Anal cancer accounts for 2.7% of all gastrointestinal tract cancers. Squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC) is the most common type of anal cancer. The patient can present with rectal bleeding (most common), change in bowel habits, perianal pruritic mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast, or perianal painful ulceration Ulceration Corneal Abrasions, Erosion, and Ulcers. The diagnosis is established via biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Staging Staging Methods which attempt to express in replicable terms the extent of the neoplasm in the patient. Grading, Staging, and Metastasis is done through imaging studies. Depending on the stage, treatment options include chemoradiotherapy and/or surgery. If treated early, anal cancer has a favorable prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas.
Last updated: Apr 11, 2023
Anal cancers are cancers arising in the anal canal or anal margin.
Anatomy:
Histology:
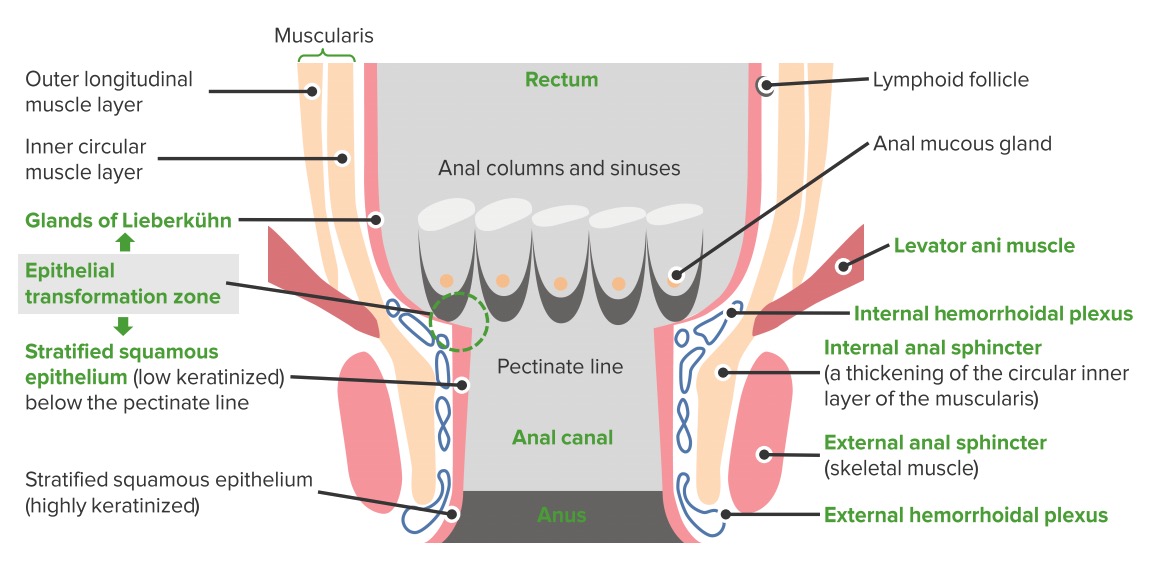
Anatomy of the anal canal
Image by Lecturio.Risk factors for anal cancer:
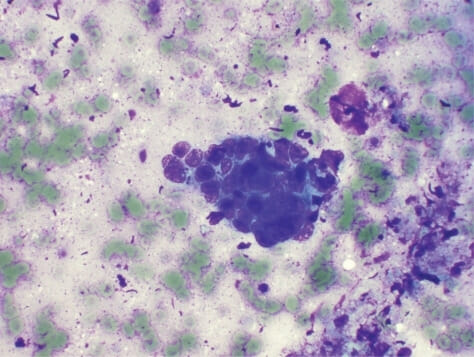
Squamous cell carcinoma of the anal canal:
Endoscopic US-guided fine-needle aspiration reveals poorly differentiated squamous cell carcinoma of the anal canal. Peripheral nuclear palisading cells are seen. (H&E staining, 40x)

Carcinoma of the anal canal
Image: “Anal canal carcinoma” by Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main. License: CC BY 3.0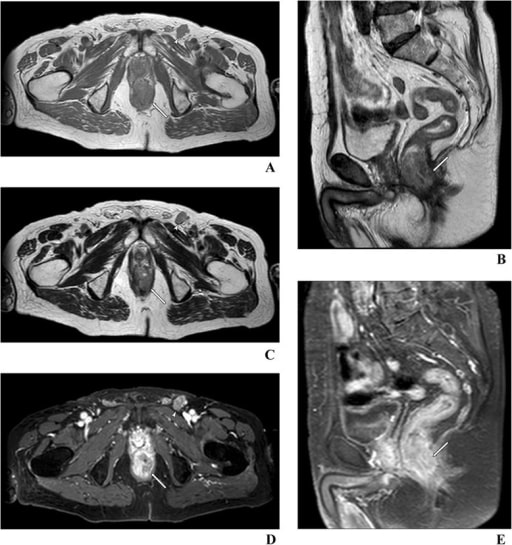
Magnetic resonance imaging images of anal cancer with invasion of the intersphincteric space and external anal sphincter (arrow)
Image: “Anal cancer with invasion of the intersphincteric space” by St. John’s Cancer Centre, 7 Jaczewskiego Str., 20-090, Lublin, Poland. License: CC BY 4.0
Computed tomography images of SCC of the anal canal extending from the anorectal junction to below the anal verge
Image: “Ulcero-fungating anal mass” by Massimo Tonolinicorresponding author and Roberto Bianco. License: CC BY 4.0| Primary tumor Tumor Inflammation (T) | Regional lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy (N) | Distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis (M) |
|---|---|---|
| Tx: primary tumor Tumor Inflammation not assessed | Nx: regional lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy cannot be assessed | M0: no distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis |
| T0: no evidence of primary tumor Tumor Inflammation | N0: no regional lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis | M1: distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis |
| Tis: high-grade squamous intraepithelial lesion | N1:
metastasis
Metastasis
The transfer of a neoplasm from one organ or part of the body to another remote from the primary site.
Grading, Staging, and Metastasis in inguinal, mesorectal, internal iliac, or external iliac nodes
|
|
| T1: tumor Tumor Inflammation ≤ 2 cm | ||
| T2: tumor Tumor Inflammation > 2 cm but ≤ 5 cm | ||
| T3 T3 A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5′ position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones: tumor Tumor Inflammation > 5 cm | ||
| T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones: tumor Tumor Inflammation of any size invading adjacent organs, such as the vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy, urethra Urethra A tube that transports urine from the urinary bladder to the outside of the body in both the sexes. It also has a reproductive function in the male by providing a passage for sperm. Urinary Tract: Anatomy, or bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess |
| Stage | T | N | M |
|---|---|---|---|
| 0 | Tis | N0 | M0 |
| I | T1 | N0 | M0 |
| IIA | T2 | N0 | M0 |
| IIB | T3 T3 A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5′ position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones | N0 | M0 |
| IIIA | T1–2 | N1 | M0 |
| IIIB | T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones | N0 | M0 |
| IIIC | T3 T3 A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5′ position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones–4 | N1 | M0 |
| IV | Any T | Any N | M1 |