A esofagite é a inflamação ou irritação do esófago. Os principais tipos de esofagite são a induzida por fármacos, a infeciosa, a eosinofílica, a corrosiva e a de refluxo ácido. Os doentes apresentam-se tipicamente com odinofagia, disfagia e dor torácica retroesternal. O diagnóstico é feito por endoscopia com biópsia. São realizados exames laboratoriais e de imagem dependendo do grau de lesão e envolvimento de outros sistemas de órgãos. O tratamento da esofagite depende da etiologia subjacente e inclui alterações dietéticas, evicção de agentes agressores, antibioterapia ou utilização de um inibidor da bomba de protões. Nos casos graves, como nas lesões corrosivas, pode ser necessário realizar uma cirurgia. Se não for tratada, a esofagite pode levar a complicações como estenoses, metaplasia do esófago e desenvolvimento de neoplasia maligna.
Última atualização: Jan 16, 2024
Para lembrar as causas mais comuns de esofagite: “PIECE”
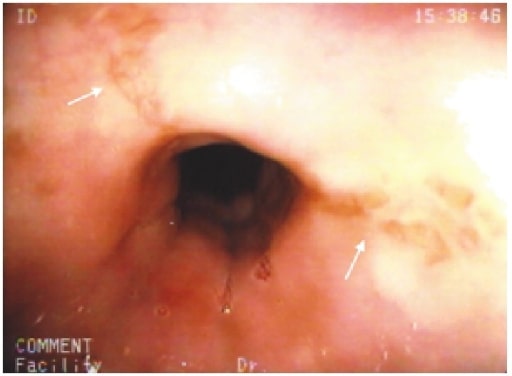
Erosões em estrela no esófago médio (setas brancas) num doente com esofagite induzida por cloxacilina
Imagem: “Cloxacillin: A New Cause of Pill-Induced Esophagitis” de Zezos P, Harel Z, Saibil F. Licença: CC BY 4.0O diagnóstico é feito por endoscopia digestiva alta.
Achados na endoscopia digestiva alta de um doente com esofagite por citomegalovírus. É possível ver uma úlcera com uma base branca no esófago.
Imagem: “Cytomegalovirus esophagitis developing during chemoradiotherapy for esophageal cancer” do Journal of Medical Case Reports. Licença: CC BY 4.0O diagnóstico é feito por endoscopia digestiva alta.
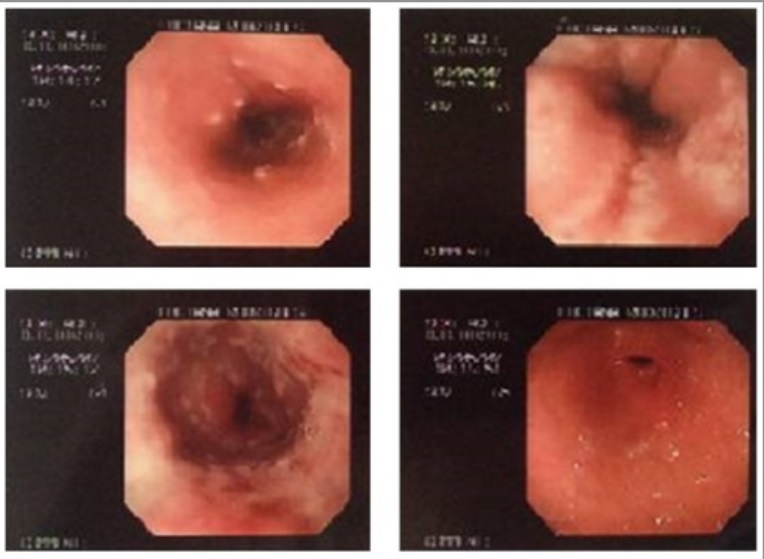
Endoscopia digestiva alta de um doente, que mostra numerosas lesões na superfície esofágica, de coloração amarelo-esbranquiçada, pleomórficas e pequenas placas circulares isoladas com erosões centrais.
Imagem: “Herpetic esophagitis in immunocompetent medical student” de Marinho AV, Bonfim VM, de Alencar LR, Pinto SA, de Araújo Filho JA. Licença: CC BY 3.0O diagnóstico é feito por endoscopia digestiva alta.

