Malignant lesions of the penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy arise from the squamous epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology of the glans, prepuce Prepuce The double-layered skin fold that covers the glans penis, the head of the penis. Penis: Anatomy, or penile shaft Penile Shaft Bowen Disease and Erythroplasia of Queyrat. Penile cancer is rare in the United States, but there is a higher prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in lower socioeconomic regions. The most common histologic subtype is squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC). Uncircumcised men and those with HPV HPV Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are at highest risk of penile neoplasms Neoplasms New abnormal growth of tissue. Malignant neoplasms show a greater degree of anaplasia and have the properties of invasion and metastasis, compared to benign neoplasms. Benign Bone Tumors. Diagnosis is a combination of physical exam, history, imaging studies, and tissue biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Proper TNM staging Staging Methods which attempt to express in replicable terms the extent of the neoplasm in the patient. Grading, Staging, and Metastasis is necessary to determine the correct treatment, which ranges from local topical therapy to multimodal surgery/ radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma/ chemotherapy Chemotherapy Osteosarcoma.
Last updated: May 17, 2024
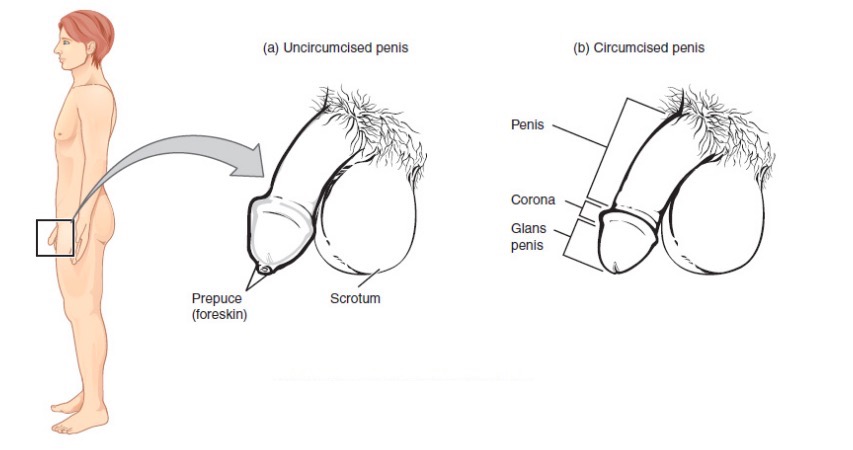
Male reproductive anatomy (external)
Image: “Male Reproductive System” by Phil Schatz. License: CC BY 4.0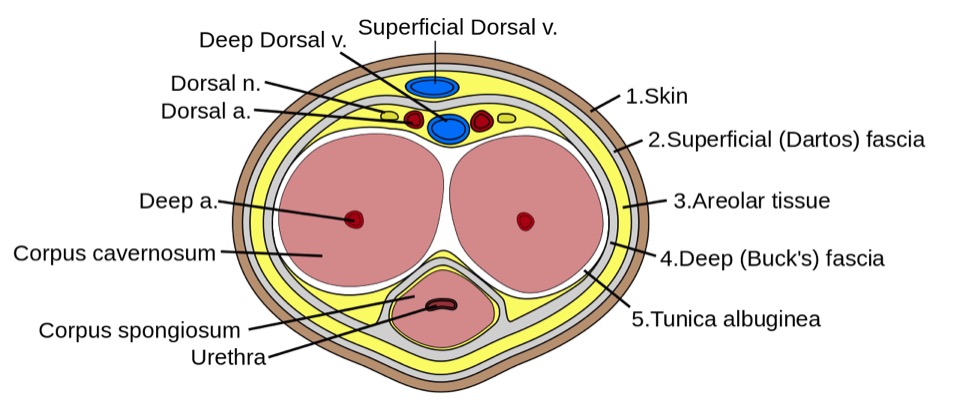
Cross section of the penis:
Image shows the form the erectile tissues take within the body of the penis. Here, note the tunica albuginea enclosing both types of erectile tissue as well as the urethra, which is fully within the corpus spongiosum.

Penile squamous cell carcinoma
Image: “Cancer of the penis” by Service d’Urologie, CHU de Cocody, Abidjan, Ivory Coast, Africa. License: CC BY 4.0| Primary tumor Tumor Inflammation (T) | Description |
|---|---|
| Tx | Primary tumor Tumor Inflammation cannot be assessed. |
| T0 | No evidence of tumor Tumor Inflammation |
| Tis | Carcinoma in situ Carcinoma in situ A lesion with cytological characteristics associated with invasive carcinoma but the tumor cells are confined to the epithelium of origin, without invasion of the basement membrane. Leukoplakia |
| T1 |
|
| T1a | Tumor Tumor Inflammation without lymphovascular invasion or perineural invasion and not high grade |
| T1b | Tumor Tumor Inflammation with lymphovascular invasion and/or perineural invasion or tumor Tumor Inflammation is high grade |
| T2 | Tumor Tumor Inflammation invades corpus spongiosum Corpus spongiosum Penis: Anatomy with or without urethral invasion. |
| T3 T3 A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5′ position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones | Tumor Tumor Inflammation invades corpora cavernosum with or without urethral invasion. |
| T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones | Tumor Tumor Inflammation invades adjacent structures. |
| Regional lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes (N) | Description |
|---|---|
| cNx | Regional lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes cannot be assessed. |
| cN0 | No palpable or visibly enlarged inguinal lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
| cN1 | Palpable mobile unilateral inguinal lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node |
| cN2 | ≥ 2 palpable mobile unilateral inguinal nodes or bilateral inguinal lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
| cN3 | Palpable fixed inguinal nodal mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast or pelvic lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy unilateral or bilateral |
| Distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis (M) | Description |
|---|---|
| M0 | No distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis |
| M1 | Distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis |
| Treatment strategy | Explanation |
|---|---|
| Penis-preserving interventions |
|
| Partial/total amputation Amputation An amputation is the separation of a portion of the limb or the entire limb from the body, along with the bone. Amputations are generally indicated for conditions that compromise the viability of the limb or promote the spread of a local process that could manifest systemically. Amputation | Partial excision decision has to be exercised with great caution in selected patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with locally invasive tumors. |
| Surveillance Surveillance Developmental Milestones and Normal Growth for lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis | Low-risk patient with no vascular invasion |
| Early lymphadenectomy | For high-risk patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship or with vascular invasion |
Carcinoma in situ Carcinoma in situ A lesion with cytological characteristics associated with invasive carcinoma but the tumor cells are confined to the epithelium of origin, without invasion of the basement membrane. Leukoplakia or Tis–T1:
Bulky T2– T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones tumors:
Lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes: