Diphtheria is an infectious disease caused by Corynebacterium diphtheriae that most often results in respiratory disease with membranous inflammation of the pharynx, sore throat, fever, swollen glands, and weakness. The hallmark sign is a sheet of thick, gray material covering the back of the throat. Diphtheria can also manifest as cutaneous disease leading to nonspecific skin lesions. In advanced stages, diphtheria can damage the heart, kidneys, and nervous system. It is diagnosed via a culture of pharyngeal swabs and treated with antibiotic therapy and the diphtheria antitoxin.
Last updated: Apr 26, 2025
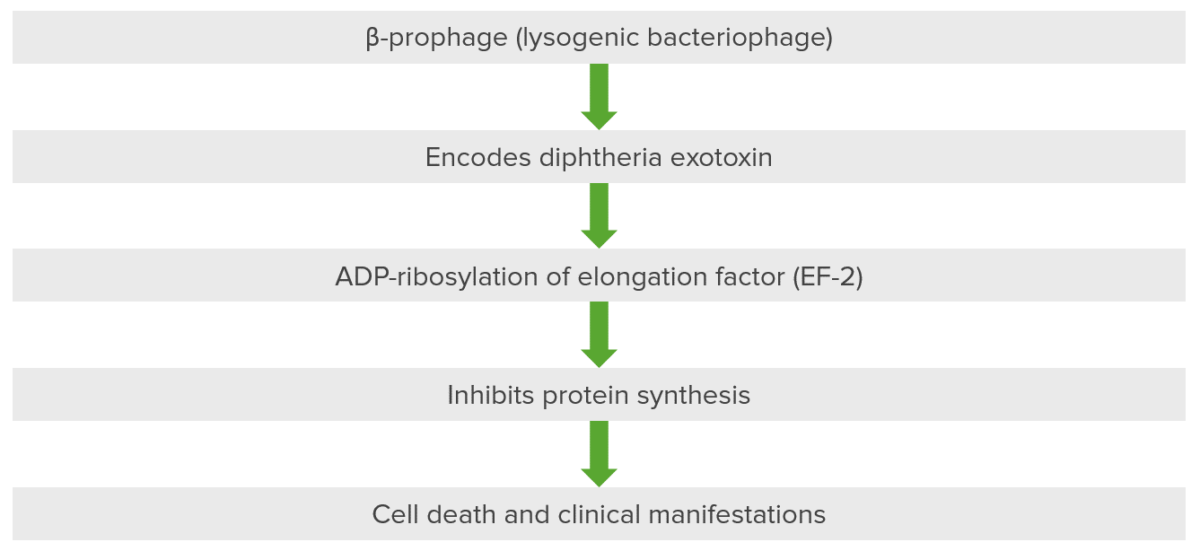
Pathogenesis of diseases associated with Corynebacterium: diphtheria exotoxin inactivates elongation factor (EF-2) via ADP-ribosylation.
This bacteriophage, a beta prophage, introduces itself into the cell and DNA of the host organism, resulting in the encoding of diphtheria exotoxin. The exotoxin has 3 domains: 1 is present in fragment A and is catalytic, while 2 are present in fragment B for receptor binding and membrane insertion and translocation. The exotoxin is the major cause of the disease in diphtheria because it ribosylates ADP present in the elongation factor. The elongation factor, specifically elongation factor 2 (EF-2), is critical for the elongation of protein chains. Diphtheria exotoxin inhibits EF-2 so that protein is not synthesized, resulting in cellular death and secondary clinical manifestations.

Clinical sign of a patient with cutaneous (wound) diphtheria: chronic non-healing ulcer
Image: “A diphtheria skin lesion on the leg” by CDC/Public Health Image Library (PHIL). License: Public Domain
A clinical sign of a patient with respiratory diphtheria: severe lymphadenopathy with “bull neck” appearance
Image: “Diphtheria bull neck” by CDC/Public Health Image Library (PHIL). License: Public Domain
Pediatric patient with diphtheria presenting with characteristic grayish-white membrane covering the posterior pharyngeal wall
Image: “A doctor with the UK’s Emergency Medical Team checks a child for symptoms of Diphtheria in a makeshift clinic in the Kutupalong camp for Rohingya refugees in Bangladesh” by Russell Watkins/Department for International Development. License: CC BY 2.0Key points to remember about diphtheria:
ABCDEFG: ADP-ribosylation, Beta-prophage, Corynebacterium diphtheriae, Elongation factor 2, Granules
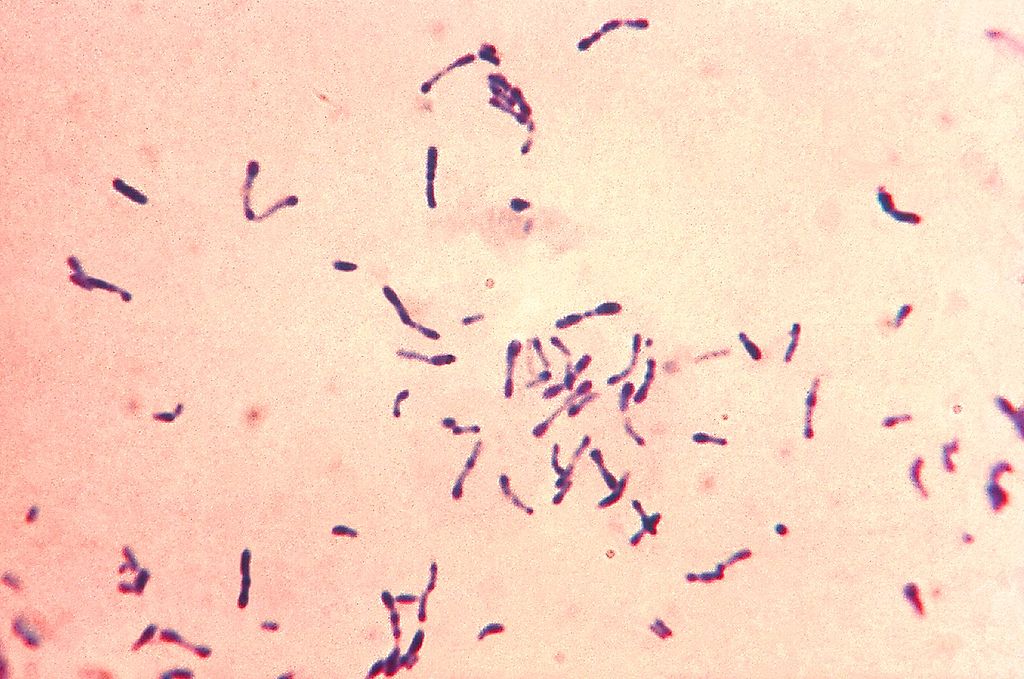
Gram-positive Corynebacterium diphtheriae bacteria with blue metachromatic granules. The bacteria were grown via Loeffler’s medium to enhance the characteristic metachromatic granules. Notice the club-shaped nature and formation into Y and V.
Image: “Gram-positive Corynebacterium diphtheriae bacteria” by Centers for Disease Control and Prevention’s Public Health Image Library (PHIL). License: Public Domain
A throat swab inoculated with Corynebacterium diphtheriae is cultured on a Petri dish plate containing Tinsdale medium supplemented with the agar component Tellurite. The gray-black colonies, each surrounded by a dark brown halo, are characteristic of C. diphtheriae on Tellurite agar.
Image: “Corynebacterium diphtheriae” by Public Health Image Library (PHIL). License: Public DomainPossible complications associated with diphtheria include:
The differential diagnosis of respiratory diphtheria includes: