Mineralocorticoids are a drug class within the corticosteroid family and fludrocortisone is the primary medication within this class. Fludrocortisone is a fluorinated analog of cortisone Cortisone A naturally occurring glucocorticoid that has been used in replacement therapy for adrenal insufficiency and as an anti-inflammatory agent. Cortisone itself is inactive; it is converted in the liver to the active metabolite hydrocortisone. Glucocorticoids. The fluorine moiety protects the drug from isoenzyme inactivation in the kidney, allowing it to exert its mineralocorticoid effect. The mechanism of action of mineralocorticoids mimics that of aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia. By acting on the mineralocorticoid receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors, fludrocortisone induces the expression of proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis responsible for Na+ reabsorption and K+ excretion by renal tubule cells, which results in Na+ and water retention. Mineralocorticoids are used in the management of diseases characterized by insufficient (or absent) aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia activity, such as adrenal insufficiency Adrenal Insufficiency Conditions in which the production of adrenal corticosteroids falls below the requirement of the body. Adrenal insufficiency can be caused by defects in the adrenal glands, the pituitary gland, or the hypothalamus. Adrenal Insufficiency and Addison Disease and congenital adrenal hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation. Adverse effects are related to both mineralocorticoid and glucocorticoid effects and include hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema, decompensated heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), hyperpigmentation Hyperpigmentation Excessive pigmentation of the skin, usually as a result of increased epidermal or dermal melanin pigmentation, hypermelanosis. Hyperpigmentation can be localized or generalized. The condition may arise from exposure to light, chemicals or other substances, or from a primary metabolic imbalance. Malassezia Fungi, hypokalemia Hypokalemia Hypokalemia is defined as plasma potassium (K+) concentration < 3.5 mEq/L. Homeostatic mechanisms maintain plasma concentration between 3.5-5.2 mEq/L despite marked variation in dietary intake. Hypokalemia can be due to renal losses, GI losses, transcellular shifts, or poor dietary intake. Hypokalemia, Cushing syndrome Cushing syndrome A condition caused by prolonged exposure to excess levels of cortisol (hydrocortisone) or other glucocorticoids from endogenous or exogenous sources. It is characterized by upper body obesity; osteoporosis; hypertension; diabetes mellitus; hirsutism; amenorrhea; and excess body fluid. Endogenous Cushing syndrome or spontaneous hypercortisolism is divided into two groups, those due to an excess of adrenocorticotropin and those that are acth-independent. Paraneoplastic Syndromes, hyperglycemia Hyperglycemia Abnormally high blood glucose level. Diabetes Mellitus, and hypothalamic-pituitary-adrenal axis Hypothalamic-pituitary-adrenal axis Adrenal Hormones suppression Suppression Defense Mechanisms.
Last updated: Feb 7, 2025
Fludrocortisone is the primary drug in this class.
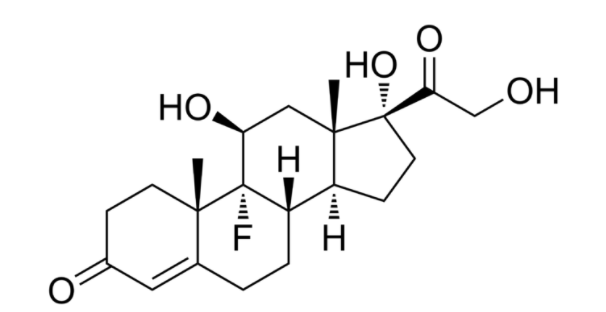
Chemical structure of fludrocortisone: Notice the similarity to cortisone, except for the presence of the fluorine atom within the steroid ring structure.
Image: “Chemical structure of fludrocortisone” by Edgar181. License: Public Domain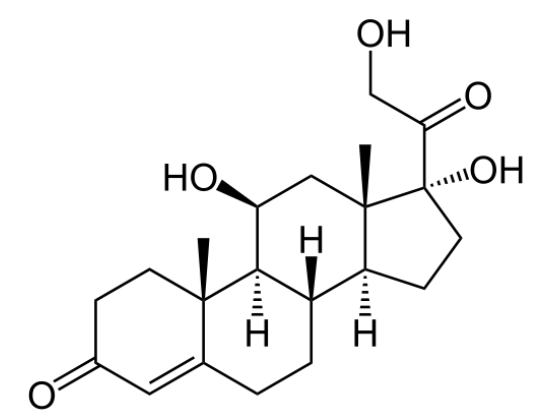
Chemical structure of cortisol
Image: “Structure of Cortisol” by NEUROtiker. License: Public Domain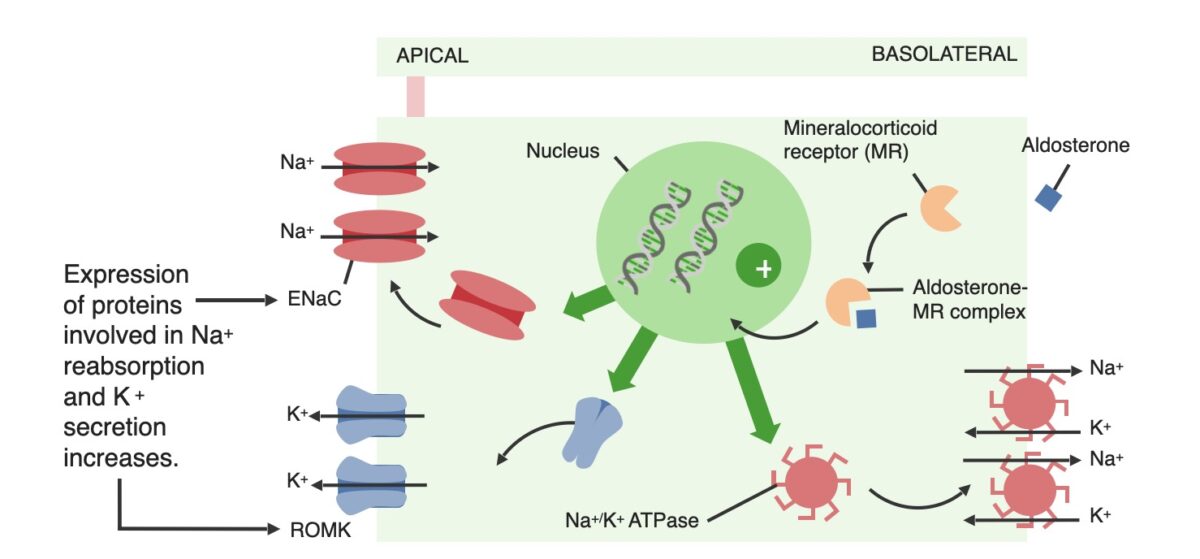
Effects of aldosterone on the principal cells within the distal renal tubules. Mineralocorticoids work similarly.
ENaC: epithelial Na+ channel
ROMK: renal outer medullary potassium
Although fludrocortisone has glucocorticoid activity, it is primarily used for its mineralocorticoid activity (particularly in conditions with inadequate aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia production).
There are many side effects of fludrocortisone therapy, notably: