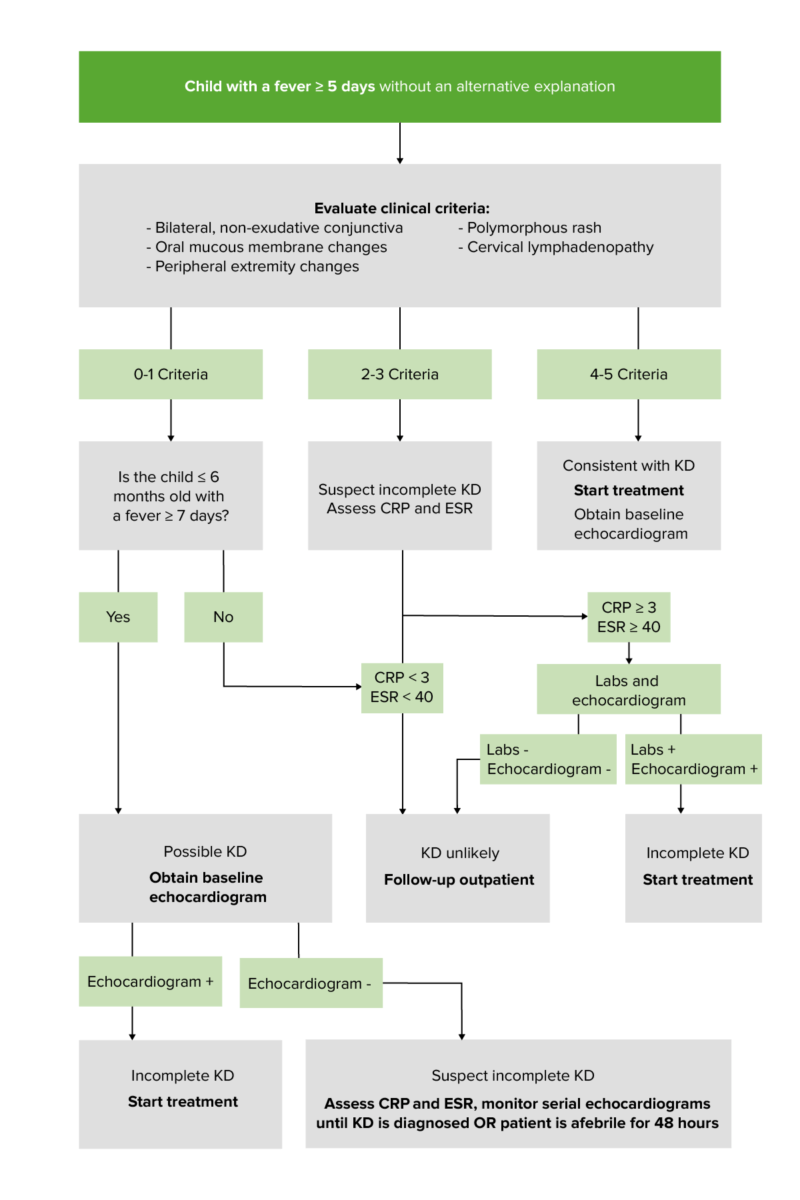
Diagnostic algorithm for children with fever/diagnosis of Kawasaki disease:
Units: CRP in mg/dL; erythrocyte sedimentation rate (ESR) in mm/hr
Positive labs (≥ 3 supplemental laboratory findings) include:
Anemia (for age)
↑ Platelet count
↑ WBC
↓ Albumin
↑ ALT
Pyuria
To recall the important clinical criteria for KD, remember CRASH and Burn:
Conjunctivitis
Rash
Adenopathy
Strawberry
tongue
Tongue
The tongue, on the other hand, is a complex muscular structure that permits tasting and facilitates the process of mastication and communication. The blood supply of the tongue originates from the external carotid artery, and the innervation is through cranial nerves.
Lips and Tongue: Anatomy
Hands and feet
Burn:
fever
Fever
Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin.
Fever

Echocardiography view at the level of aortic valve demonstrating an increase in the size of a coronary artery aneurysm (arrowheads) secondary to KD
Image: “Follow-up echocardiography” by Department of Cardiology, Dr. Balabhai Nanavati Hospital, Mumbai, India. License: CC BY 2.0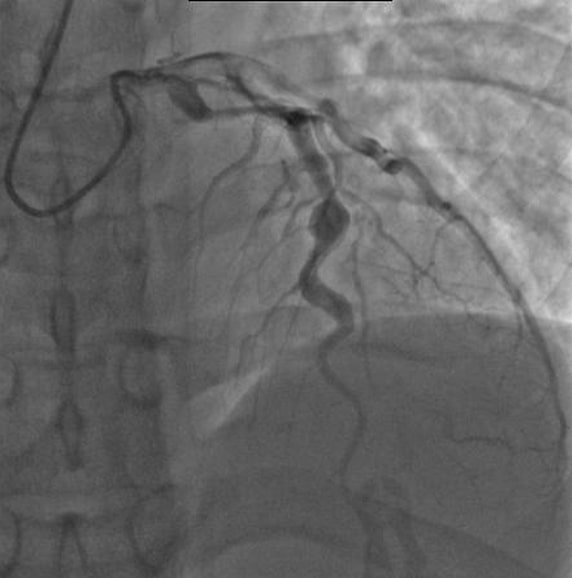
Angiography of a patient with KD showing ectatic left anterior descending coronary artery, with the largest aneurysm measuring 6.5 mm in diameter.
Image: “Angiography showing ectatic LAD,” by mprice18. License: CC BY 3.0| Medication | Indication |
|---|---|
| Clopidogrel Clopidogrel A ticlopidine analog and platelet purinergic p2y receptor antagonist that inhibits adenosine diphosphate-mediated platelet aggregation. It is used to prevent thromboembolism in patients with arterial occlusive diseases; myocardial infarction; stroke; or atrial fibrillation. Antiplatelet Drugs, dipyridamole Dipyridamole A phosphodiesterase inhibitor that blocks uptake and metabolism of adenosine by erythrocytes and vascular endothelial cells. Dipyridamole also potentiates the antiaggregating action of prostacyclin. Phosphodiesterase Inhibitors, and other antiplatelet drugs | For small-to-medium-sized aneurysms of the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology and a high risk for thrombus formation |
| Low-molecular-weight heparin, warfarin Warfarin An anticoagulant that acts by inhibiting the synthesis of vitamin K-dependent coagulation factors. Warfarin is indicated for the prophylaxis and/or treatment of venous thrombosis and its extension, pulmonary embolism, and atrial fibrillation with embolization. It is also used as an adjunct in the prophylaxis of systemic embolism after myocardial infarction. Warfarin is also used as a rodenticide. Anticoagulants, and other anticoagulants Anticoagulants Anticoagulants are drugs that retard or interrupt the coagulation cascade. The primary classes of available anticoagulants include heparins, vitamin K-dependent antagonists (e.g., warfarin), direct thrombin inhibitors, and factor Xa inhibitors. Anticoagulants | For large aneurysms of the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology with a high risk of thrombus formation |
| Infliximab Infliximab A chimeric monoclonal antibody to tnf-alpha that is used in the treatment of rheumatoid arthritis; ankylosing spondylitis; psoriatic arthritis and Crohn’s disease. Disease-Modifying Antirheumatic Drugs (DMARDs), cyclophosphamide Cyclophosphamide Precursor of an alkylating nitrogen mustard antineoplastic and immunosuppressive agent that must be activated in the liver to form the active aldophosphamide. It has been used in the treatment of lymphoma and leukemia. Its side effect, alopecia, has been used for defleecing sheep. Cyclophosphamide may also cause sterility, birth defects, mutations, and cancer. Immunosuppressants, and cyclosporine Cyclosporine A cyclic undecapeptide from an extract of soil fungi. It is a powerful immunosupressant with a specific action on T-lymphocytes. It is used for the prophylaxis of graft rejection in organ and tissue transplantation. Immunosuppressants | Refractory cases with coronary aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms |
| Corticosteroids Corticosteroids Chorioretinitis | Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who do not respond to standard treatments and therapies or are at risk for IVIG IVIG Dermatomyositis resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing |
References