IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions nephropathy (Berger's disease) is a renal disease characterized by IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions deposition in the mesangium. It is the most common cause of primary glomerulonephritis in most developed countries. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship frequently present in the second and third decades of life and, historically, with a preceding upper respiratory or GI infection GI infection Microsporidia/Microsporidiosis. Common presenting features are gross hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma or asymptomatic, microscopic hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma on urinalysis Urinalysis Examination of urine by chemical, physical, or microscopic means. Routine urinalysis usually includes performing chemical screening tests, determining specific gravity, observing any unusual color or odor, screening for bacteriuria, and examining the sediment microscopically. Urinary Tract Infections (UTIs) in Children. The course is often benign Benign Fibroadenoma, with the definitive diagnostic procedure, renal biopsy Renal Biopsy Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis, performed only in cases of severe, progressive renal disease. Treatment depends on the severity of proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children, renal function, and pathologic changes. ACE inhibitors ACE inhibitors Truncus Arteriosus or angiotensin-receptor blockers ( ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Angina Medication) are given to reduce disease progression. Persistent proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children and increasing creatinine are indications for immunosuppressive therapy that includes glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids and, possibly, cytotoxic Cytotoxic Parvovirus B19 agents.
Last updated: May 17, 2024
IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions nephropathy (Berger’s disease) is a renal disease characterized by IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions deposition in the mesangium, causing glomerular inflammation Glomerular Inflammation Nephritic Syndrome in Children (glomerulonephritis (GN)).
IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions nephropathy presents with recurrent gross hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma or asymptomatic microscopic hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma as the most common manifestations.
The diagnosis is usually based on the clinical presentation and suspicion arising from a preceding infectious event.
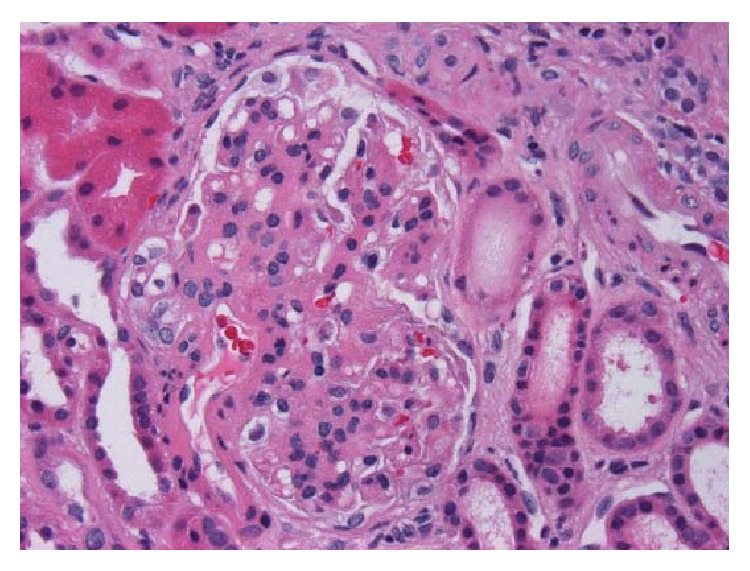
Micrograph of IgA nephropathy: a glomerulus with thickened mesangium and segmental mesangial hypercellularity
Image: “IgA Nephropathy in a Patient Presenting with Pseudotumor Cerebri” by Ahmed US, Bacaj P, Iqbal HI, Onder S. License: CC BY 4.0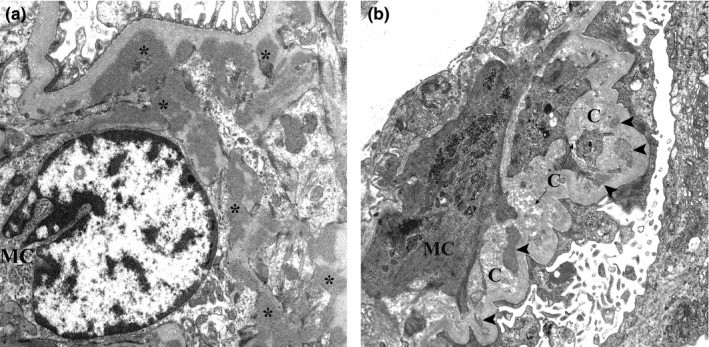
(a): IgA nephropathy: Several electron-dense mesangial deposits (asterisks) are shown. These deposits lack the electron‐lucent halo.
(b): chronic IgA nephropathy: Mesangial deposits with varying degrees of resorption (arrowheads) close to collagen fibers are evident.
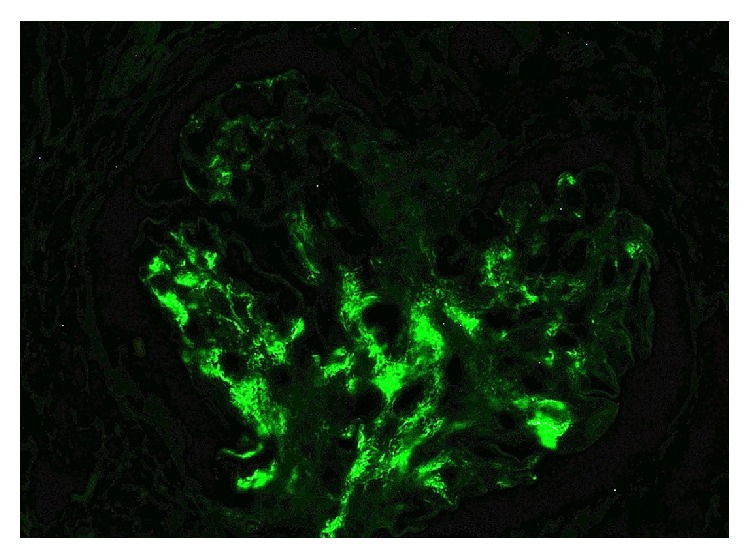
IgA nephropathy: immunofluorescence demonstrating positivity for IgA
Image: “IgA Nephropathy in a Patient Presenting with Pseudotumor Cerebri” by Ahmed US, Bacaj P, Iqbal HI, Onder S. License: CC BY 4.0The following conditions are among the differential diagnoses for IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions nephropathy.