The head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess examination is the portion of the physical examination done to observe for signs of head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess disease or illness. The head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess examination consists of inspection Inspection Dermatologic Examination, palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination, and auscultation. The information gathered from the physical examination of the head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, along with the information from the history, is used by the physician to generate a differential diagnosis and treatment plan for the patient.
Last updated: Mar 29, 2023
The head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess examination is often annotated as HEENT (head, eyes, ears, nose Nose The nose is the human body’s primary organ of smell and functions as part of the upper respiratory system. The nose may be best known for inhaling oxygen and exhaling carbon dioxide, but it also contributes to other important functions, such as tasting. The anatomy of the nose can be divided into the external nose and the nasal cavity. Nose Anatomy (External & Internal) and throat Throat The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy) in clinical documentation Documentation Systematic organization, storage, retrieval, and dissemination of specialized information, especially of a scientific or technical nature. It often involves authenticating or validating information. Advance Directives shorthand.
Equipment needed:
Positioning:
Environment:
Initial steps:
The 1st part of the head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess exam begins with inspection Inspection Dermatologic Examination of the individual. Note pertinent positive and negative findings.
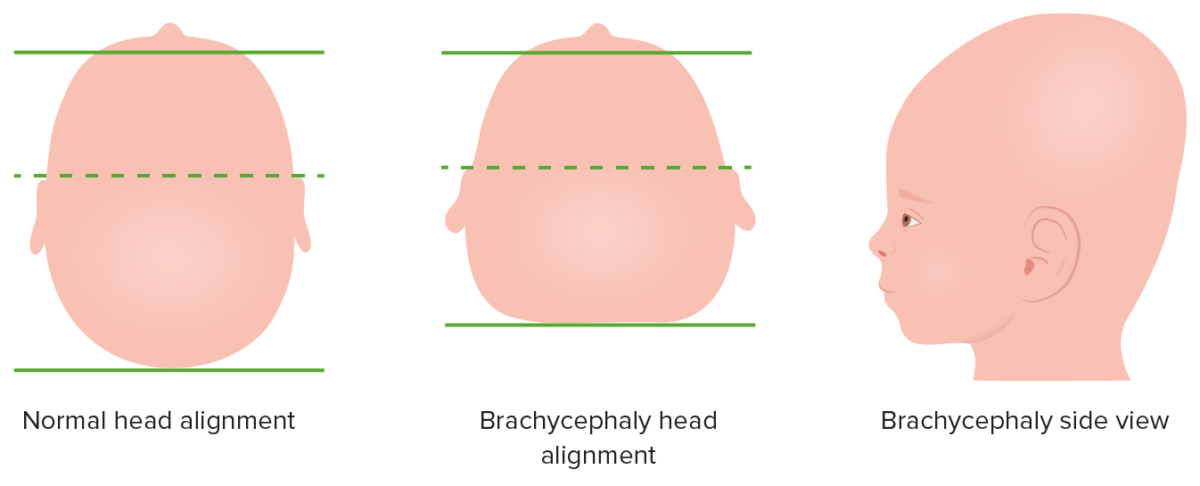
Variation in skull shape
Image by Lecturio. License: CC BY-NC-SA 4.0Classically written as “pupils equal, round, and reactive to light and accommodation” for normal clinical exam documentation Documentation Systematic organization, storage, retrieval, and dissemination of specialized information, especially of a scientific or technical nature. It often involves authenticating or validating information. Advance Directives (PERRLA for shorthand)
General:
Sclera Sclera The white, opaque, fibrous, outer tunic of the eyeball, covering it entirely excepting the segment covered anteriorly by the cornea. It is essentially avascular but contains