Basal cell Basal Cell Erythema Multiforme carcinoma is the most common skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions malignancy Malignancy Hemothorax. This cancer arises from the basal layer of the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions. The lesions most commonly appear on the face as pearly nodules, often with telangiectatic blood vessels and ulceration Ulceration Corneal Abrasions, Erosion, and Ulcers in elderly individuals. Diagnosis is established by tissue biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Despite having low metastatic potential, basal cell Basal Cell Erythema Multiforme carcinoma should be treated adequately because it is locally aggressive and destructive to tissues. Complete surgical excision is the main treatment method. Long-term prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is excellent with adequate management.
Last updated: May 17, 2024
Basal cell Basal Cell Erythema Multiforme carcinoma is a skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions cancer arising from the basal layer of epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions and its appendages.
| Type | Frequency | Histology | Clinical presentation |
|---|---|---|---|
| Nodular basal cell Basal Cell Erythema Multiforme carcinoma | 80% |
|
|
| Superficial basal cell Basal Cell Erythema Multiforme carcinoma | 15% | Atypical basaloid tumors arise as buds from the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions |
|
| Morpheaform basal cell Basal Cell Erythema Multiforme carcinoma | 5%–10% |
|
|

Nodular basal cell carcinoma of the nose:
Pearly nodule with visible telangiectatic vessels

Superficial basal cell carcinoma:
A pink, scaly lesion on the skin

Morpheaform basal cell carcinoma:
Sclerotic, partially reddish plaque with irregular borders and crusting in the center
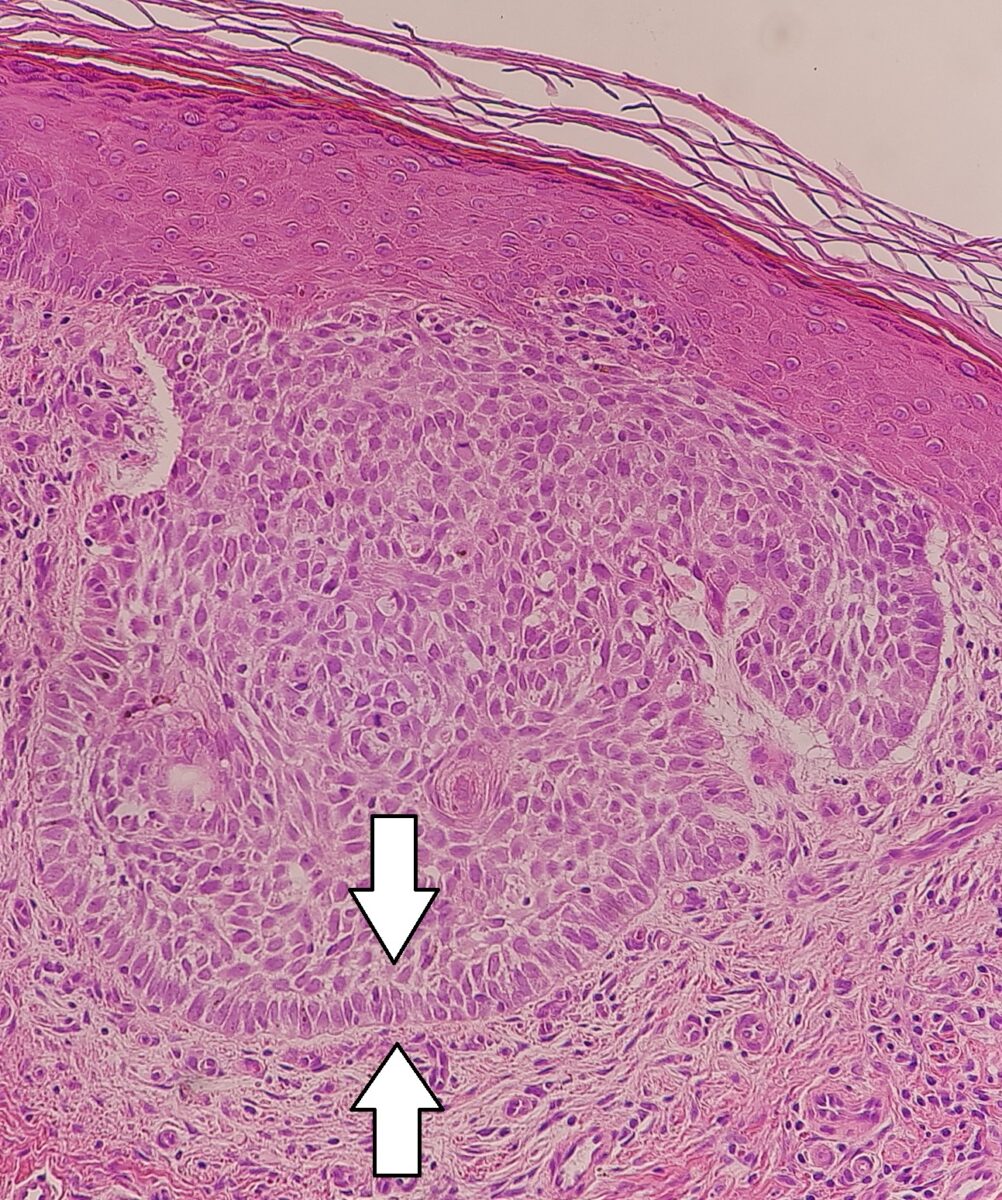
Nodular basal cell carcinoma:
Palisading keratinocytes in nodular basal cell cancer
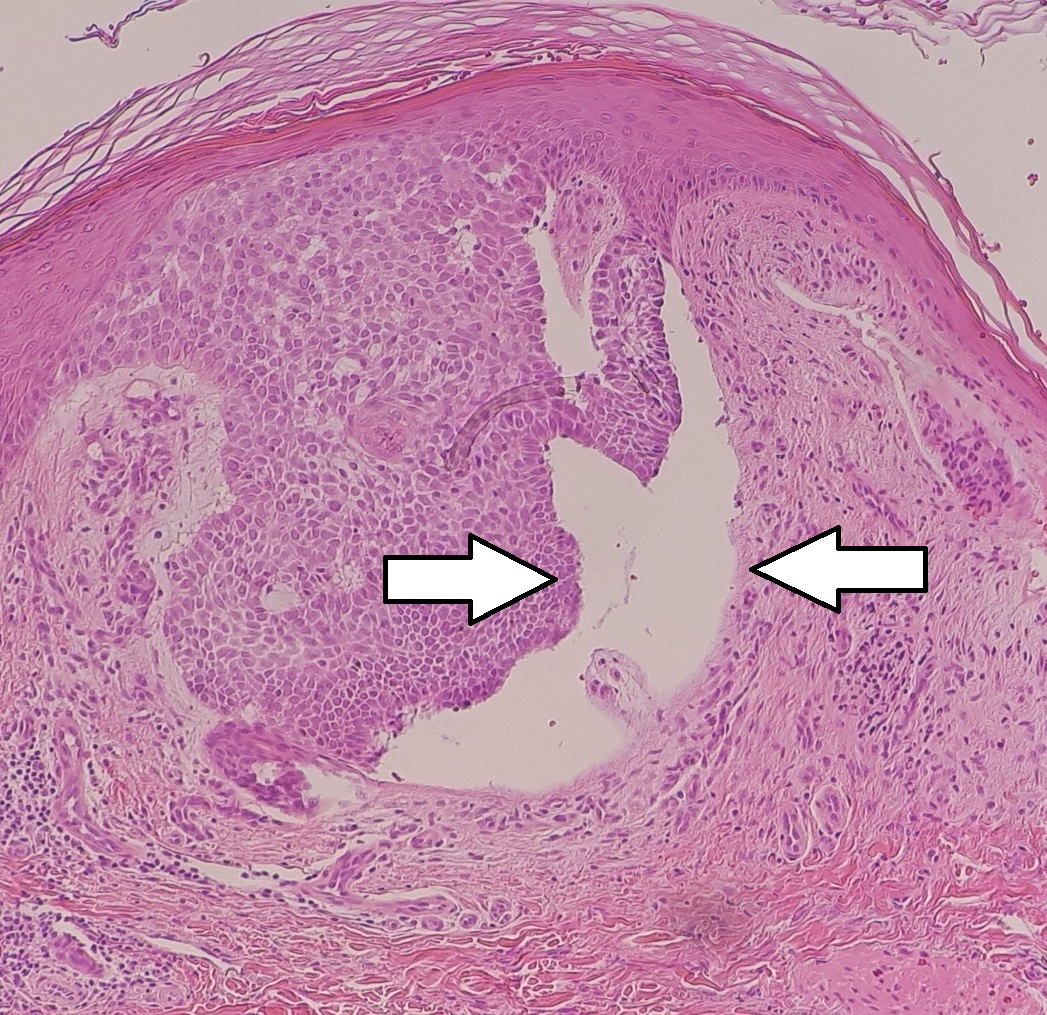
Nodular basal cell carcinoma:
Micrograph of a nodular basal cell cancer with a cleft
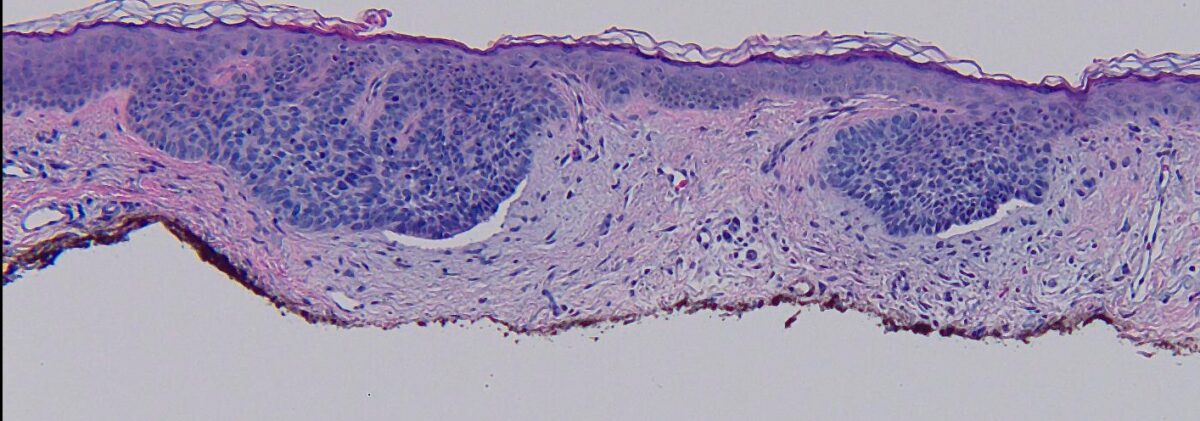
Micrograph of superficial basal cell carcinoma:
Palisading tumor cells budding off of the epidermis
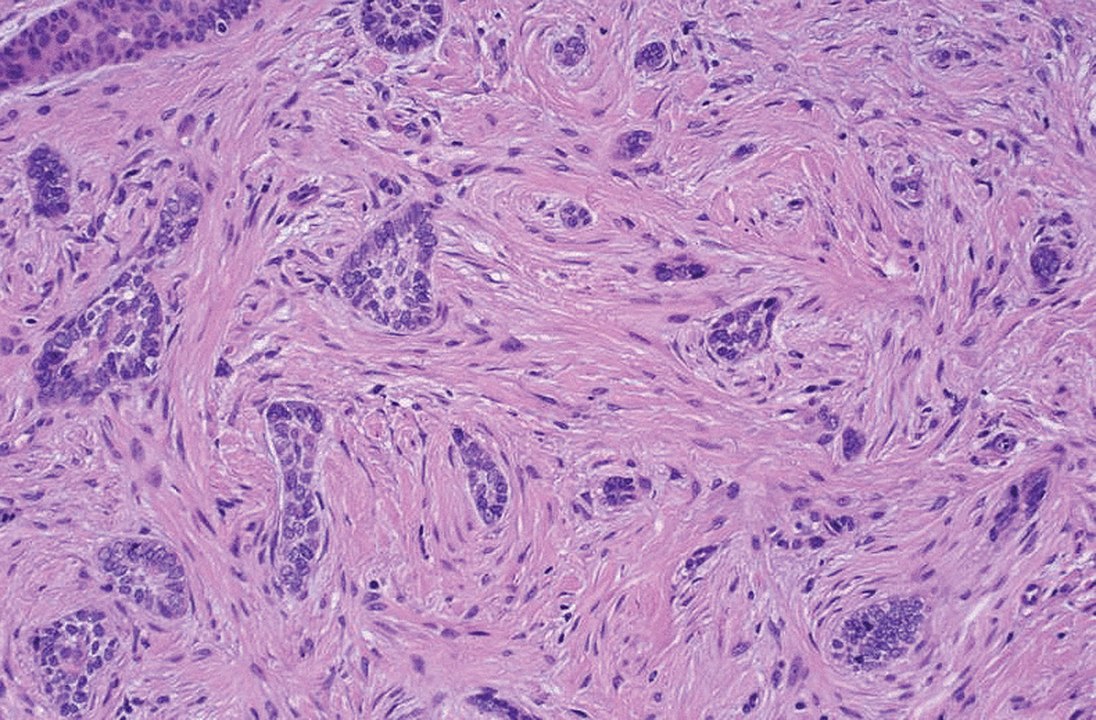
Morpheaform basal-cell carcinoma: Cords of tumor cells grow into the dermis (infiltrative)
Image: “Morpheaform basal-cell carcinoma” by Masahiro Nakayama, Keiji Tabuchi, Yasuhiro Nakamura, and Akira Hara. License: CC BY 4.0History:
Physical exam:
Dermoscopy Dermoscopy A noninvasive technique that enables direct microscopic examination of the surface and architecture of the skin. Seborrheic Keratosis:
Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma:
Assess risk of recurrence:
Surgery:
Alternative therapies:
Therapy for advanced disease: