Henoch-Schönlein purpura (HSP), also known as immunoglobulin A vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus, is an autoimmune small-vessel vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus that typically presents as a tetrad of abdominal pain Abdominal Pain Acute Abdomen, arthralgia Arthralgia Pain in the joint. Rheumatic Fever, hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma, and purpuric rash Rash Rocky Mountain Spotted Fever. The pathophysiology involves the deposition of IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions immune complexes Immune complexes The complex formed by the binding of antigen and antibody molecules. The deposition of large antigen-antibody complexes leading to tissue damage causes immune complex diseases. C3 Deficiency in multiple vessels following a trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation (infection/environmental), and the symptoms depend on the tissues that are involved. The diagnosis is established clinically, but can be supported with laboratory studies and skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions or kidney biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Management is mostly supportive, but may involve steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors and immunosuppressants Immunosuppressants Immunosuppressants are a class of drugs widely used in the management of autoimmune conditions and organ transplant rejection. The general effect is dampening of the immune response. Immunosuppressants in more severe cases. Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is usually excellent, but some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may develop end-stage renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome.
Last updated: Jun 19, 2025
Henoch-Schönlein purpura (HSP) is an immunoglobulin A ( IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions)-mediated small-vessel vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus.

Hallmark purpuric rash of Henoch-Schönlein purpura
Image: “Purpura Schönlein-Henoch” by Mnokel. License: Public Domain
Purpura evident on the distal extremities of a pediatric patient with Henoch-Schönlein purpura
Image: “Purpura2” by Okwikikim. License: Public DomainLaboratory workup is used to rule out differentials and evaluate complications.
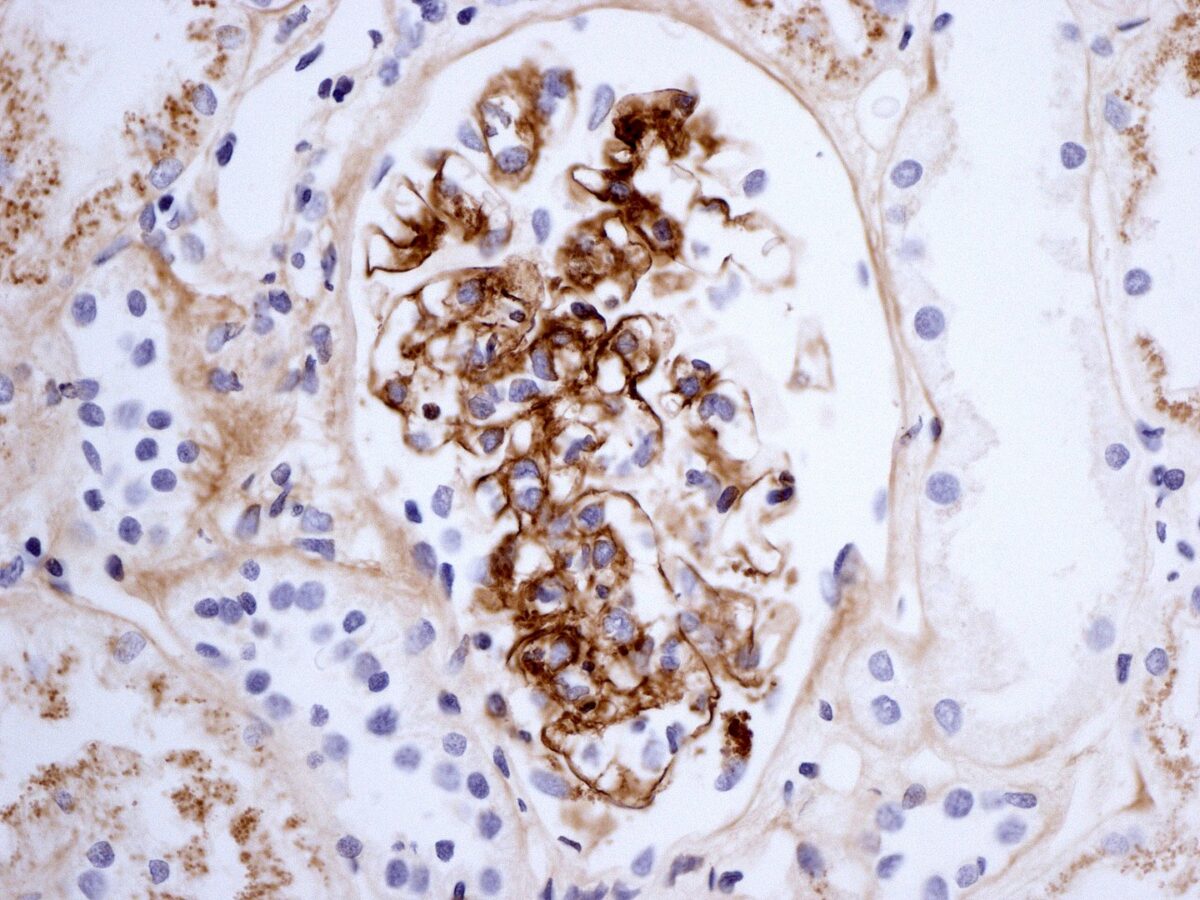
Renal biopsy in Henoch-Schönlein purpura showing immunostaining for IgA
Image: “Henoch-Schönlein nephritis IgA immunostaining” by Lazarus Karamadoukis, Linmarie Ludeman, and Anthony J Williams. License: CC BY 2.0Imaging is used for complicated presentations.

Target sign typical of intussusception on abdominal ultrasound
Image: “Pelvic plastron secondary to acute appendicitis in a child presented as appendiceal intussusception. A case report” by Christianakis E, Sakelaropoulos A, Papantzimas C, Pitiakoudis M, Filippou G, Filippou D, Rizos S, Paschalidis N. License: CC BY 2.0