apertures for vessels, lymphatics, and nerves. Eye: Anatomy and conjunctiva Conjunctiva The mucous membrane that covers the posterior surface of the eyelids and the anterior pericorneal surface of the eyeball. Eye: Anatomy:
Pupils:
Extraocular eye movements:
Fundoscopic exam:
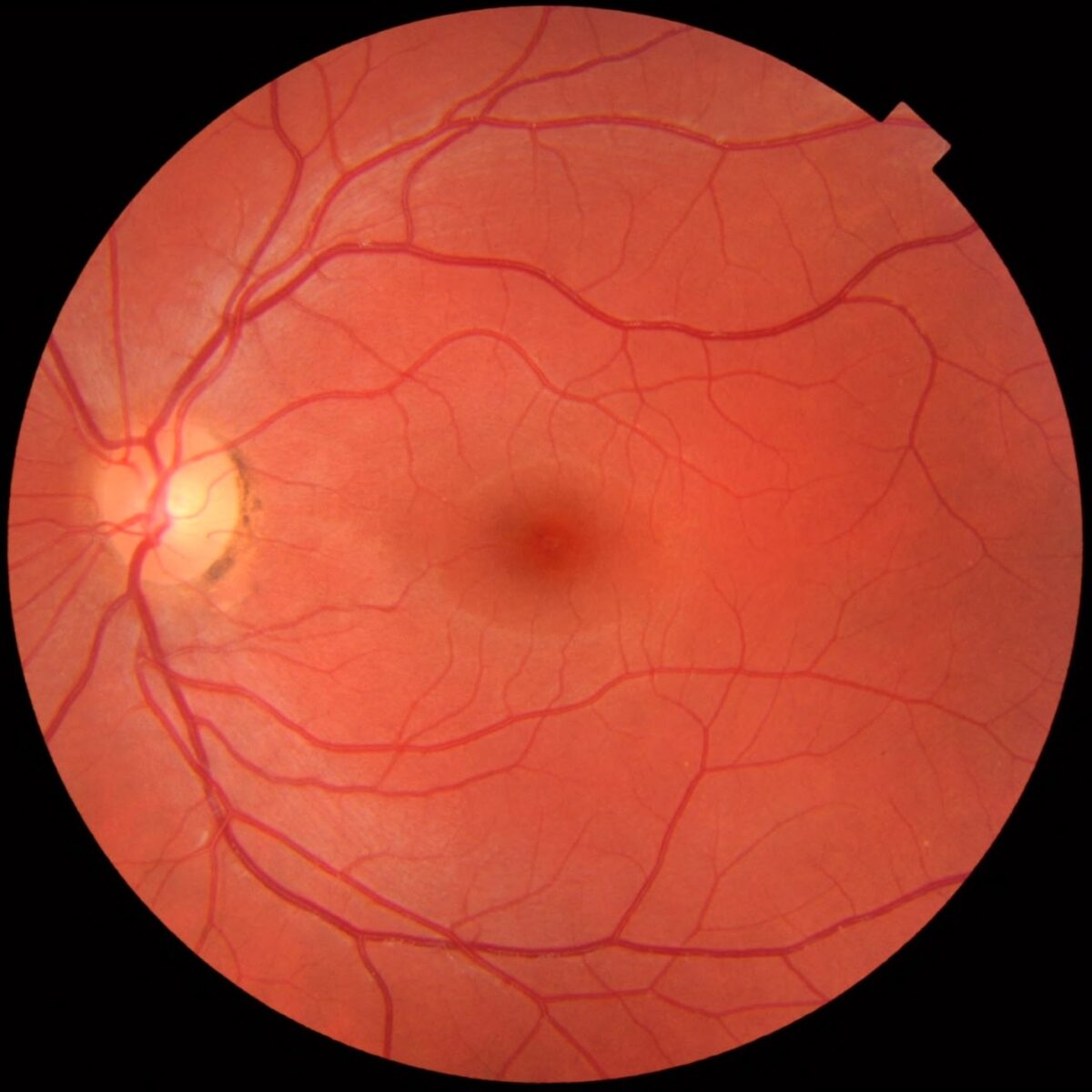
Fundus of the eye as seen through an ophthalmoscope
Image: “Fundus photograph of normal left eye” by Mikael Häggström. License: CC0 1.0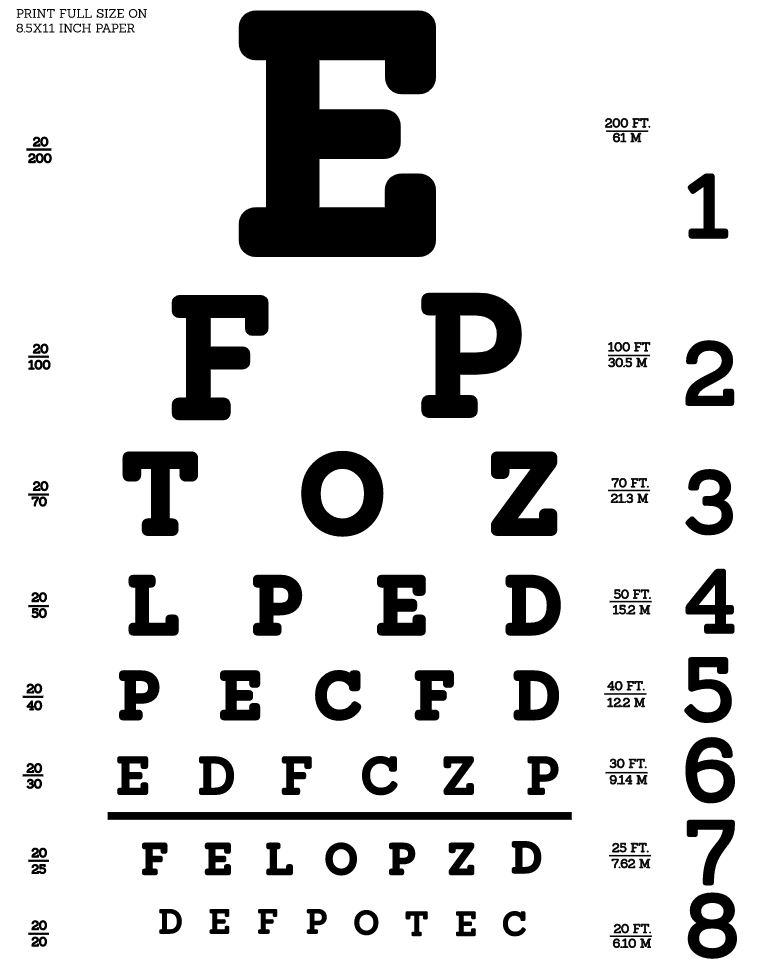
Snellen eye chart: used to test visual acuity
Image: “Snellen chart by Openclipart” by Openclipart. License: CC0 1.0Eye muscle, cranial nerve innervation, and muscle movement:
| Eye muscle | Cranial nerve innervation | Muscle movement |
|---|---|---|
| Superior rectus Superior rectus Orbit and Extraocular Muscles: Anatomy | Oculomotor (III) |
|
| Inferior rectus Inferior rectus Orbit and Extraocular Muscles: Anatomy | Oculomotor (III) |
|
| Medial rectus Medial rectus Orbit and Extraocular Muscles: Anatomy | Oculomotor (III) | Adduction Adduction Examination of the Upper Limbs |
| Inferior oblique Inferior oblique Orbit and Extraocular Muscles: Anatomy | Oculomotor (III) |
|
| Superior oblique Superior oblique Orbit and Extraocular Muscles: Anatomy | Trochlear (IV) |
|
| Lateral rectus Lateral rectus Orbit and Extraocular Muscles: Anatomy | Abducens (VI) | Abduction Abduction Examination of the Upper Limbs |
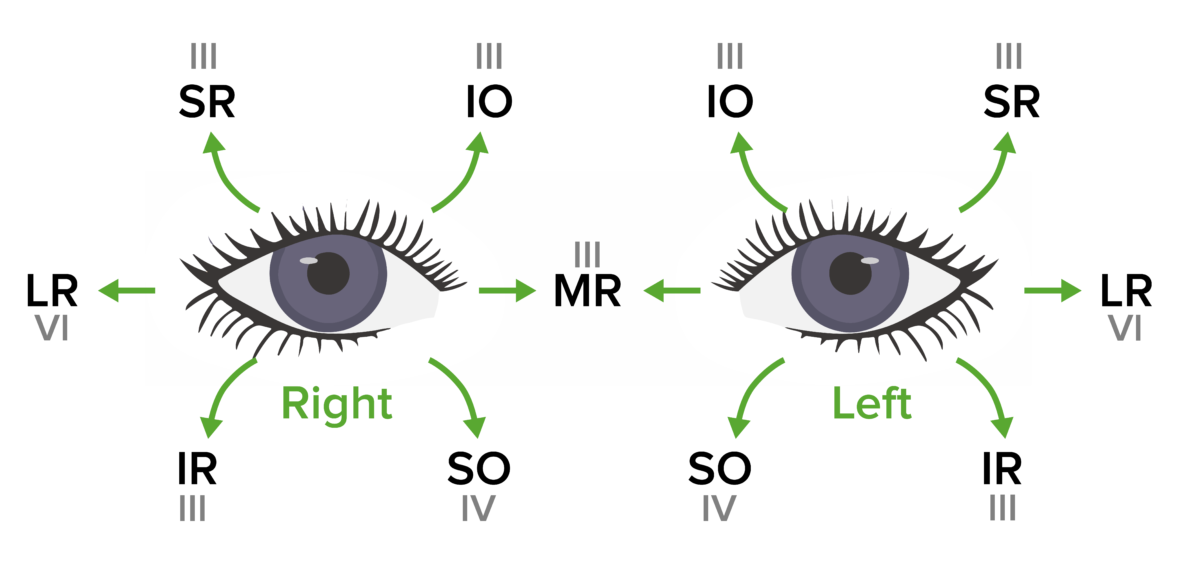
Cranial nerves III, IV, and VI: the innervated muscle and eye movement specific to each muscle
SR: superior rectus
IR: inferior rectus
MR: medial rectus
LR: lateral rectus
IO: inferior oblique
SO: superior oblique
Mnemonic

Nasal inspection
Image by Lecturio. License: CC BY-NC-SA 4.0
Pharyngeal inspection
Image by Lecturio. License: CC BY-NC-SA 4.0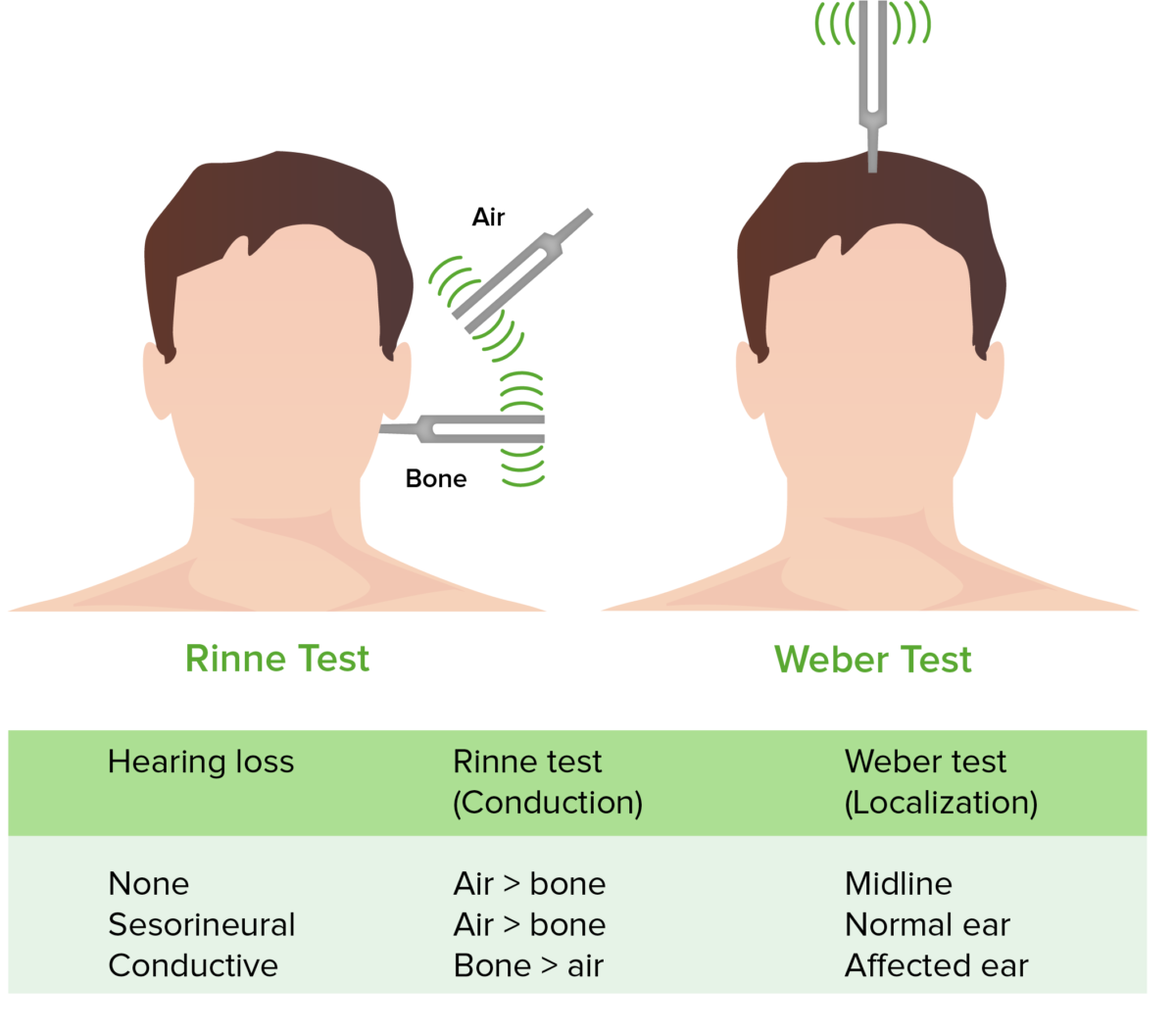
Rinne and Weber tests
Image by Lecturio. License: CC BY-NC-SA 4.0
Otoscope exam
Image by Lecturio. License: CC BY-NC-SA 4.0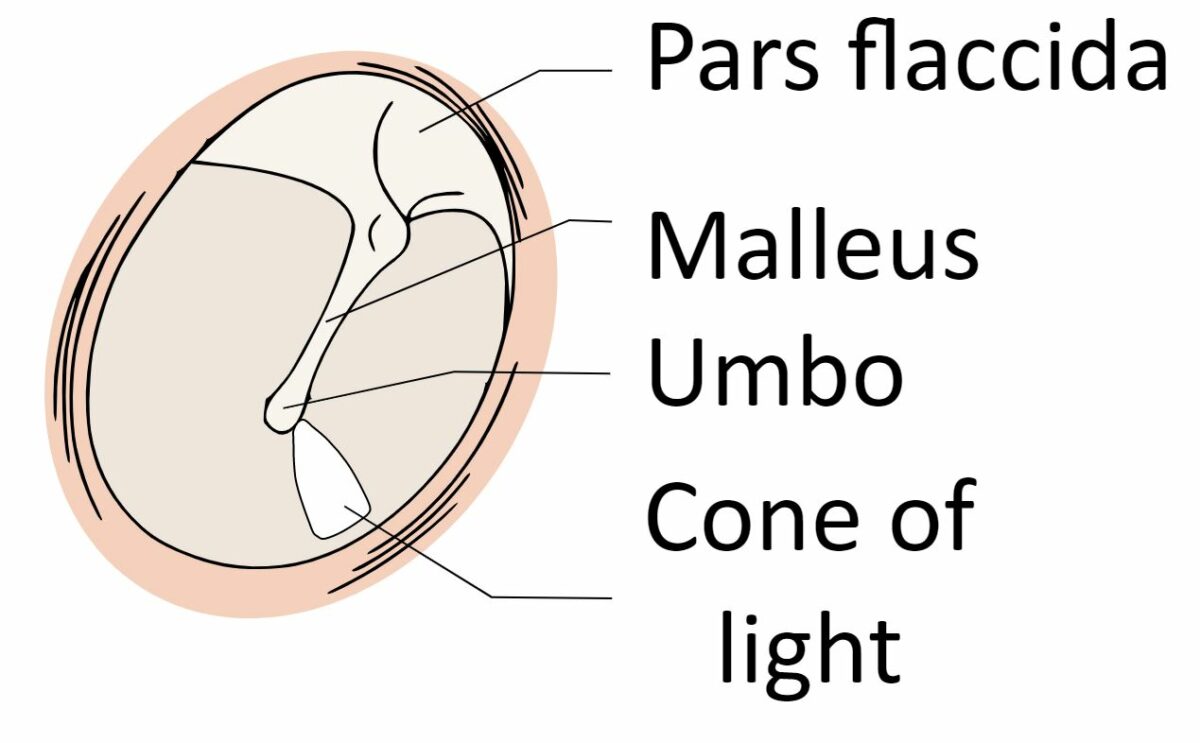
Schematic of the normal tympanic membrane
Image: “View-normal-tympanic-membrane” by Madhero88. License: CC BY 3.0Palpate the sinuses:

Palpation/percussion of the frontal sinuses
Image by Lecturio. License: CC BY-NC-SA 4.0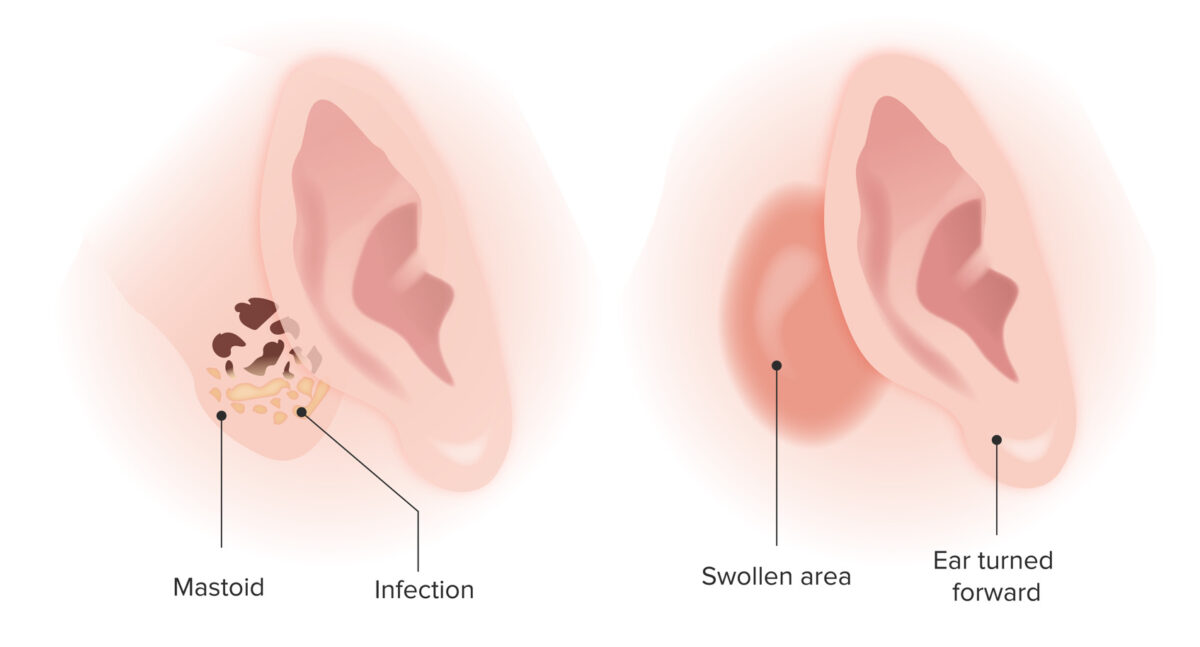
Mastoiditis
Image by Lecturio. License: CC BY-NC-SA 4.0
Examination of the floor of the mouth
Image by Lecturio. License: CC BY-NC-SA 4.0Palpate tracheal position:
Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy:

Goiter: Note the massive enlargement of the thyroid.
Image: “Iodine deficiency among goiter patients in rural South Sudan” by Chuot CC, Galukande M, Ibingira C, Kisa N, Fualal JO. License: CC BY 2.0Lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy of the head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess:
Enlarged and/or tender lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy ( lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy) may indicate:
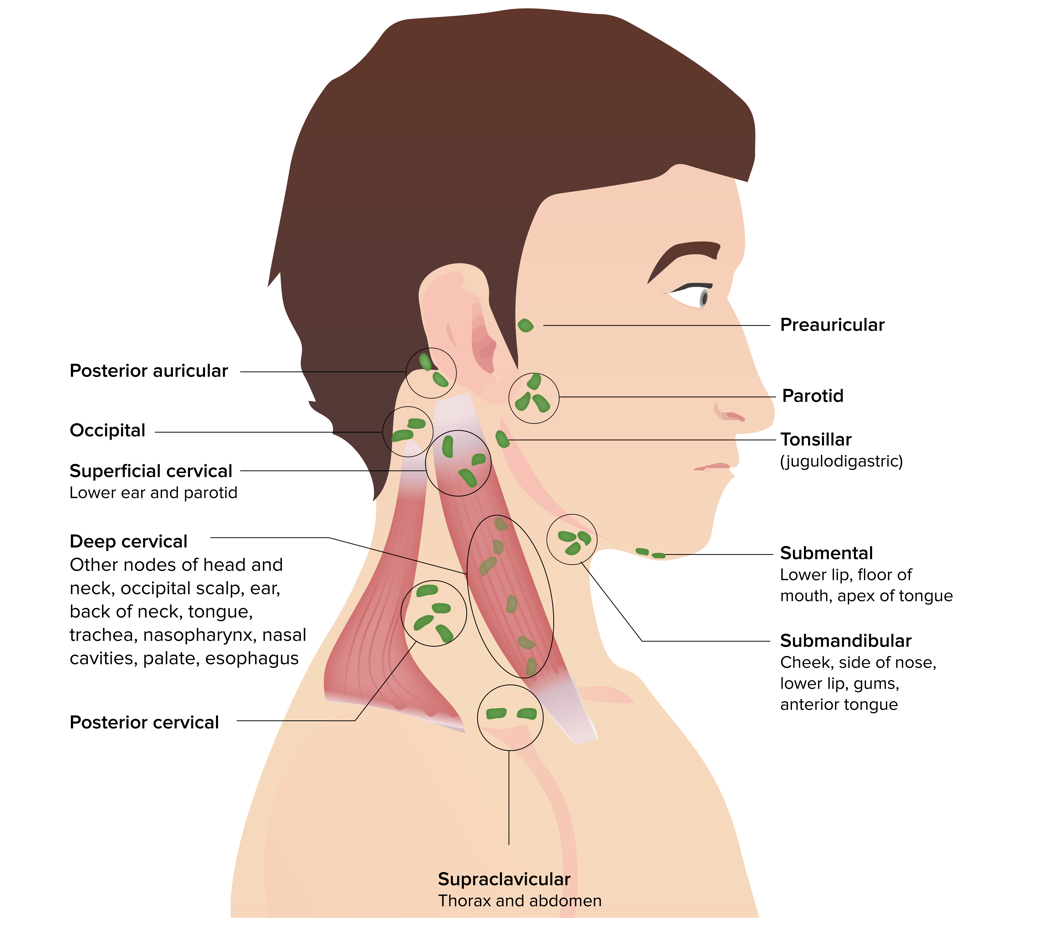
Head and neck lymph nodes
Image by Lecturio. License: CC BY-NC-SA 4.0| Level and nodal groups | Cancer sites of lymphatic spread |
|---|---|
| Submental and submandibular nodes |
|
| Upper jugulodigastric group |
|
| Middle jugular nodes |
|
| Inferior jugular nodes |
|
| Posterior triangle Posterior triangle Triangles of the Neck: Anatomy group | Back of skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy |
| Anterior compartment group |
|
| Cranial nerve | Examination |
|---|---|
| CN I: olfactory nerve Olfactory nerve The 1st cranial nerve. The olfactory nerve conveys the sense of smell. It is formed by the axons of olfactory receptor neurons which project from the olfactory epithelium (in the nasal epithelium) to the olfactory bulb. Nose Anatomy (External & Internal) |
|
| CN II: optic nerve Optic nerve The 2nd cranial nerve which conveys visual information from the retina to the brain. The nerve carries the axons of the retinal ganglion cells which sort at the optic chiasm and continue via the optic tracts to the brain. The largest projection is to the lateral geniculate nuclei; other targets include the superior colliculi and the suprachiasmatic nuclei. Though known as the second cranial nerve, it is considered part of the central nervous system. The 12 Cranial Nerves: Overview and Functions |
|
| CN III, IV, VI: oculomotor nerve Oculomotor nerve The 3D cranial nerve. The oculomotor nerve sends motor fibers to the levator muscles of the eyelid and to the superior rectus, inferior rectus, and inferior oblique muscles of the eye. It also sends parasympathetic efferents (via the ciliary ganglion) to the muscles controlling pupillary constriction and accommodation. The motor fibers originate in the oculomotor nuclei of the midbrain. The 12 Cranial Nerves: Overview and Functions, trochlear nerve Trochlear nerve The 4th cranial nerve. The trochlear nerve carries the motor innervation of the superior oblique muscles of the eye. The 12 Cranial Nerves: Overview and Functions, and abducens nerve Abducens nerve The 6th cranial nerve which originates in the abducens nucleus of the pons and sends motor fibers to the lateral rectus muscles of the eye. Damage to the nerve or its nucleus disrupts horizontal eye movement control. The 12 Cranial Nerves: Overview and Functions |
|
| CN V: trigeminal nerve Trigeminal nerve The 5th and largest cranial nerve. The trigeminal nerve is a mixed motor and sensory nerve. The larger sensory part forms the ophthalmic, mandibular, and maxillary nerves which carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth and from the teeth. Most of these fibers originate from cells of the trigeminal ganglion and project to the trigeminal nucleus of the brain stem. The smaller motor part arises from the brain stem trigeminal motor nucleus and innervates the muscles of mastication. The 12 Cranial Nerves: Overview and Functions |
|
| CN VII: facial nerve Facial nerve The 7th cranial nerve. The facial nerve has two parts, the larger motor root which may be called the facial nerve proper, and the smaller intermediate or sensory root. Together they provide efferent innervation to the muscles of facial expression and to the lacrimal and salivary glands, and convey afferent information for taste from the anterior two-thirds of the tongue and for touch from the external ear. The 12 Cranial Nerves: Overview and Functions |
|
| CN VIII: vestibulocochlear nerve Vestibulocochlear nerve The 8th cranial nerve. The vestibulocochlear nerve has a cochlear part (cochlear nerve) which is concerned with hearing and a vestibular part (vestibular nerve) which mediates the sense of balance and head position. The fibers of the cochlear nerve originate from neurons of the spiral ganglion and project to the cochlear nuclei (cochlear nucleus). The fibers of the vestibular nerve arise from neurons of scarpa’s ganglion and project to the vestibular nuclei. The 12 Cranial Nerves: Overview and Functions |
|
| CN IX, X: glossopharyngeal nerve Glossopharyngeal nerve The 9th cranial nerve. The glossopharyngeal nerve is a mixed motor and sensory nerve; it conveys somatic and autonomic efferents as well as general, special, and visceral afferents. Among the connections are motor fibers to the stylopharyngeus muscle, parasympathetic fibers to the parotid glands, general and taste afferents from the posterior third of the tongue, the nasopharynx, and the palate, and afferents from baroreceptors and chemoreceptor cells of the carotid sinus. Pharynx: Anatomy and vagus nerve Vagus nerve The 10th cranial nerve. The vagus is a mixed nerve which contains somatic afferents (from skin in back of the ear and the external auditory meatus), visceral afferents (from the pharynx, larynx, thorax, and abdomen), parasympathetic efferents (to the thorax and abdomen), and efferents to striated muscle (of the larynx and pharynx). Pharynx: Anatomy |
|
| CN XI: accessory nerve |
|
| CN XII: hypoglossal nerve Hypoglossal nerve The 12th cranial nerve. The hypoglossal nerve originates in the hypoglossal nucleus of the medulla and supplies motor innervation to all of the muscles of the tongue except the palatoglossus (which is supplied by the vagus). This nerve also contains proprioceptive afferents from the tongue muscles. Lips and Tongue: Anatomy |
|
| Region | Findings | Possible cause |
|---|---|---|
| Face |
|
|
| Neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess |
|
|
| Eyes |
|
|
| Mouth |
|
|