The pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland, also known as the hypophysis, is considered the “master endocrine gland” because it releases hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types that regulate the activity of multiple major endocrine organs in the body. The gland sits on the sella turcica, just below the hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus, which is the primary regulator of the pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland. The pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland has 2 lobes: the anterior lobe Anterior lobe Cerebellum: Anatomy (the adenohypophysis) and the posterior lobe Posterior lobe Cerebellum: Anatomy (the neurohypophysis). Each lobe has its own regulation, set of secretory products, and feedback loops. Abnormalities in the pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland can lead to a wide range of clinical conditions, some of which include hyperprolactinemia Hyperprolactinemia Hyperprolactinemia is defined as a condition of elevated levels of prolactin (PRL) hormone in the blood. The PRL hormone is secreted by the anterior pituitary gland and is responsible for breast development and lactation. The most common cause is PRL-secreting pituitary adenomas (prolactinomas). Hyperprolactinemia, acromegaly Acromegaly A condition caused by prolonged exposure to excessive human growth hormone in adults. It is characterized by bony enlargement of the face; lower jaw (prognathism); hands; feet; head; and thorax. The most common etiology is a growth hormone-secreting pituitary adenoma. Acromegaly and Gigantism, hyperthyroidism Hyperthyroidism Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate. Thyrotoxicosis and Hyperthyroidism or hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto's disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism, and central diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus insipidus.
Last updated: Nov 19, 2024
The pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland is known as the “master endocrine gland.” This gland receives stimulatory input from the hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus and secretes multiple different hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types, which target multiple different end organs and have wide-ranging effects throughout the body.
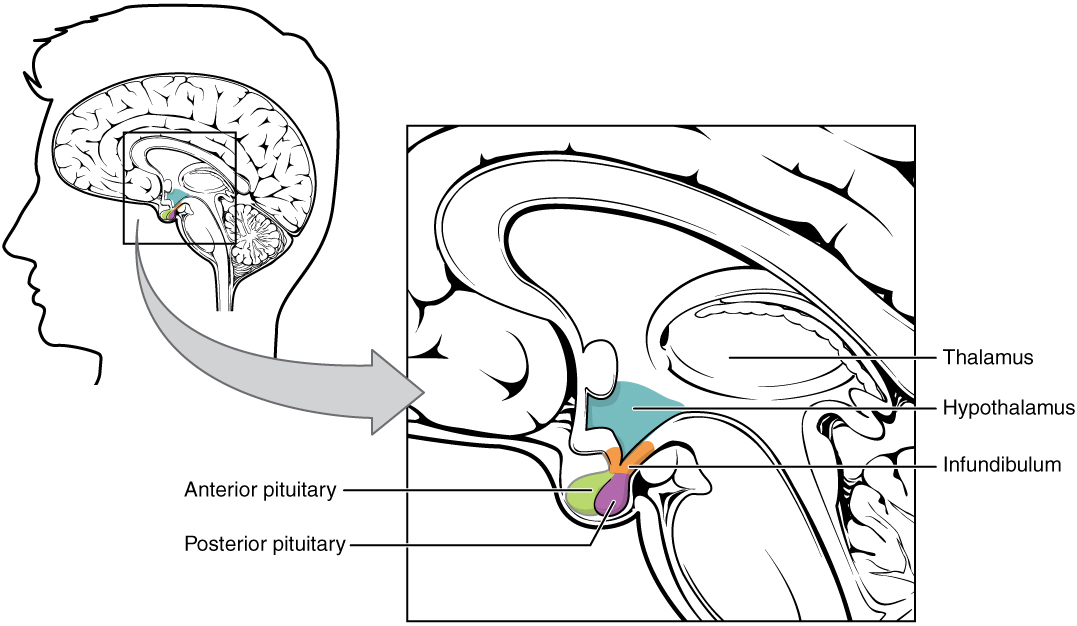
Hypothalamic–pituitary complex:
The image shows the pituitary gland, made up of the anterior and posterior lobes, in relation to the hypothalamus.
The pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland is divided into 2 primary components:
The 2 halves function independently, as 2 separate glands, each with their own:
Anterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types:
Posterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types:
Major components of the pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland include:
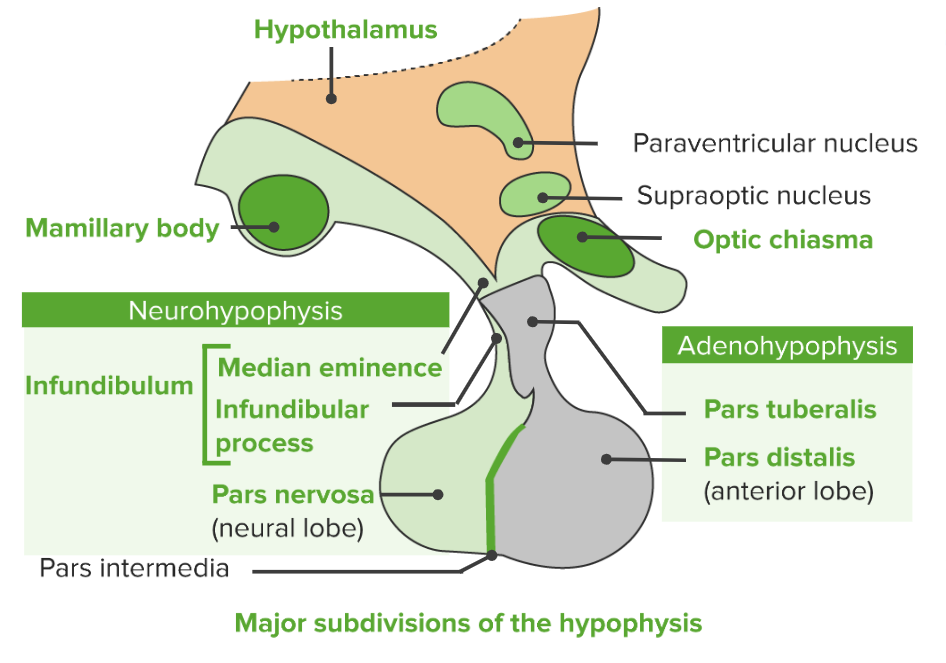
Major subdivisions of the pituitary gland (hypophysis)
Image by Lecturio.Adenohypophysis/anterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types: via the hypothalamohypophyseal portal system (i.e., connected via the circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment):
Neurohypophysis/posterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types: via the hypothalamohypophyseal tract (i.e., directly connected via the nerves)
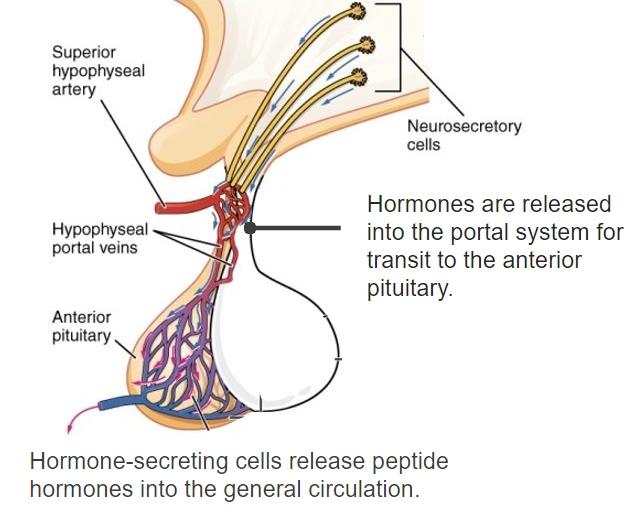
Diagram of the hypothalamohypophyseal portal system connecting the hypothalamus and the anterior pituitary
Image: “The hypothalamus produces separate hormones that stimulate or inhibit hormone production in the anterior pituitary” by OpenStax College. License: CC BY 4.0, edited by Lecturio.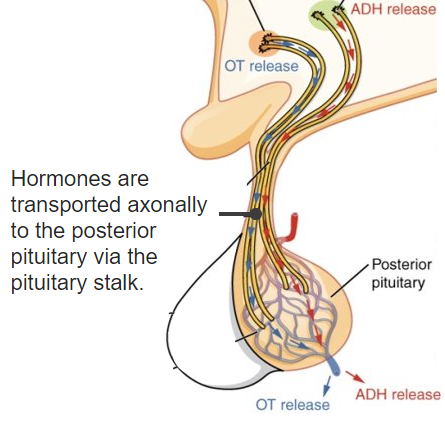
Diagram of the nerve connections between the hypothalamus and the posterior pituitary gland
ADH: antidiuretic hormone
OT: oxytocin
General characteristics:
Chromophils:
Chromophobes:
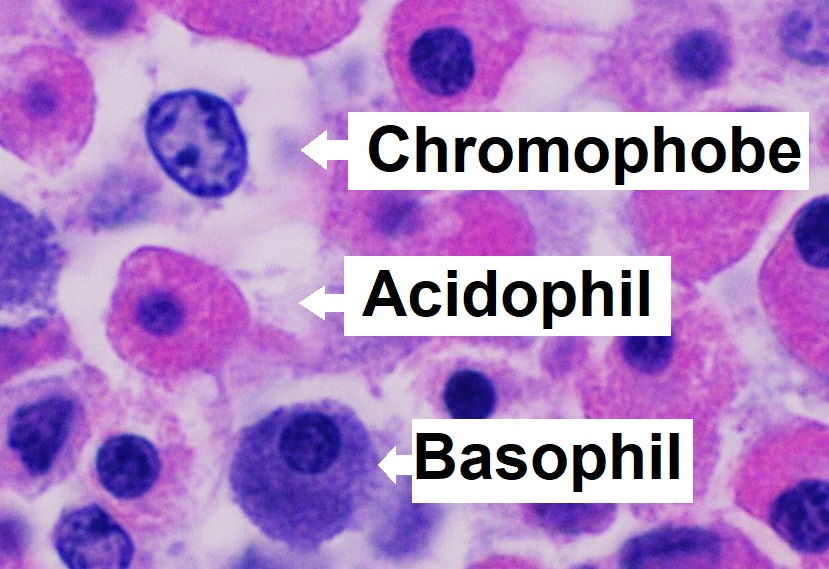
Microanatomy of the pars distalis in the anterior lobe of the pituitary gland showing chromophobes, basophils, and acidophils
Image: “Microanatomy of the pars distalis showing chromophobes, basophils, and acidophils” by Mikael Häggström. License: CC0 1.0The neurohypophysis is filled with the terminal axons Axons Nerve fibers that are capable of rapidly conducting impulses away from the neuron cell body. Nervous System: Histology of neurosecretory cells, supporting cells known as pituicytes, and dense networks of fenestrated capillaries Fenestrated capillaries Wall contains multiple fenestrations, or “pores”, with continuous basal lamina. Capillaries: Histology.
Both the anterior and posterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types drain into:
The pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland’s primary function is to secrete a variety of regulatory hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types.
Hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types secreted by the anterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types affect many of the other major endocrine glands Endocrine glands Ductless glands that secrete hormones directly into the blood circulation. These hormones influence the metabolism and other functions of cells in the body. Glandular Epithelium: Histology in the body. Hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types are part of complex regulatory systems known as “axes.” These axes are summarized in the table below.
| Hypothalamic hormone | Pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types target cell | Pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types hormone | Target organ | End effects |
|---|---|---|---|---|
| Corticotropin-releasing hormone Corticotropin-releasing hormone A peptide of about 41 amino acids that stimulates the release of adrenocorticotropic hormone. Crh is synthesized by neurons in the paraventricular nucleus of the hypothalamus. After being released into the pituitary portal circulation, crh stimulates the release of acth from the pituitary gland. Crh can also be synthesized in other tissues, such as placenta; adrenal medulla; and testis. Hypothalamic and Pituitary Hormones (CRH) | Corticotropes | ACTH | Adrenal cortex Adrenal Cortex The outer layer of the adrenal gland. It is derived from mesoderm and comprised of three zones (outer zona glomerulosa, middle zona fasciculata, and inner zona reticularis) with each producing various steroids preferentially, such as aldosterone; hydrocortisone; dehydroepiandrosterone; and androstenedione. Adrenal cortex function is regulated by pituitary adrenocorticotropin. Adrenal Glands: Anatomy | Release of corticosteroids Corticosteroids Chorioretinitis |
| Thyrotropin-releasing hormone Thyrotropin-releasing hormone A tripeptide that stimulates the release of thyrotropin and prolactin. It is synthesized by the neurons in the paraventricular nucleus of the hypothalamus. After being released into the pituitary portal circulation, TRH stimulates the release of TSH and PRL from the anterior pituitary gland. Hypothalamic and Pituitary Hormones (TRH) | Thyrotropes | TSH | Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland | Release of thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types |
| Gonadotropin-releasing hormone Gonadotropin-releasing hormone A decapeptide that stimulates the synthesis and secretion of both pituitary gonadotropins, luteinizing hormone and follicle stimulating hormone. Gnrh is produced by neurons in the septum preoptic area of the hypothalamus and released into the pituitary portal blood, leading to stimulation of gonadotrophs in the anterior pituitary gland. Puberty (GnRH) | Gonadotropes | FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle |
|
Development of ovarian follicles and sperm production |
| LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle |
|
|
||
| Growth hormone–releasing hormone ( GHRH GHRH A peptide of 44 amino acids in most species that stimulates the release and synthesis of growth hormone. GHRF (or GRF) is synthesized by neurons in the arcuate nucleus of the hypothalamus. After being released into the pituitary portal circulation, GHRF stimulates gh release by the somatotrophs in the pituitary gland. Hypothalamic and Pituitary Hormones) | Somatotropes | GH | Many organs | Anabolic effects |
| Somatostatin Somatostatin A 14-amino acid peptide named for its ability to inhibit pituitary growth hormone release, also called somatotropin release-inhibiting factor. It is expressed in the central and peripheral nervous systems, the gut, and other organs. SRIF can also inhibit the release of thyroid-stimulating hormone; prolactin; insulin; and glucagon besides acting as a neurotransmitter and neuromodulator. In a number of species including humans, there is an additional form of somatostatin, srif-28 with a 14-amino acid extension at the n-terminal. Gastrointestinal Secretions (inhibitor) | Somatotropes | GH (inhibited) | Many organs | Anabolic effects inhibited with somatostatin Somatostatin A 14-amino acid peptide named for its ability to inhibit pituitary growth hormone release, also called somatotropin release-inhibiting factor. It is expressed in the central and peripheral nervous systems, the gut, and other organs. SRIF can also inhibit the release of thyroid-stimulating hormone; prolactin; insulin; and glucagon besides acting as a neurotransmitter and neuromodulator. In a number of species including humans, there is an additional form of somatostatin, srif-28 with a 14-amino acid extension at the n-terminal. Gastrointestinal Secretions |
| Dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS (inhibitor) | Lactotropes | Prolactin Prolactin A lactogenic hormone secreted by the adenohypophysis. It is a polypeptide of approximately 23 kd. Besides its major action on lactation, in some species prolactin exerts effects on reproduction, maternal behavior, fat metabolism, immunomodulation and osmoregulation. Breasts: Anatomy (inhibited) | Mammary glands | Milk production inhibited with dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS |
The 2 major posterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types are ADH and oxytocin, which are not involved in regulatory axes the way the anterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types are. These hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types act directly on end target organs.
| Hormone | Synthesis Synthesis Polymerase Chain Reaction (PCR) | Target organ | Function |
|---|---|---|---|
| Antidiuretic hormone Antidiuretic hormone Antidiuretic hormones released by the neurohypophysis of all vertebrates (structure varies with species) to regulate water balance and osmolarity. In general, vasopressin is a nonapeptide consisting of a six-amino-acid ring with a cysteine 1 to cysteine 6 disulfide bridge or an octapeptide containing a cystine. All mammals have arginine vasopressin except the pig with a lysine at position 8. Vasopressin, a vasoconstrictor, acts on the kidney collecting ducts to increase water reabsorption, increase blood volume and blood pressure. Hypernatremia (ADH) | Supraoptic nuclei of hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus | Kidney |
|
| Oxytocin | Paraventricular nuclei of hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus | Breast | Stimulates milk ejection Milk ejection Expulsion of milk from the mammary alveolar lumen, which is surrounded by a layer of milk-secreting epithelial cells and a network of myoepithelial cells. Contraction of the myoepithelial cells is regulated by neuroendocrine signals. Breastfeeding during lactation Lactation The processes of milk secretion by the maternal mammary glands after parturition. The proliferation of the mammary glandular tissue, milk synthesis, and milk expulsion or let down are regulated by the interactions of several hormones including estradiol; progesterone; prolactin; and oxytocin. Breastfeeding |
| Uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy | Stimulates uterine contractions during labor |