Polyneuropathy is any disease process affecting the function of or causing damage to multiple nerves of the peripheral nervous system Peripheral nervous system The nervous system outside of the brain and spinal cord. The peripheral nervous system has autonomic and somatic divisions. The autonomic nervous system includes the enteric, parasympathetic, and sympathetic subdivisions. The somatic nervous system includes the cranial and spinal nerves and their ganglia and the peripheral sensory receptors. Nervous System: Anatomy, Structure, and Classification. There are numerous etiologies of polyneuropathy, most of which are systemic and the most common of which is diabetic neuropathy Neuropathy Leprosy. The clinical presentation varies by etiology as well as classification of the polyneuropathy, but generally manifests as sensorimotor disturbances ( pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, paresthesia, numbness, weakness, and loss of coordination Coordination Cerebellar Disorders and balance), which have a gradual onset and progressive course. Distal nerves are affected most commonly, but the disease process may progress proximally with time or progression of the underlying etiologic disease entity. Diagnosis is made clinically, but laboratory studies, electrodiagnostic testing, and/or nerve biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma may be required in some cases. Management varies depending on the etiology.
Last updated: Mar 29, 2023
Polyneuropathy is part of a spectrum of neurologic disorders affecting the integrity and function of the peripheral nerves Peripheral Nerves The nerves outside of the brain and spinal cord, including the autonomic, cranial, and spinal nerves. Peripheral nerves contain non-neuronal cells and connective tissue as well as axons. The connective tissue layers include, from the outside to the inside, the epineurium, the perineurium, and the endoneurium. Nervous System: Histology. The nomenclature corresponds with the number of nerves involved:
Polyneuropathies Polyneuropathies Diseases of multiple peripheral nerves simultaneously. Polyneuropathies usually are characterized by symmetrical, bilateral distal motor and sensory impairment with a graded increase in severity distally. The pathological processes affecting peripheral nerves include degeneration of the axon, myelin or both. The various forms of polyneuropathy are categorized by the type of nerve affected (e.g., sensory, motor, or autonomic), by the distribution of nerve injury (e.g., distal vs. Proximal), by nerve component primarily affected (e.g., demyelinating vs. axonal), by etiology, or by pattern of inheritance. Mononeuropathy and Plexopathy may be classified on the basis of:
There are numerous causes of polyneuropathy; however, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus (diabetic neuropathy Neuropathy Leprosy) and chronic alcohol use ( alcoholic Alcoholic Persons who have a history of physical or psychological dependence on ethanol. Mallory-Weiss Syndrome (Mallory-Weiss Tear) neuropathy Neuropathy Leprosy) are responsible for almost 50% of all polyneuropathies Polyneuropathies Diseases of multiple peripheral nerves simultaneously. Polyneuropathies usually are characterized by symmetrical, bilateral distal motor and sensory impairment with a graded increase in severity distally. The pathological processes affecting peripheral nerves include degeneration of the axon, myelin or both. The various forms of polyneuropathy are categorized by the type of nerve affected (e.g., sensory, motor, or autonomic), by the distribution of nerve injury (e.g., distal vs. Proximal), by nerve component primarily affected (e.g., demyelinating vs. axonal), by etiology, or by pattern of inheritance. Mononeuropathy and Plexopathy. Most cases are likely multifactorial. Therefore, the various etiologic entities will be presented as both risk factors and distinct etiologic causes.
The following description is of the pathophysiology of diabetic polyneuropathy, as its pathogenesis is the most studied and most well understood. Many of the pathologic processes are common to other forms of polyneuropathy. Key distinguishing characteristics of other entities will be pointed out in the discussions of those entities.
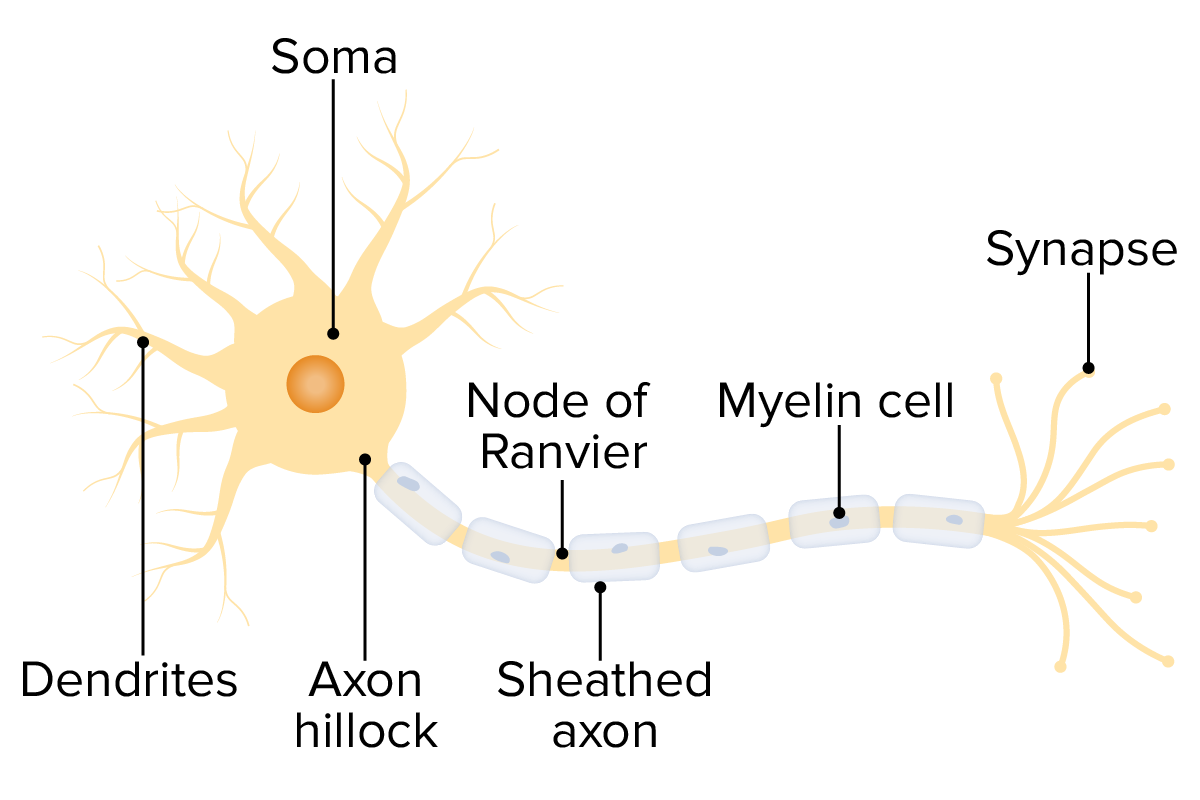
The structure of a neuron allows demonstration of the different areas that may be affected in polyneuropathies.
Image by Lecturio.Take a complete history, including:
Full neurologic exam to discover any focal neurologic deficits Neurologic Deficits High-Risk Headaches:
Pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways management:
Disease-modifying therapies: