Membranoproliferative glomerulonephritis (MPGN) is also known as mesangiocapillary glomerulonephritis. Membranoproliferative glomerulonephritis is a pattern of glomerular injury characterized by mesangial hypercellularity, endocapillary proliferation, and thickening of the glomerular basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN) (double contour formation). The changes are due to the deposition of Igs Igs Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions, complement factors, or both, in the glomerular mesangium Mesangium The thin membranous structure supporting the adjoining glomerular capillaries. It is composed of glomerular mesangial cells and their extracellular matrix. IgA Nephropathy and along the glomerular capillary walls. The pathogenic variants include immune complex/monoclonal Ig-mediated (e.g., from infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, autoimmune diseases Autoimmune diseases Disorders that are characterized by the production of antibodies that react with host tissues or immune effector cells that are autoreactive to endogenous peptides. Selective IgA Deficiency) and complement-mediated MPGN. In rare cases, MPGN is not associated with Igs Igs Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions and the complement system Complement system Serum glycoproteins participating in the host defense mechanism of complement activation that creates the complement membrane attack complex. Included are glycoproteins in the various pathways of complement activation (classical complement pathway; alternative complement pathway; and lectin complement pathway). Innate Immunity: Barriers, Complement, and Cytokines, such as in the case of endothelial injury. With multiple etiologies, the presentation and clinical course vary. Presenting features can be asymptomatic proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children and hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma, nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome, nephritic syndrome Nephritic syndrome Nephritic syndrome is a broad category of glomerular diseases characterized by glomerular hematuria, variable loss of renal function, and hypertension. These features are in contrast to those of nephrotic syndrome, which includes glomerular diseases characterized by severe proteinuria, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephritic Syndrome, or chronic renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome. Definitive diagnosis requires renal biopsy Renal Biopsy Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis, although additional laboratory and imaging tests may point to the associated disease. Treatment is based on the underlying cause. Steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors, immunosuppressants Immunosuppressants Immunosuppressants are a class of drugs widely used in the management of autoimmune conditions and organ transplant rejection. The general effect is dampening of the immune response. Immunosuppressants, and kidney transplantation Kidney Transplantation The transference of a kidney from one human or animal to another. Organ Transplantation are among the commonly used treatment modalities.
Last updated: May 17, 2024
Membranoproliferative glomerulonephritis (MPGN) is a glomerular injury characterized by glomerular basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN) (GBM) thickening (“membrano-”) and increased endocapillary and mesangial cellularity (“proliferative”).
Traditionally, MPGN was classified based on electron microscopy findings (old classification):
A different classification based on the pathogenetic process helps point to the underlying etiology or disease, thus directing treatment.
| Immune complex/monoclonal Ig-mediated MPGN | Complement-mediated MPGN | MPGN with no Ig Ig X-linked Agammaglobulinemia or complement | |
|---|---|---|---|
| LM | “Tram tracking” (double contouring) of basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN) | ||
| IM |
|
Complement positive and no (or minimal) staining for Ig Ig X-linked Agammaglobulinemia | No Ig Ig X-linked Agammaglobulinemia or complement staining |
| EM | Subendothelial and mesangial deposits (in some autoimmune diseases Autoimmune diseases Disorders that are characterized by the production of antibodies that react with host tissues or immune effector cells that are autoreactive to endogenous peptides. Selective IgA Deficiency, + subepithelial deposits) |
|
No electron-dense deposits along the capillary walls |
| Differential diagnosis |
|
|
Endothelial injury, which can be from:
|
| Etiology | Microscopic findings | |
|---|---|---|
| Immune complex/monoclonal Ig-mediated MPGN | Hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus or C (or other viral infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease) |
|
| Monoclonal gammopathy Monoclonal gammopathy Conditions characterized by the presence of m protein (monoclonal protein) in serum or urine without clinical manifestations of plasma cell dyscrasia. MALT Lymphoma | Kappa OR lambda light chains Light chains Polypeptide chains, consisting of 211 to 217 amino acid residues and having a molecular weight of approximately 22 kda. There are two major types of light chains, kappa and lambda. Two ig light chains and two ig heavy chains (immunoglobulin heavy chains) make one immunoglobulin molecule. Immunoglobulins: Types and Functions | |
| Autoimmune diseases Autoimmune diseases Disorders that are characterized by the production of antibodies that react with host tissues or immune effector cells that are autoreactive to endogenous peptides. Selective IgA Deficiency | “Full-house pattern”:
|
|
| Complement-mediated MPGN | C3 glomerulopathy |
|
| C4 glomerulopathy |
|
|
| MPGN not associated with complement or Ig Ig X-linked Agammaglobulinemia deposition | Microangiopathies (commonly associated with endothelial injury) | No significant Ig Ig X-linked Agammaglobulinemia or complement deposition seen |
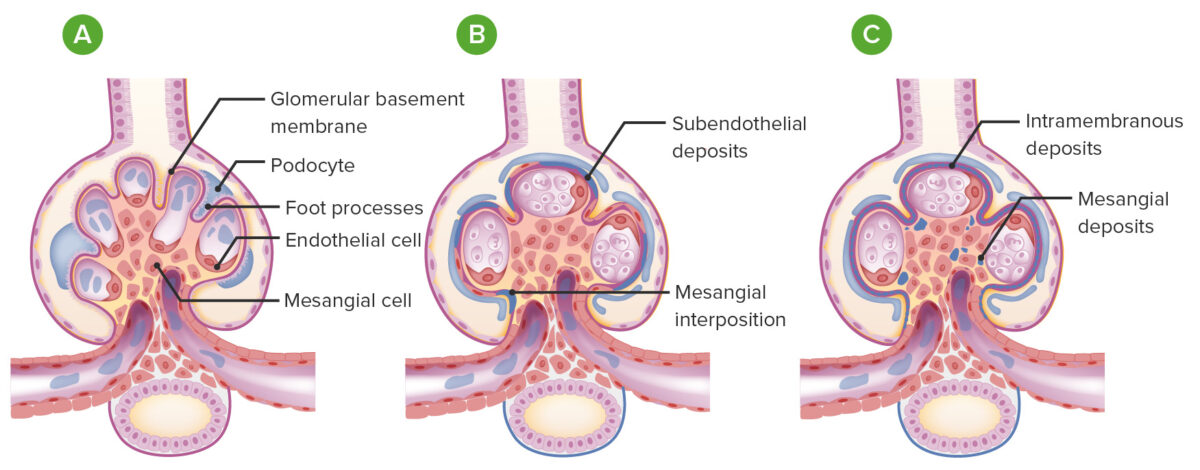
Membranoproliferative glomerulonephritis (MPGN) vs normal glomeruli:
A: normal glomerulus (with open capillary loops, ≤ 3 nuclei in each mesangial area, intact foot processes, and no deposits or proliferation)
B: MPGN: Glomeruli become lobulated with endocapillary proliferation and the glomerular basement membrane has a split appearance (from subendothelial deposits and mesangial interposition).
C: MPGN with mesangial deposits and intramembranous deposits (as seen in dense deposit disease)
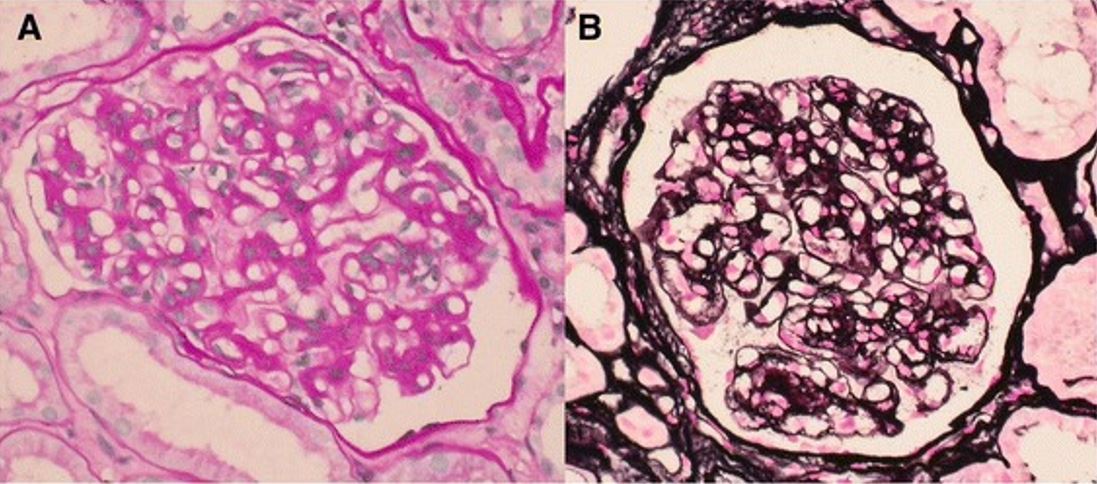
Light microscopic features of membranoproliferative glomerulonephritis
A: Mesangium is expanded and the glomerular capillary walls appear thickened (periodic acid-Schiff).
B: Glomerular capillary walls exhibit thickened and segmental double contours (methenamine silver).
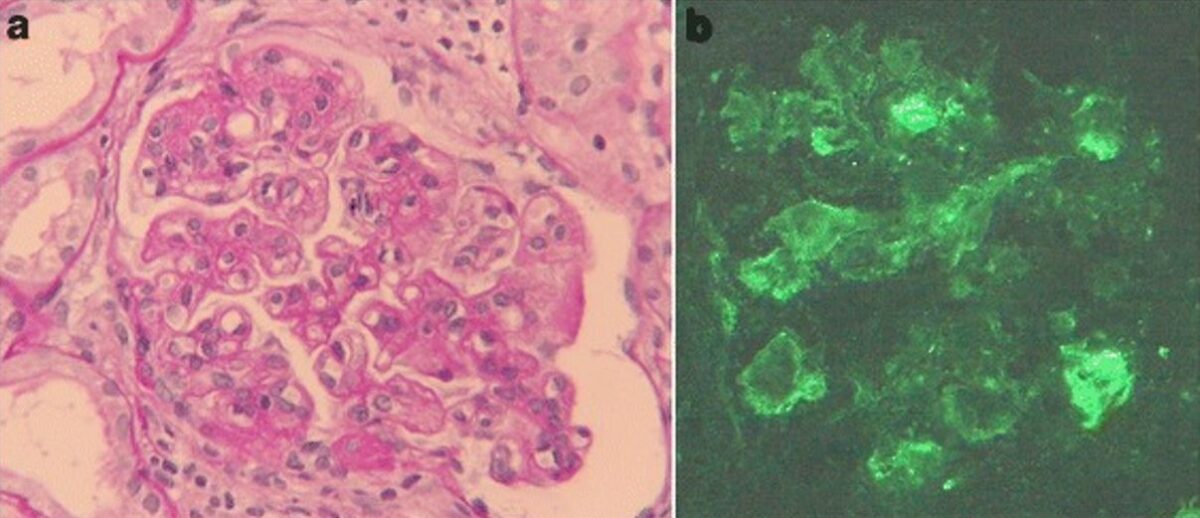
Membranoproliferative glomerulonephritis associated with hepatitis C
a: light microscopy findings of kidney biopsy: Periodic acid-Schiff staining reveals mesangial hypercellularity, lobular accentuation, and double contour of the basement membrane (original magnification, ×400).
b: Immunofluorescence staining of IgM is positive along the capillary loop (original magnification, ×400).
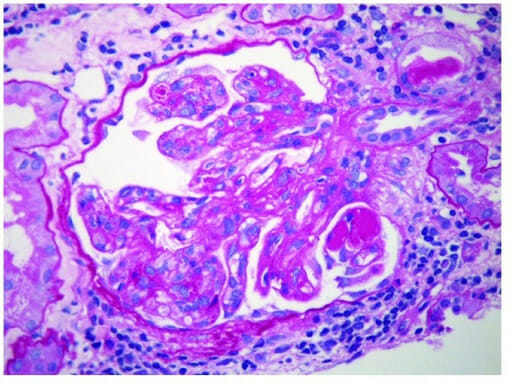
Membranoproliferative glomerulonephritis:
Endocapillary proliferation with extensive subendothelial deposits along the glomerular capillary walls. Mesangial deposits are also present (electron microscopy).
Additional workup is indicated when biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma shows changes consistent with: