The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a disorder of impaired water excretion due to the inability to suppress the secretion of antidiuretic hormone (ADH). There are many causes of SIADH, including increased pituitary production of ADH (related to trauma, disease, or medications), ectopic production of ADH by a tumor, and hereditary disorders. SIADH is characterized by impaired water excretion, leading to dilutional hyponatremia. This condition is usually asymptomatic but may cause neurologic symptoms. SIADH should be suspected in any patient with hyponatremia, hypo-osmolality, and high urine osmolality.
Last updated: May 17, 2024
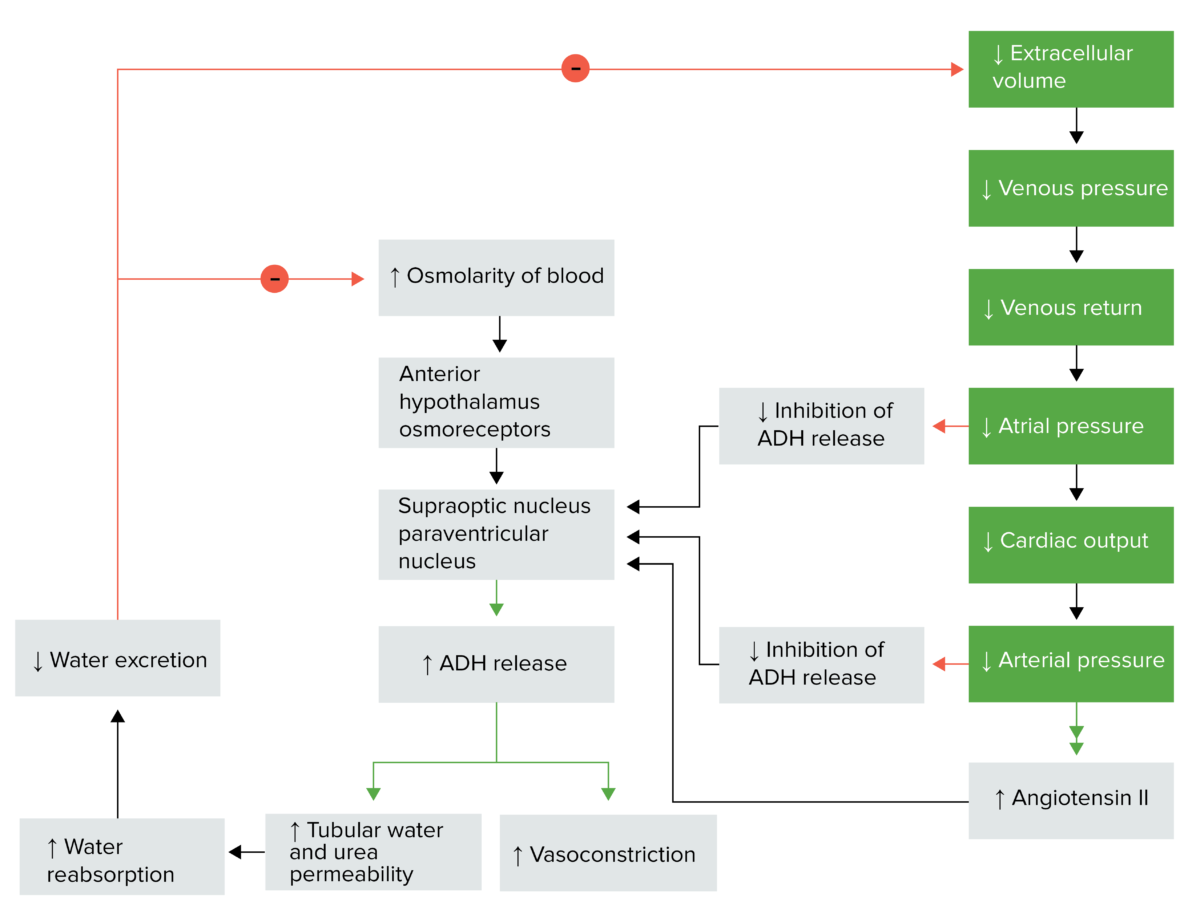
Antidiuretic hormone regulation
Image by Lecturio.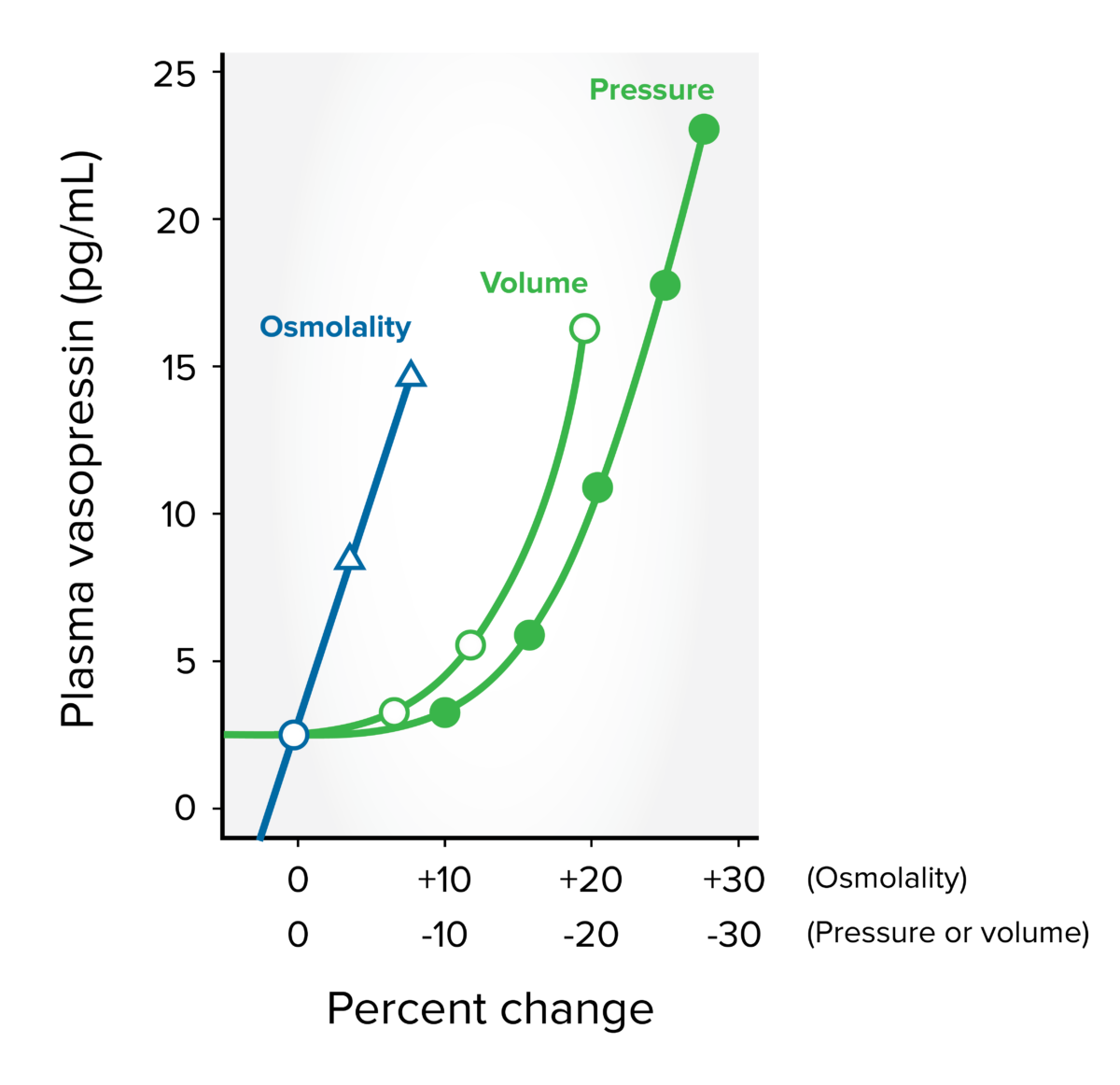
Antidiuretic hormone secretion: directly related to plasma osmolality, blood pressure, and blood volume
Image by Lecturio.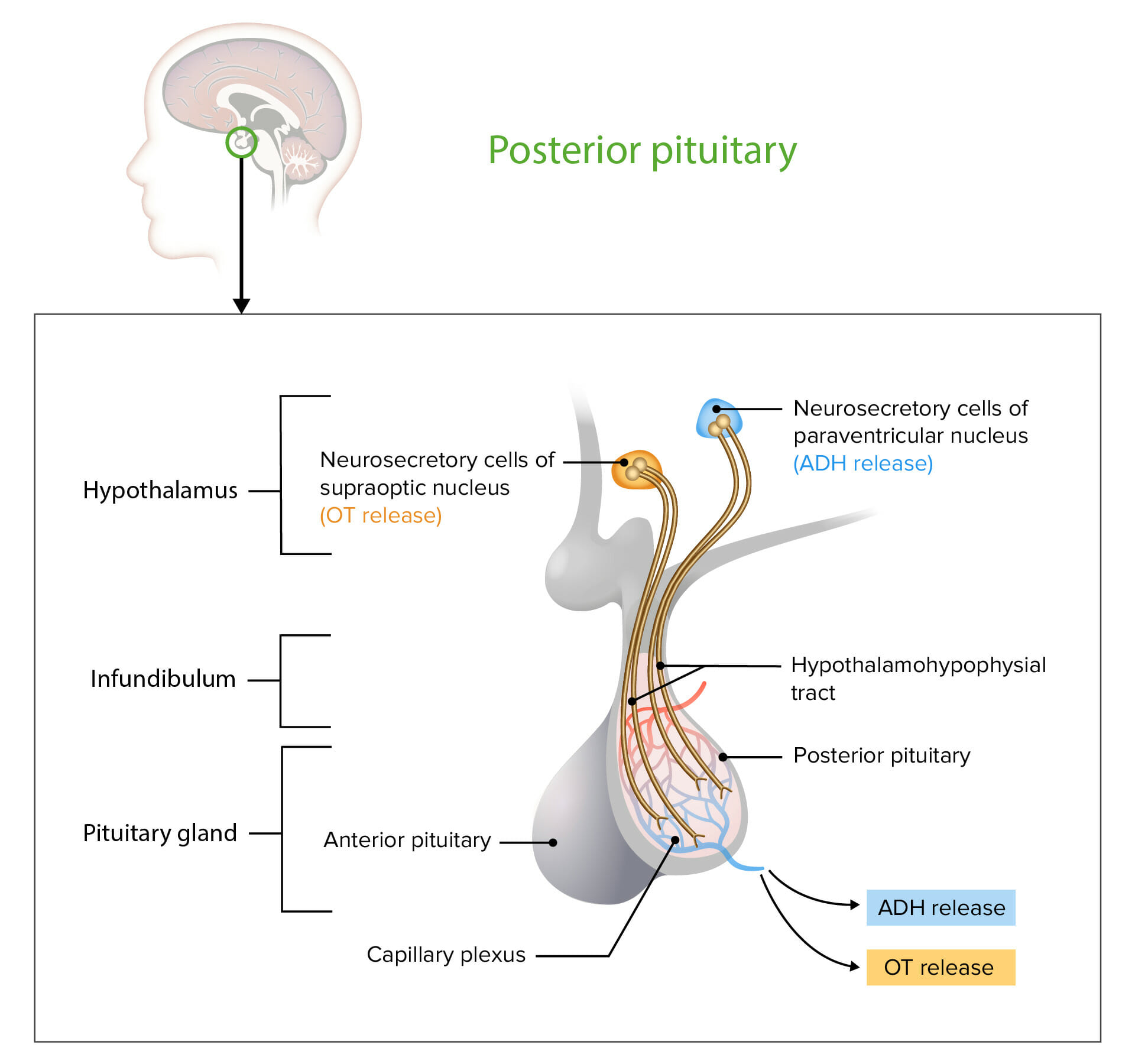
Neurosecretory cells in the hypothalamus release OT or ADH into the posterior lobe of the pituitary gland. The hormones are stored or released into the blood via the capillary plexus.
OT: oxytocin
ADH: antidiuretic hormone
| Major causes | Examples |
|---|---|
| Central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification causes |
|
| Neoplasms Neoplasms New abnormal growth of tissue. Malignant neoplasms show a greater degree of anaplasia and have the properties of invasion and metastasis, compared to benign neoplasms. Benign Bone Tumors |
|
| Pulmonary causes |
|
| Medications |
|
| Surgery |
|
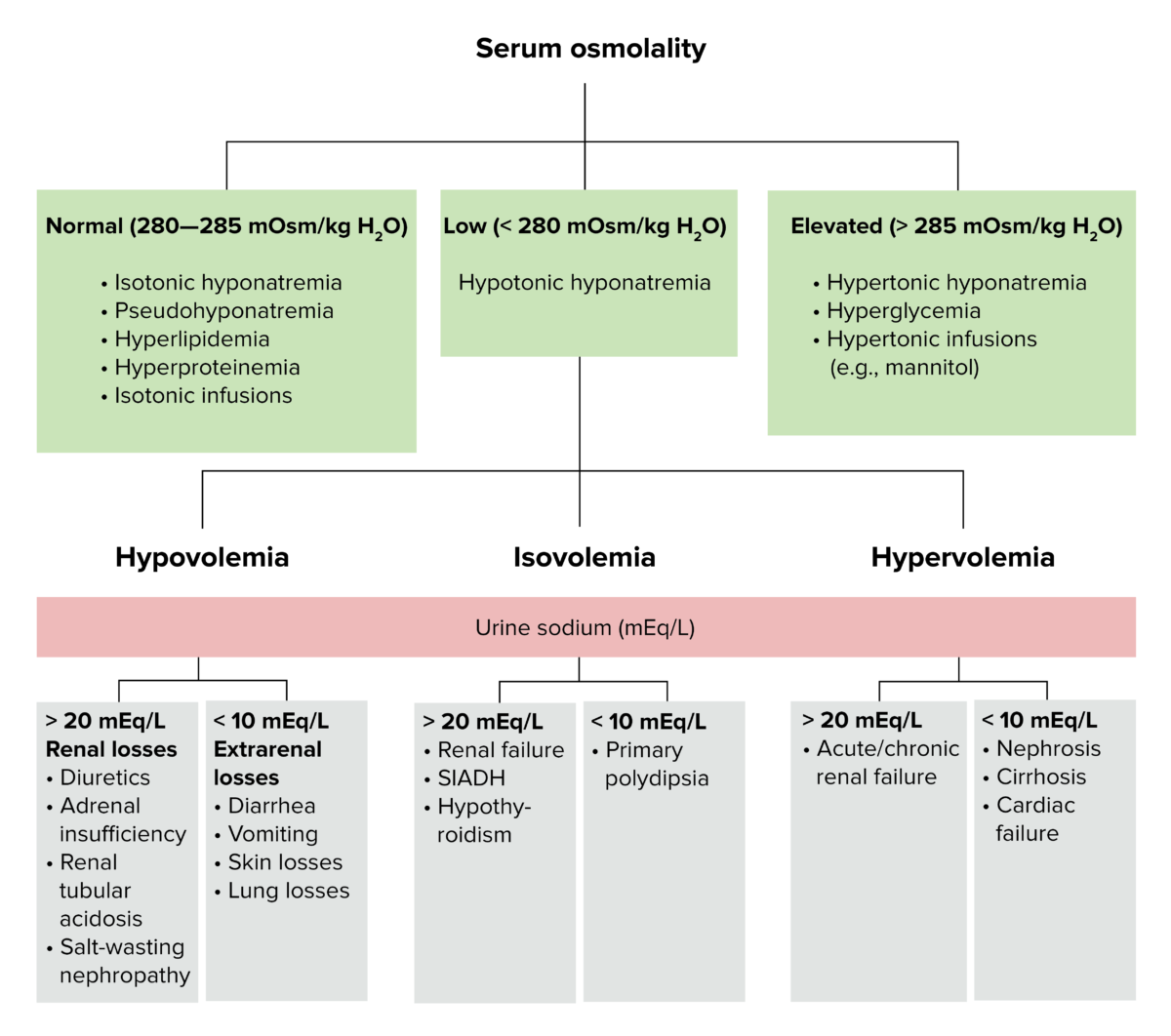
Diagnostic algorithm for volemic and sodium alterations
Image by Lecturio.The differential diagnosis of SIADH includes other hyponatremic conditions: