Vesicoureteral reflux (VUR) is the retrograde flow Retrograde flow Veins: Histology of urine from the bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess into the upper urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy. Primary VUR often results from the incomplete closure of the ureterovesical junction, whereas secondary VUR is due to an anatomic or physiologic obstruction. Vesicoureteral reflux does not cause specific symptoms, but it is suspected after detecting hydronephrosis Hydronephrosis Hydronephrosis is dilation of the renal collecting system as a result of the obstruction of urine outflow. Hydronephrosis can be unilateral or bilateral. Nephrolithiasis is the most common cause of hydronephrosis in young adults, while prostatic hyperplasia and neoplasm are seen in older patients. Hydronephrosis on prenatal ultrasonography or in a young child presenting with a urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infection. A voiding cystourethrogram Voiding Cystourethrogram Urinary Tract Infections (UTIs) in Children should be performed to diagnose the condition and assess its severity. The majority of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will have spontaneous resolution of VUR. Some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may require surgical management, particularly individuals with high-grade reflux.
Last updated: Jun 15, 2025
Vesicoureteral reflux (VUR) is the retrograde flow Retrograde flow Veins: Histology of urine from the bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess into the upper urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy.
Primary VUR:
Secondary VUR:
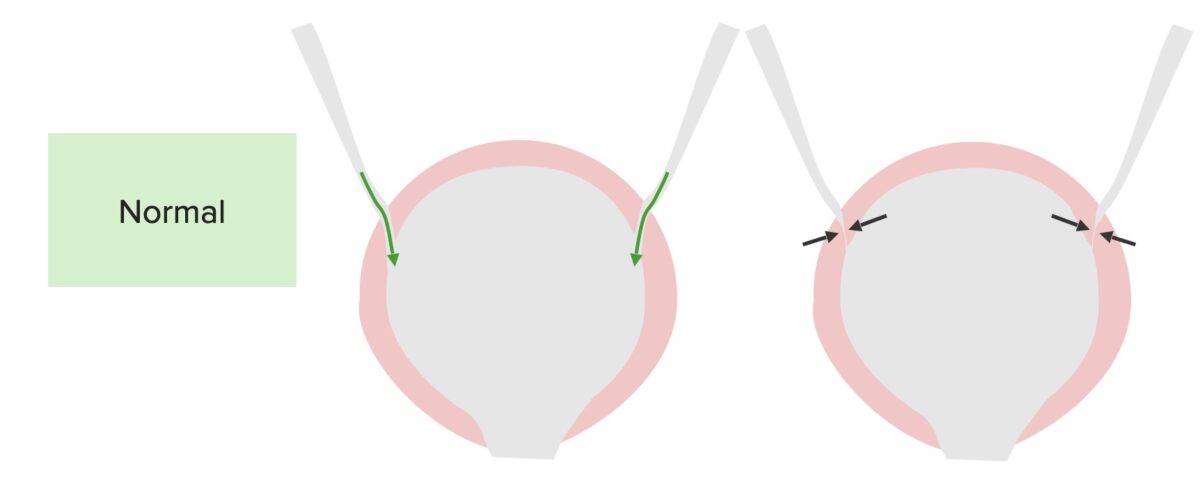
Normal function of the bladder and ureters:
The ureters enter at an angle, allowing the bladder to squeeze the ureteral opening, which is closed during micturition to prevent reflux.
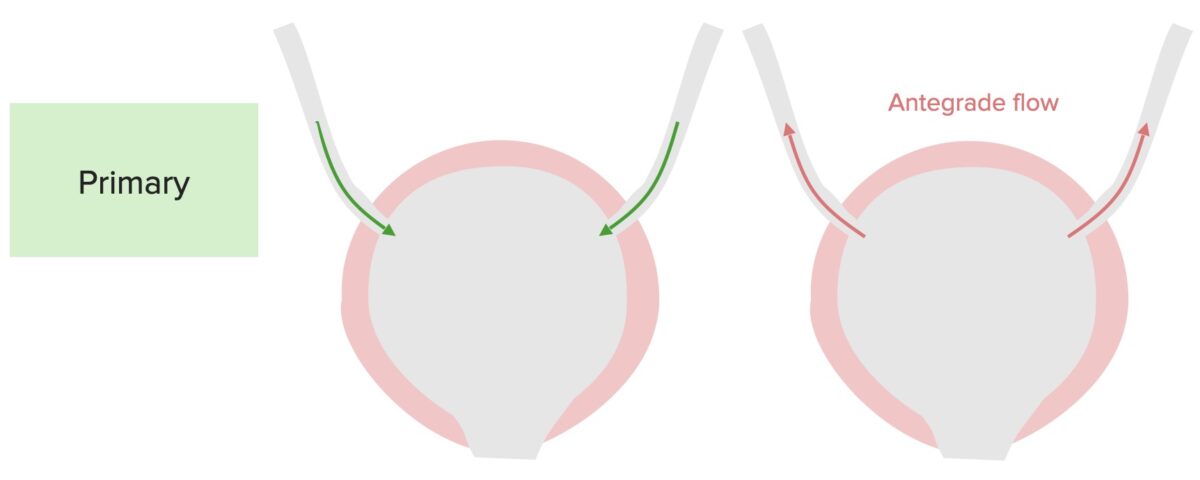
Pathophysiology of primary vesicoureteral reflux:
A defect in the terminal ureter and in the ability to close the ureterovesicular junction results in the antegrade flow up the ureters during micturition.
There are no specific signs or symptoms for VUR, and the condition may be suspected in the following circumstances:
There are no laboratory tests that can diagnose VUR. The following assessments may be performed to evaluate for complications:
Renal and bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess US:
Voiding cystourethrogram Voiding Cystourethrogram Urinary Tract Infections (UTIs) in Children:
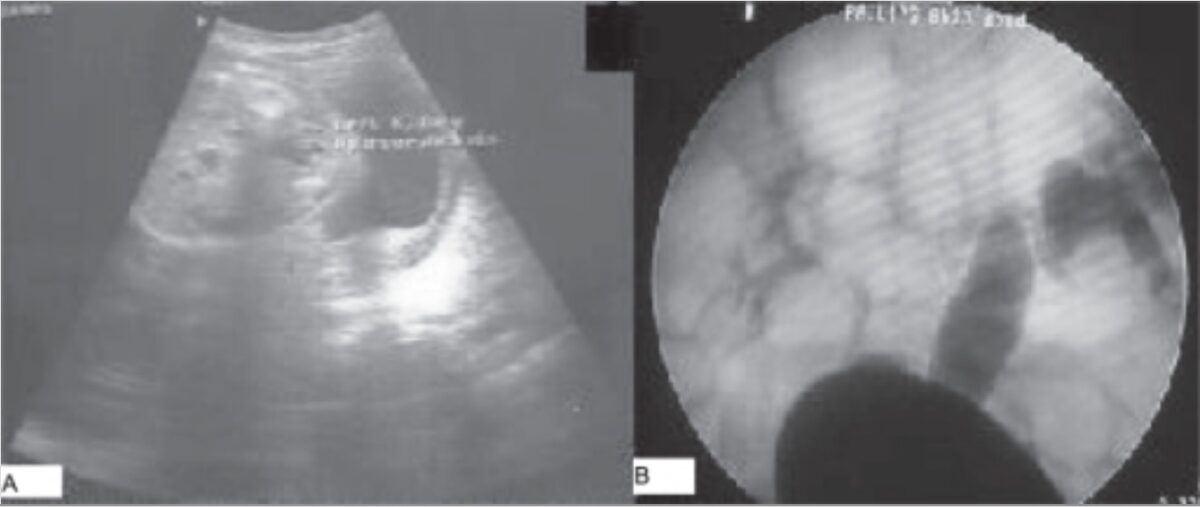
Imaging findings in vesicoureteral reflux:
A: Postnatal ultrasound showing unilateral hydronephrosis
B: Voiding cystourethrogram showing contrast reflux in the right and left ureters and collecting systems (right: grade III, left: grade V)
Severity classification helps grade the severity of VUR based on imaging findings.
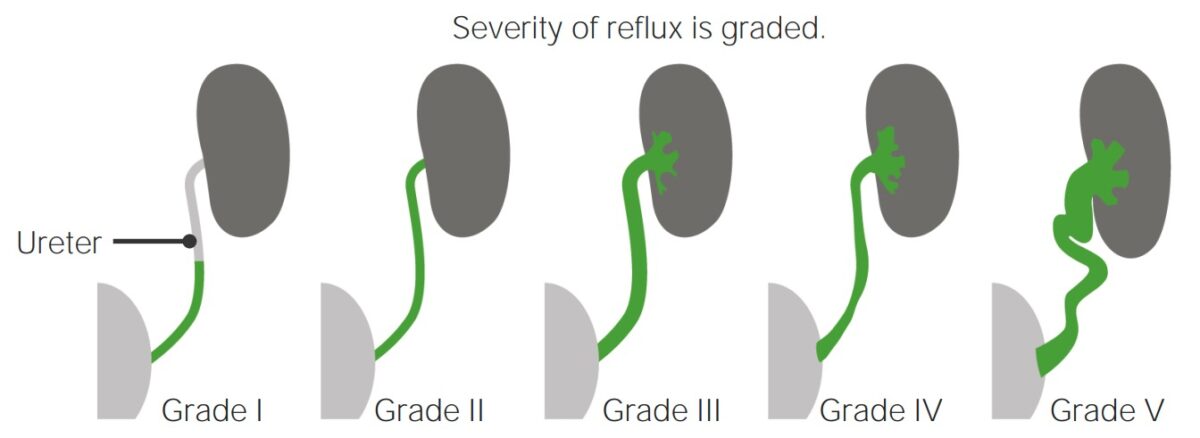
Severity classification of vesicoureteral reflux
Image by Lecturio.Conservative management:
Invasive management: