A retinal vessel occlusion is a blockage in a major artery or vein of the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy. Depending on the location, the occlusion can be classified as central retinal artery occlusion (CRAO), branch retinal artery occlusion (BRAO), central retinal vein occlusion (CRVO), or branch retinal vein occlusion (BRVO). Typically, a retinal vessel occlusion is a thromboembolic event. Risk factors include hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, and cardiac valvular disease. Central retinal vessel occlusion is characterized by sudden, unilateral, painless loss of vision Vision Ophthalmic Exam and/or transient vision Vision Ophthalmic Exam loss ( amaurosis fugax Amaurosis fugax Transient complete or partial monocular blindness due to retinal ischemia. This may be caused by emboli from the carotid artery (usually in association with carotid stenosis) and other locations that enter the central retinal artery. Carotid Artery Stenosis). Treatment options are limited in all cases and usually ineffective. When the macula Macula An oval area in the retina, 3 to 5 mm in diameter, usually located temporal to the posterior pole of the eye and slightly below the level of the optic disk. It is characterized by the presence of a yellow pigment diffusely permeating the inner layers, contains the fovea centralis in its center, and provides the best phototropic visual acuity. It is devoid of retinal blood vessels, except in its periphery, and receives nourishment from the choriocapillaris of the choroid. Eye: Anatomy is involved, prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is especially poor, leading to permanent vision Vision Ophthalmic Exam loss.
Last updated: May 17, 2024
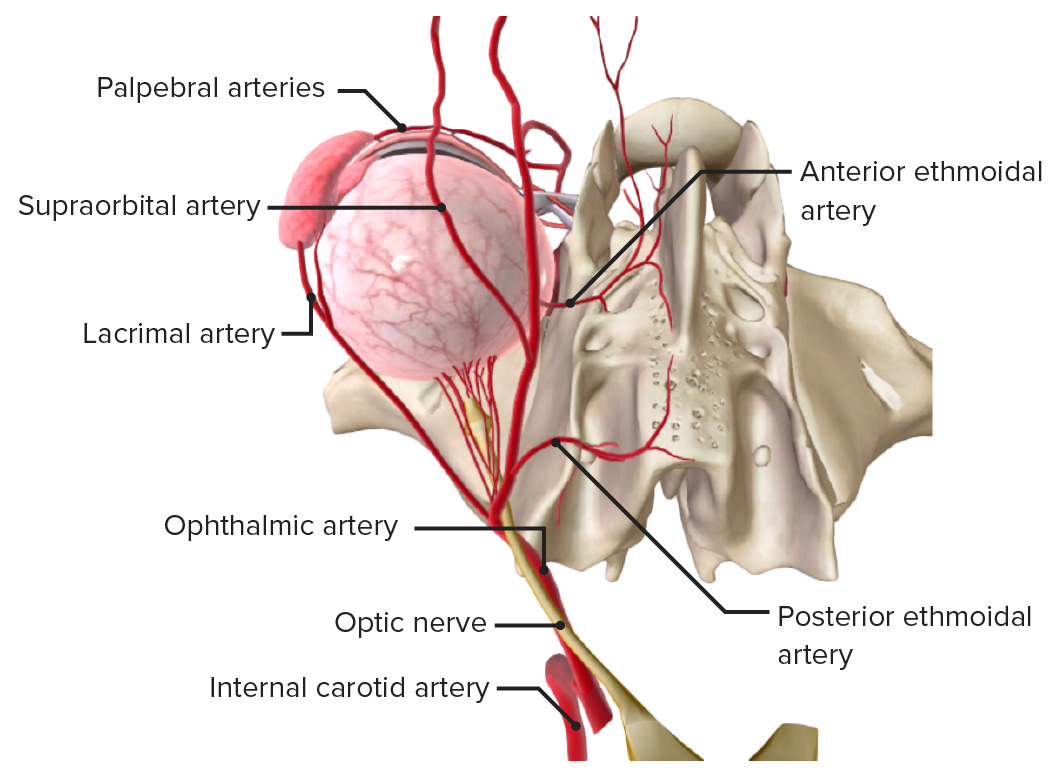
The carotid artery with the ophthalmic artery and branches. Note the central retinal artery and posterior choroidal arteries, which enter the eye around the optic nerve.
Image by BioDigital, edited by Lecturio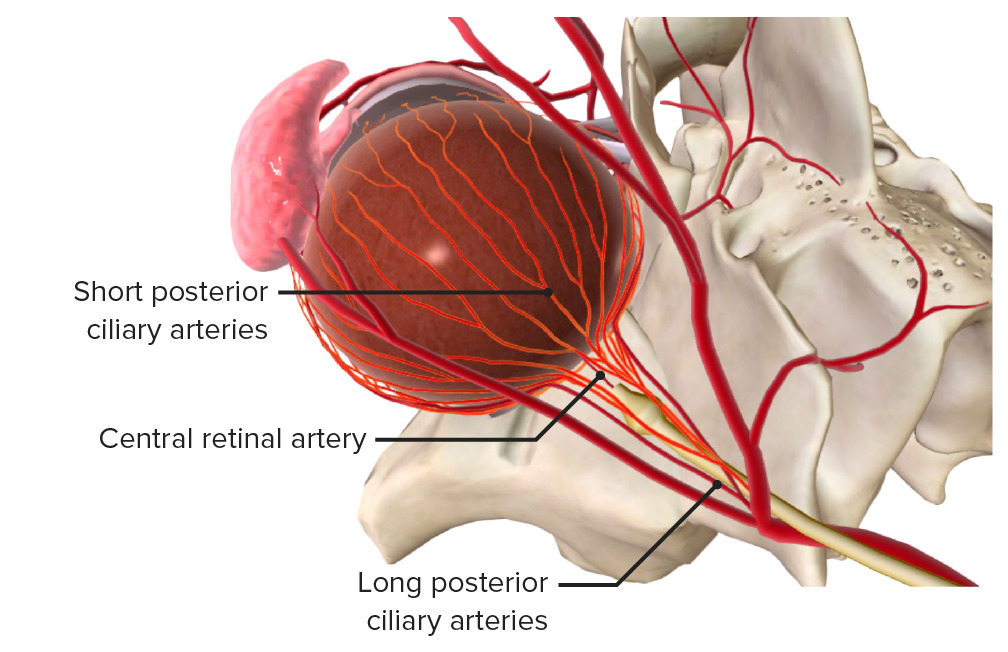
Superior view: The internal carotid artery branches into the ophthalmic artery, which further divides into the central retinal artery and the posterior ciliary arteries.
Image by BioDigital, edited by Lecturio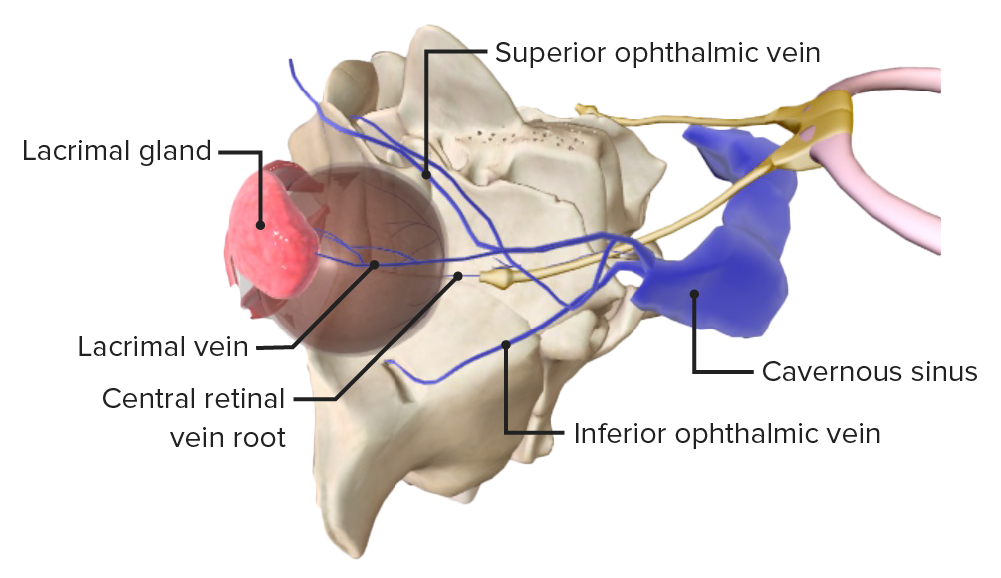
The superior ophthalmic vein and the cavernous sinus, into which the central retinal vein drains.
Image by BioDigital, edited by LecturioExact causes are not known, although there is an association with the following conditions:
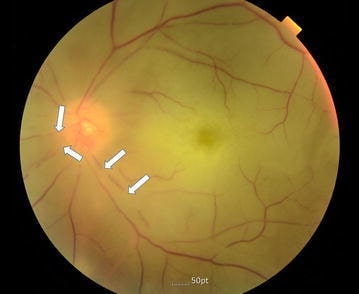
Image showing a color fundus photograph of the left eye with CRAO; retinal artery attenuation (arrows) and optic disc pallor
Image: “Color fundus photography of the left eye” by Division of Cardiology, Department of Internal Medicine, Pohang St. Mary’s Hospital, Pohang, Republic of Korea. License: CC BY 4.0
Fundus photograph of the right eye indicating CRAO/CRVO: a “blood and thunder” appearance and “cherry red” spot are both seen in this image (a patient with systemic lupus erythematosus)
Image: “Chorea and retinal vessel occlusion” by Department of Neurology, Shariati Hospital, Tehran University of Medical Sciences AND Iranian Center of Neurological Research, Tehran, Iran. License: CC BY 2.0Central retinal artery occlusion
Central retinal vein occlusion
Diagnosis of both conditions is usually clinical but additional investigations may be ordered.
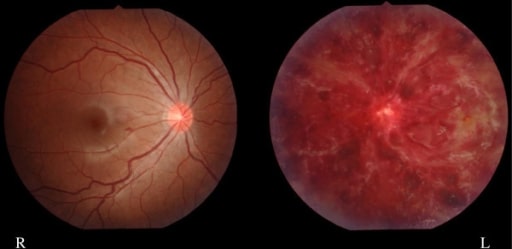
Image of a 15-year-old girl with left intraretinal hemorrhaging (CRVO) (patient has a history of systemic lupus and antiphospholipid antibodies)
Image: “Finding of eye fundus” by Department of Pediatrics and Child Neurology, Oita University Faculty of Medicine, Hasama, Yufu, Oita 879-5593, Japan. License: CC BY 2.0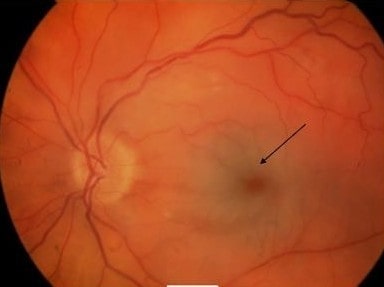
Left eye showing “cherry red” spot with retinal pallor typical of CRAO (arrow)
Image: “Acute central retinal artery occlusion” by James Paget University Hospital NHS Foundation Trust, Lowestoft Road, Gorleston, Great Yarmouth NR31 6LA, Norfolk, UK. License: CC BY 2.0