Leukoplakia is a potentially malignant lesion affecting the squamous epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology usually within the oral cavity. Leukoplakia can be associated with a history of chronic tobacco and alcohol use, both of which can synergistically damage the epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology. Leukoplakia presents as a white plaque Plaque Primary Skin Lesions that cannot be scraped off. Diagnosis is confirmed with a biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. The lesion can be surgically treated, but close observation is always recommended owing to the risk of malignant transformation Transformation Change brought about to an organism's genetic composition by unidirectional transfer (transfection; transduction, genetic; conjugation, genetic, etc.) and incorporation of foreign DNA into prokaryotic or eukaryotic cells by recombination of part or all of that DNA into the cell's genome. Bacteriology.
Last updated: May 21, 2025
Risk factors are similar to those for squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC).
This form is less likely to be malignant and is characterized by:
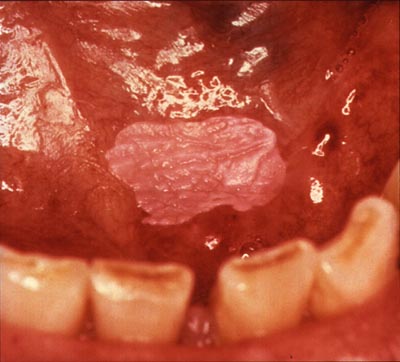
Homogeneous leukoplakia on the floor of the mouth in a smoker
Image: “Homogenous leukoplakia” by National Institutes of Health. License: Public Domain
Homogeneous oral leukoplakia
Image: “Toxic leukoplakia of the oral mucosa in a 62-year-old man” by Klaus D. Peter. License: CC BY 3.0Nonhomogenous leukoplakia presents a higher risk of malignant transformation Transformation Change brought about to an organism’s genetic composition by unidirectional transfer (transfection; transduction, genetic; conjugation, genetic, etc.) and incorporation of foreign DNA into prokaryotic or eukaryotic cells by recombination of part or all of that DNA into the cell’s genome. Bacteriology and may appear:
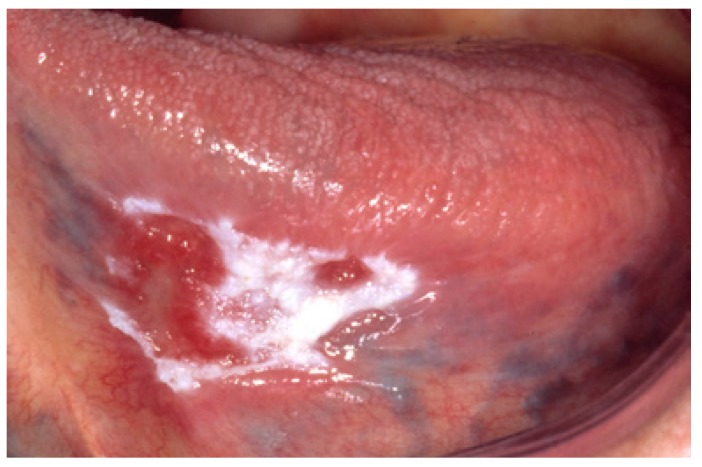
Nonhomogeneous leukoplakia of the tongue with white and red changes
Image: “Nonhomogeneous (white and red changes, also referred to as erythroleukoplakia) in an 88-year-old woman.” by Isaäc van der Waal. License: CC BY 2.5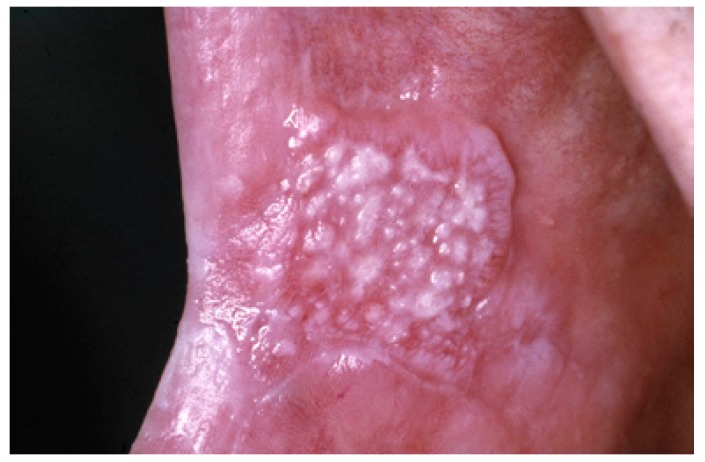
Nonhomogeneous oral leukoplakia with a nodular appearance
Image: “Nonhomogeneous, nodular, leukoplakia in a 61-year-old man” by Isaäc van der Waal. License: CC BY 2.5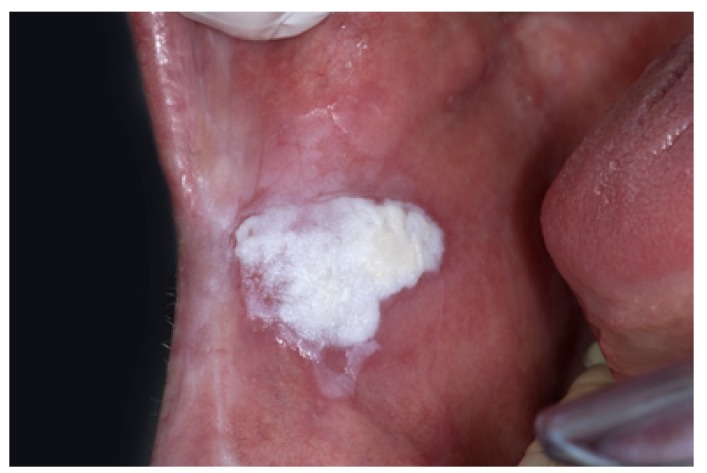
Nonhomogeneous oral leukoplakia with a verrucous texture
Image: “Nonhomogeneous, verrucous leukoplakia” by Isaäc van der Waal. License: CC BY 2.5
Nonhomogeneous exophytic leukoplakia
Image: “exofitic leukoplakia” by Aitor III. License: Public DomainBiopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is required for a definitive diagnosis, to evaluate for dysplasia, and to rule out other conditions. Findings include:
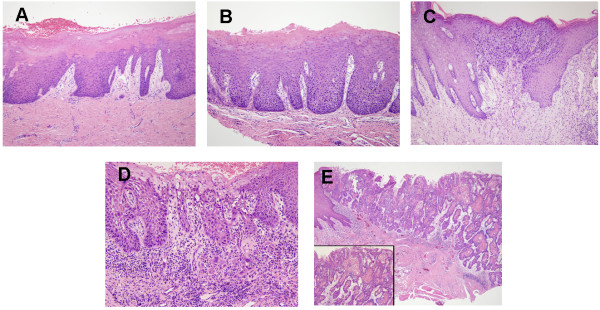
Histological images of oral leukoplakia demonstrating progressive dysplasia and malignant transformation:
A: Hyperkeratosis with low-grade dysplasia present
B: Moderate dysplasia
C: High-grade dysplasia
D: Leukoplakia in the state of becoming invasive carcinoma
E: Invasive carcinoma