The purine salvage pathway involves production of purine nucleotides Nucleotides The monomeric units from which DNA or RNA polymers are constructed. They consist of a purine or pyrimidine base, a pentose sugar, and a phosphate group. Nucleic Acids from nucleoside intermediates formed during degradation of RNA RNA A polynucleotide consisting essentially of chains with a repeating backbone of phosphate and ribose units to which nitrogenous bases are attached. RNA is unique among biological macromolecules in that it can encode genetic information, serve as an abundant structural component of cells, and also possesses catalytic activity. RNA Types and Structure and DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure. The salvaged nucleosides Nucleosides Purine or pyrimidine bases attached to a ribose or deoxyribose. Nucleic Acids can be reconverted back into nucleotides Nucleotides The monomeric units from which DNA or RNA polymers are constructed. They consist of a purine or pyrimidine base, a pentose sugar, and a phosphate group. Nucleic Acids. These salvage pathways are crucial in tissues incapable of de novo synthesis Synthesis Polymerase Chain Reaction (PCR) of purine nucleotides Nucleotides The monomeric units from which DNA or RNA polymers are constructed. They consist of a purine or pyrimidine base, a pentose sugar, and a phosphate group. Nucleic Acids. Deficiencies in these pathways can give rise to conditions such as Lesch-Nyhan syndrome and adenine phosphoribosyltransferase Adenine phosphoribosyltransferase An enzyme catalyzing the formation of amp from adenine and phosphoribosylpyrophosphate. It can act as a salvage enzyme for recycling of adenine into nucleic acids. Purine and Pyrimidine Metabolism (APRT) deficiency. Lesch-Nyhan syndrome presents with neurologic deficits Neurologic Deficits High-Risk Headaches and self-mutilation in the 1st year of life and APRT deficiency presents with renal dysfunction. There is no cure for either disease, and treatment is supportive. The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is poor for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with Lesch-Nyhan syndrome, as affected individuals die within the 1st 2 decades of life. Indivuals affected with APRT deficiency have a better prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas, but develop end-stage renal disease if not treated.
Last updated: Apr 23, 2025
Purines Purines A series of heterocyclic compounds that are variously substituted in nature and are known also as purine bases. They include adenine and guanine, constituents of nucleic acids, as well as many alkaloids such as caffeine and theophylline. Uric acid is the metabolic end product of purine metabolism. Nucleic Acids are used for cellular energy and may be recycled through a salvage pathway that is susceptible to enzyme deficiencies that cause Lesch-Nyhan syndrome and adenine phosphoribosyltransferase Adenine phosphoribosyltransferase An enzyme catalyzing the formation of amp from adenine and phosphoribosylpyrophosphate. It can act as a salvage enzyme for recycling of adenine into nucleic acids. Purine and Pyrimidine Metabolism (APRT) deficiency.
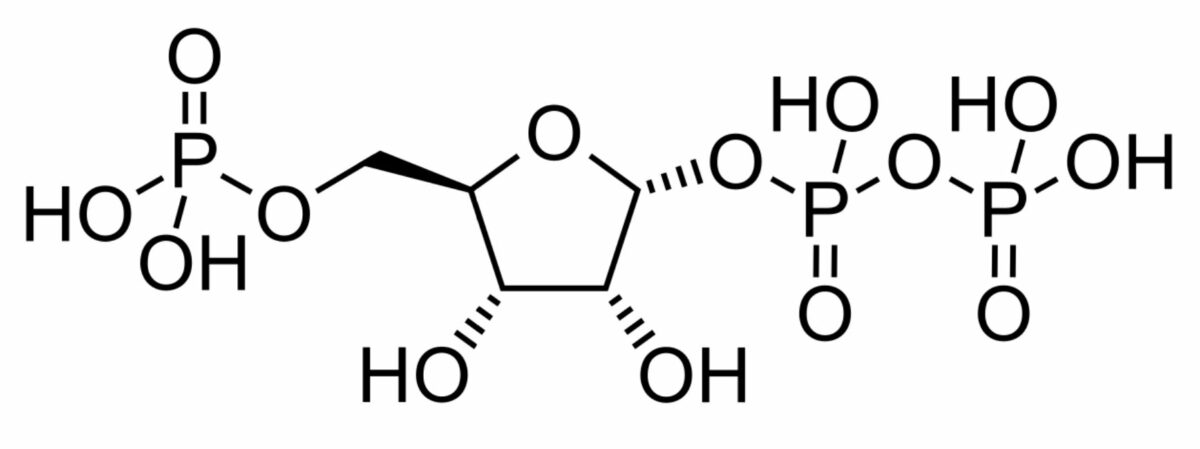
Chemical structure of phosphoribosyl pyrophosphate:
This pentose phosphate plays an important role in transferring phosphoribose groups to accommodate different reactions. Increased levels of this chemical are seen with Lesch-Nyhan syndrome.
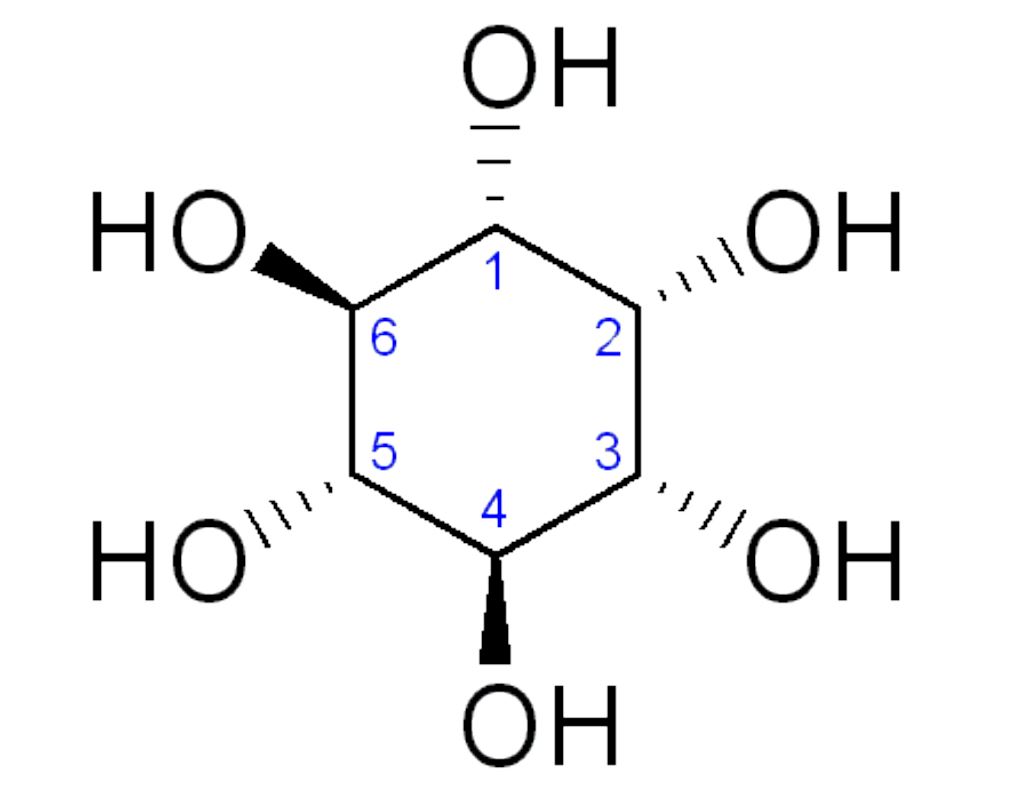
General structure of inositol:
Less inositol monophosphate is produced in Lesch-Nyhan syndrome as more uric acid is produced, resulting in hyperuricemia.

Wounded thumb due to the self-mutilation behavior in Lesch-Nyhan syndrome
Image: “Lesch-Nyhan Syndrome: Disorder of Self-mutilating Behavior” by Jathar P, Panse AM, Jathar M, Gawali PN . License: CC BY 3.0