Cerebral palsy Palsy paralysis of an area of the body, thus incapable of voluntary movement Cranial Nerve Palsies (CP) refers to a group of conditions resulting in motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology impairment affecting tone and posture and limiting physical activity. Cerebral palsy Palsy paralysis of an area of the body, thus incapable of voluntary movement Cranial Nerve Palsies is the most common cause of childhood disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman's compensation benefits. ABCDE Assessment. It is caused by a nonprogressive CNS injury to the fetal or infant brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification. It is classified according to muscle tone Muscle tone The state of activity or tension of a muscle beyond that related to its physical properties, that is, its active resistance to stretch. In skeletal muscle, tonus is dependent upon efferent innervation. Skeletal Muscle Contraction, its distribution, and the presumed time of injury (spastic diplegia is the most common), and it is present in around 3 per 1,000 live births. Diagnosis is made by a detailed history and physical exam with an MRI scan confirming CNS insult. Interventions are multidisciplinary and prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas depends on the degree of disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman's compensation benefits. ABCDE Assessment.
Last updated: Feb 18, 2025
Cerebral palsy Palsy paralysis of an area of the body, thus incapable of voluntary movement Cranial Nerve Palsies (CP) is a syndrome of permanent motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology impairment (posture and movement) that results from nonprogressive lesions to the developing brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification.
The ultimate cause of CP is injury to a child’s CNS during its embryological or perinatal development. The pathophysiology of this insult varies based on its etiology.
| CP subtype | Etiologies | MRI findings |
|---|---|---|
| Hemiplegia (25%) |
|
|
| Spastic quadriplegia Quadriplegia Severe or complete loss of motor function in all four limbs which may result from brain diseases; spinal cord diseases; peripheral nervous system diseases; neuromuscular diseases; or rarely muscular diseases. The locked-in syndrome is characterized by quadriplegia in combination with cranial muscle paralysis. Consciousness is spared and the only retained voluntary motor activity may be limited eye movements. This condition is usually caused by a lesion in the upper brain stem which injures the descending corticospinal and corticobulbar tracts. Locked-in Syndrome (20%) |
|
|
| Spastic diplegia (35%) |
|
|
| Extrapyramidal (athetoid, dyskinetic) (15%) |
|
|
Neurological:
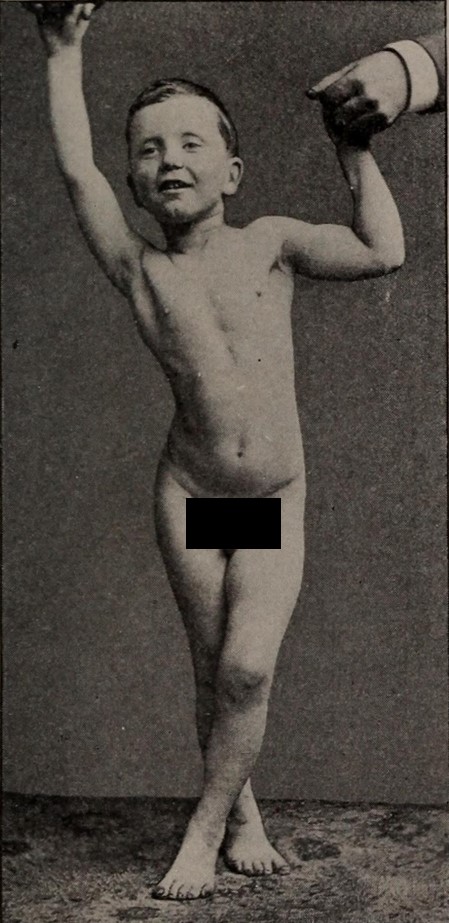
Photograph of a child with spastic diplegia:
Notice the scissoring of the legs, a key finding in the spastic diplegic form of cerebral palsy (CP).
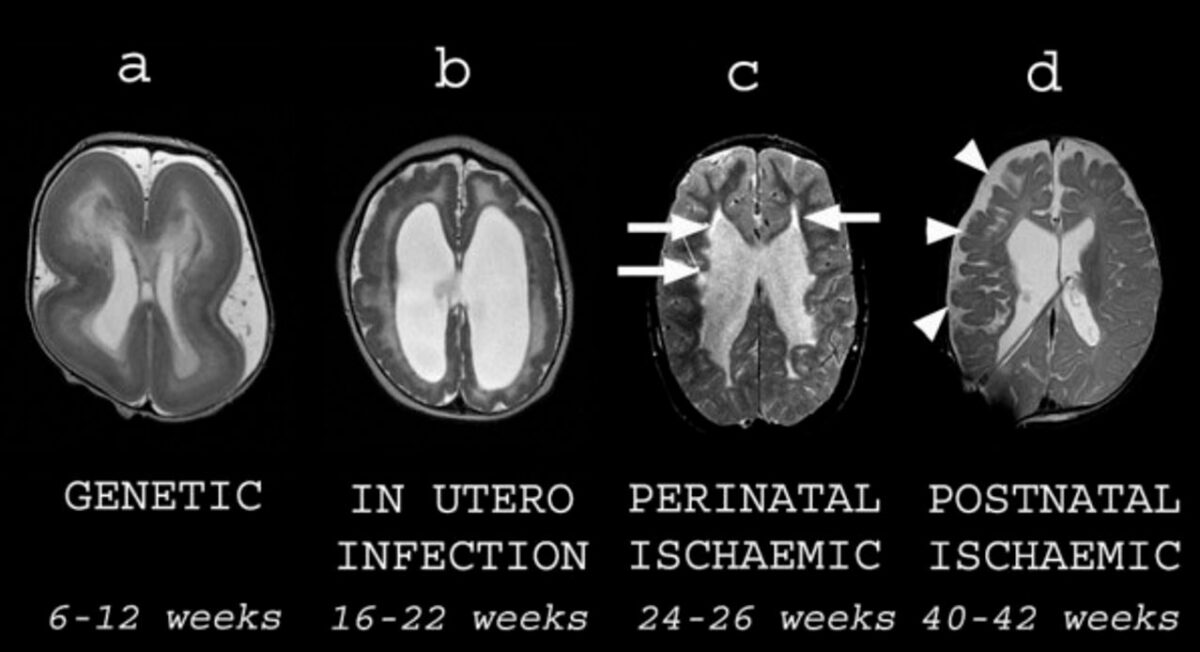
Different types of structural brain abnormalities in cerebral palsy (CP):
All images are axial T2-weighted MRI scans. Each image is subtitled by its presumed etiology and timing during gestation.
A: a child with lissencephaly showing cortical thickening and agyria
B: a child with congenital cytomegalovirus infection showing an overfolded cortex (polymicrogyria), thin white matter, and dilated lateral ventricles
C: an ex-premature child showing cystic white matter injury (arrows) consistent with periventricular leukomalacia
D: a child who suffered a hemorrhagic stroke in the newborn period. There is cortical and white matter loss in the right frontal and parietal lobes (arrowheads) consistent with previous ischemia.
There is no curative treatment at this time. Management focuses on improving symptoms and increasing function while addressing comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus. Early multidisciplinary intervention improves patient outcomes.
The following conditions are etiological and/or risk factors for CP: