Congenital diaphragmatic hernias are embryologically derived defects in the diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy through which abdominal structures can pass into the chest cavity. The presence of intestines and intra-abdominal organs in the chest interferes with embryonic development of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy, which is the major cause of pathology postnatally. Prenatal diagnosis is commonly made by ultrasound during pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care followed by confirmation on chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests after birth. Immediate respiratory resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome at birth with endotracheal intubation Intubation Peritonsillar Abscess and mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing are required. Surgical repair is the only curative option. Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas varies, but children with diaphragmatic hernias usually suffer from lifelong pulmonary complications.
Last updated: Jan 21, 2025
Multiple embryological mechanisms have been proposed:
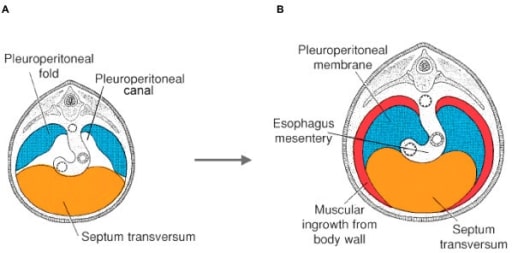
Embryological development of the diaphragm morphogenesis depicted at 5 weeks (A) and 4 months (B) of gestation.
The diaphragm is described as arising from the septum transversum, pleuroperitoneal folds (PPFs), esophageal mesentery, and thoracic body wall.
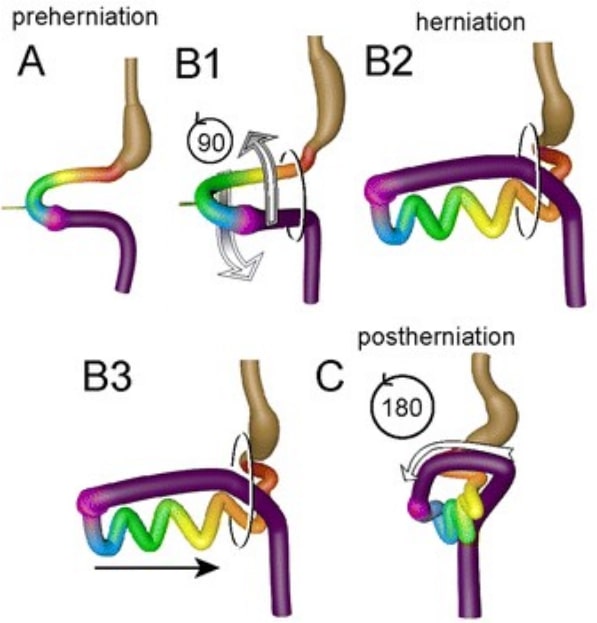
Diagram showing intestinal rotation and herniation during normal embryonic development. From panel A to B, the midgut loop rotates 90° in a counterclockwise direction, so that its position changes from midsagittal (A) to transverse (B1).
The small intestine forms loops (B2) and slides back into the abdomen (B3) during resolution of the hernia. Meanwhile, the cecum moves from the left to the right side, which represents the additional 180° counterclockwise rotation of the intestine (C, central view).
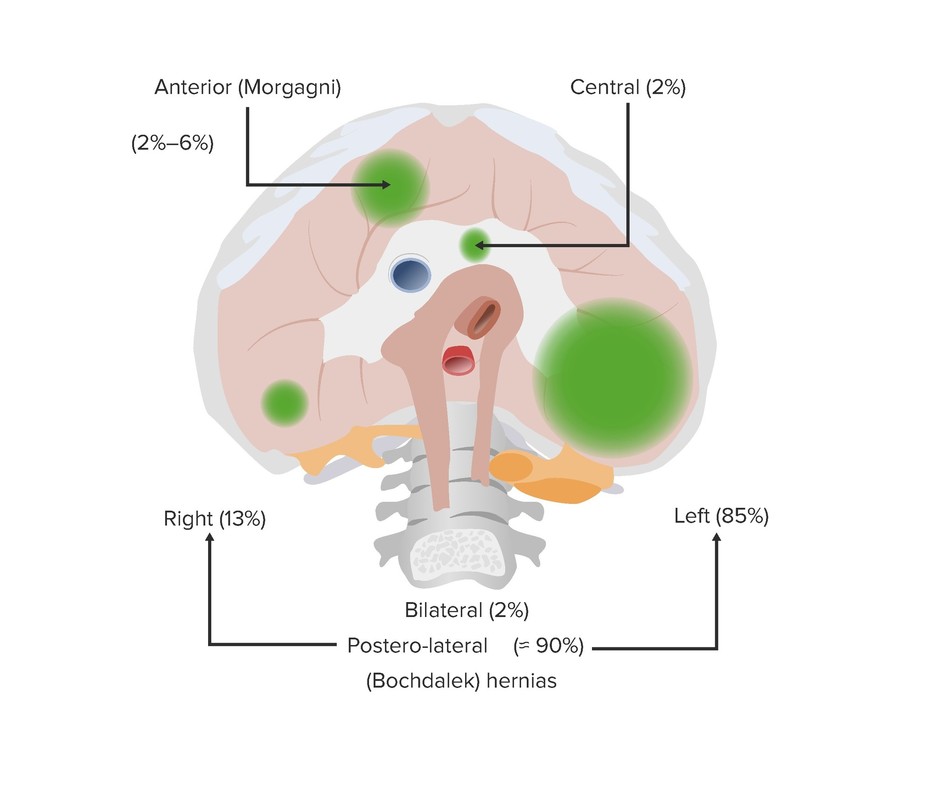
Classification of CDH based on the location of diaphragmatic hernias.
The most common type is the posterior lateral hernia (approximately 90%), also known as Bochdalek hernia. Most of these hernias occur on the left side (85%).
Other types of hernias are the anterior defect or Morgagni hernia (2%–6%), followed by the rare central hernia (2%).
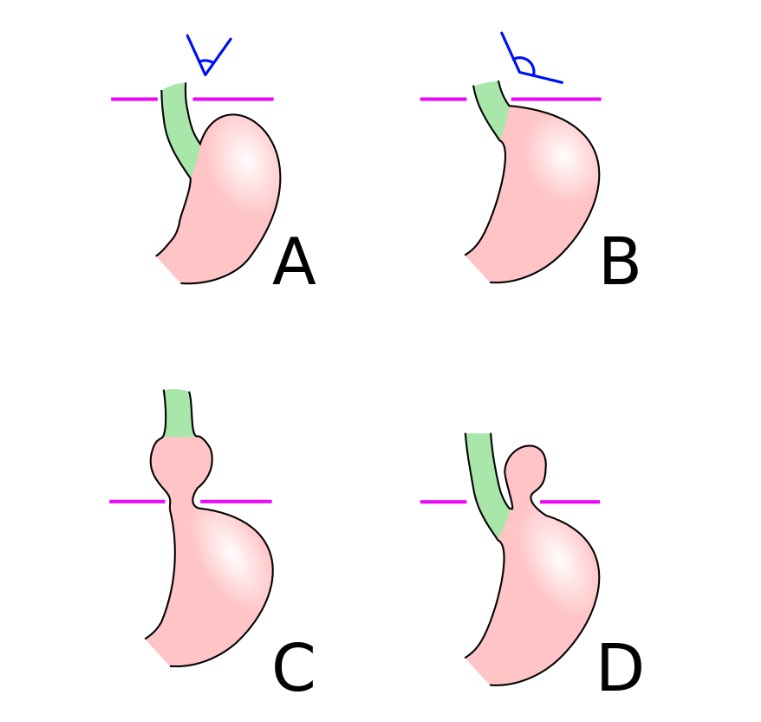
A: Normal anatomy
B: Pre-stage
C: Sliding hiatus hernia
D: Paraesophageal hiatus hernia
Pathological effects of CDH are due to lung hypoplasia Hypoplasia Hypoplastic Left Heart Syndrome (HLHS):

Ultrasonography: Congenital diaphragmatic hernia. The heart (arrow) is pushed to the right within the thorax and the stomach (STM) is seen in the thorax.
Image: “Congenital diaphragmatic hernia” by US National Library of Medicine. License: CC BY 2.0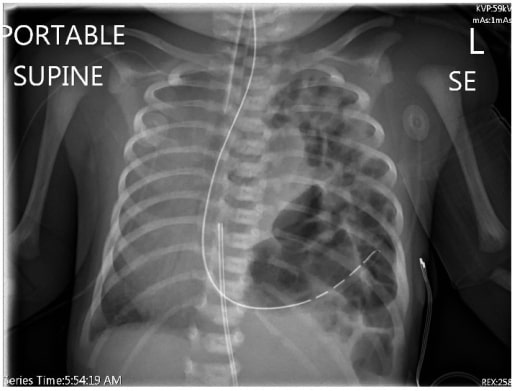
Chest radiograph showing left diaphragmatic hernia and contralateral shift of the heart and mediastinum
Image: “Chest radiograph” by Alberta Children’s Hospital, Calgary, AB, Canada T3B 6A8. License: CC BY 4.0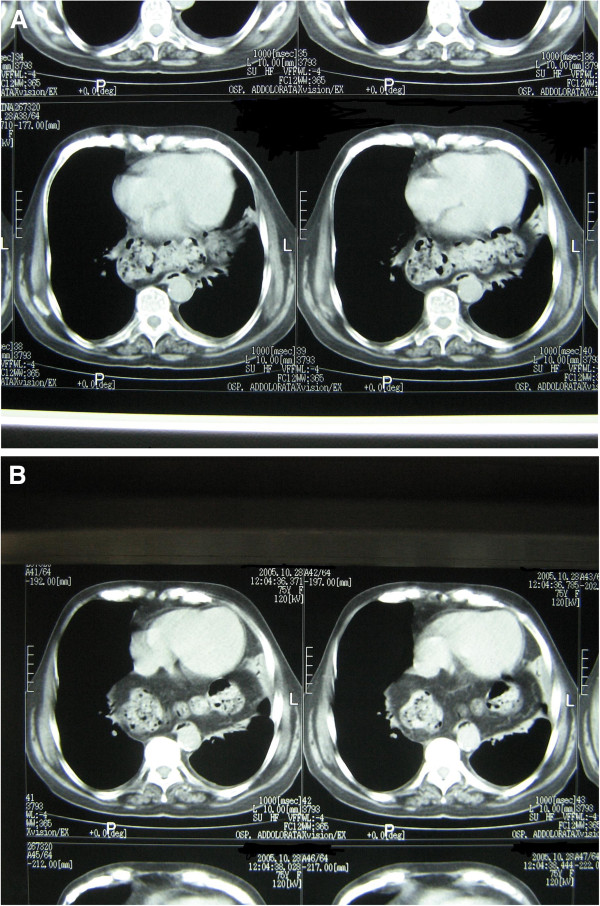
Axial CT scan of the chest: Gas-filled large bowel loops are visible behind the heart, lying anteriorly to the spine and the aorta.
Image: “Axial CT scan of the chest” by Department of Anatomical, Histological, Forensic and Locomotor System Sciences, V, A, Borelli 50, Rome, 00161, Italy. License: CC BY 2.0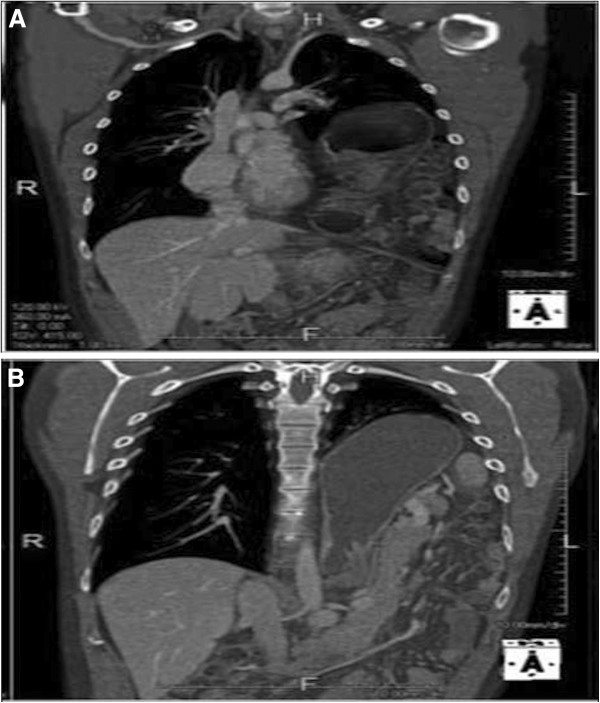
Computed tomography scan of the chest. Coronal reconstruction. Part of the stomach, adjacent to the heart (A), is clearly visible. Some bowel loops (B) are also visible on the left side of the chest: the left lung is displaced and compressed.
Image: “Computed tomography scan of the chest” by 2013 Bianchi et al., BioMed Central Ltd. License: CC BY 2.0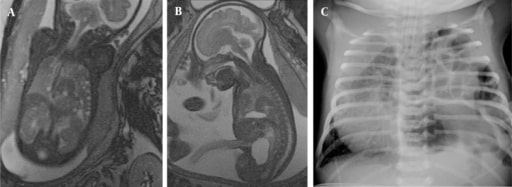
Congenital diaphragmatic hernia in a fetus at 35 weeks’ gestation, including intestines and spleen on, coronal (A) and sagittal images (B), and postnatal chest X-ray (C)
Image: “Congenital diaphragmatic hernia in the 35th GW fetus” by Department of Radiology, School of Medicine, Acibadem University, Istanbul, Turkey. License: CC BY 3.0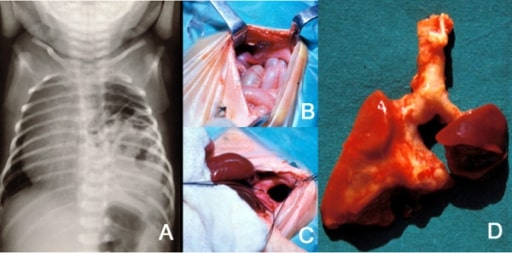
A: Plain X-ray of the thorax of a newborn with CDH. There are bowel loops into the left hemithorax, the mediastinum is displaced to the contralateral side, and the space occupied by the lung is reduced.
B and C: At laparotomy, a left posterolateral diaphragmatic hernia was discovered.
In B, small bowel loops can be seen entering the thorax through the orifice.
In C, this is seen after reducing the contents of the hernia.
D: The patient died of severe persistent pulmonary hypertension days later. At autopsy, extreme left lung hypoplasia and less severe right lung hypoplasia were discovered.
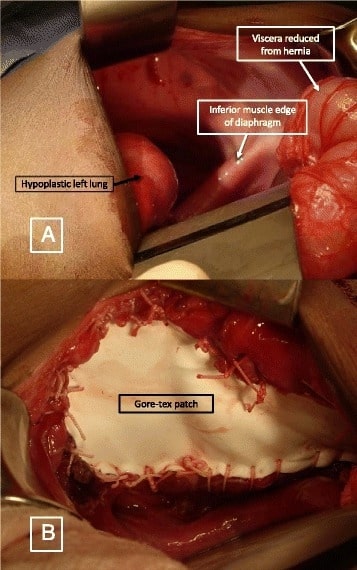
A: Left-sided diaphragmatic hernia showing the hypoplastic left lung, inferior muscle edge of the diaphragm, and reduced viscera
B: Prosthetic patch (Gore-Tex patch) used to close the defect
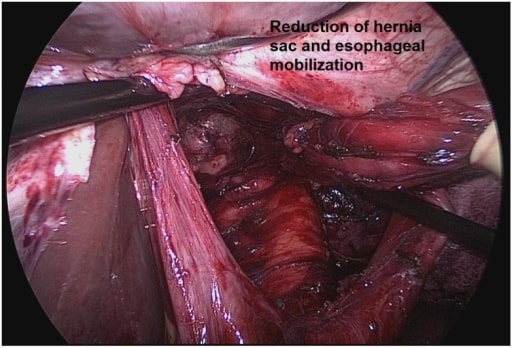
Paraesophageal hernia repair: complete sac excision and mobilization of an adequate segment of intra-abdominal esophagus
Image: “Complete sac excision” by Department of Surgery, Brigham and Women’s Hospital, Boston VA Health Care System, Boston, MA , USA. License: CC BY 4.0