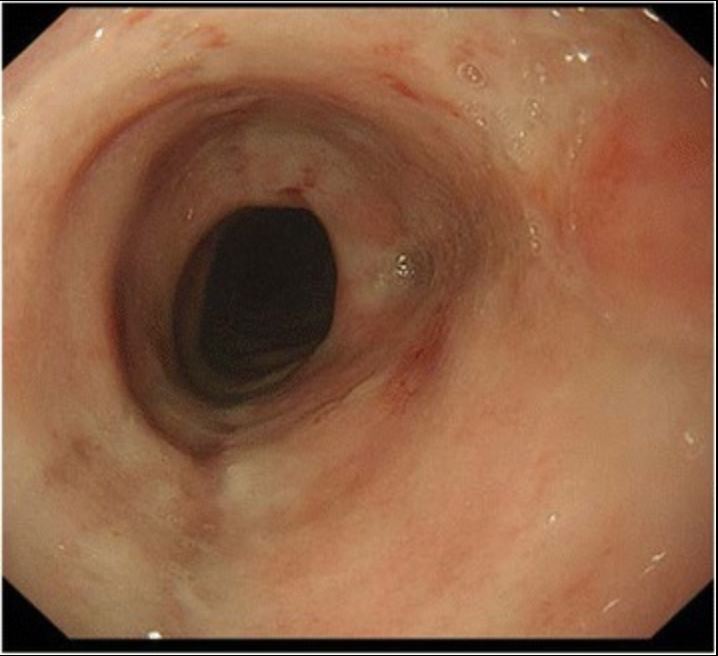
A endoscopia digestiva alta mostra lesões brancas difusas no esófago, características de esofagite por Candida .
Imagem: “Epigastric Distress Caused by Esophageal Candidiasis” de Chen KH, Weng MT, Chou YH, Lu YF, Hsieh CH. Licença: CC BY 4.0O diagnóstico é feito por endoscopia digestiva alta.
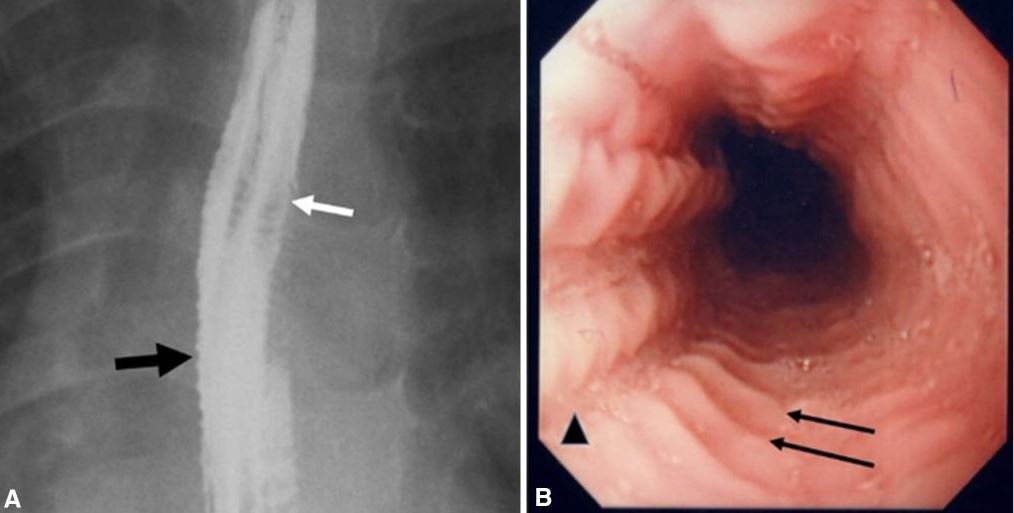
Images of eosinophilic esophagitis:
A. Esophagram in a patient with history of recurrent food impactions and dysphagia shows multiple esophageal rings (white arrow), giving the appearance of a corrugated or ringed esophagus, and mucosal irregularity (black arrow).
B. Endoscopy shows multiple transverse rings (arrows) and mucosal furrowing (arrowhead).
Achados na endoscopia digestiva alta de uma criança que ingeriu uma substância alcalina: estenose pilórica desenvolvida 2 meses após a lesão.
Imagem: “Pyloric stenosis after 2 months” de Dehghani SM, Aldaghi M, Javaherizadeh H. Licença: CC BY 3.0A esofagite de refluxo é também conhecida como doença de refluxo gastroesofágico (DRGE).
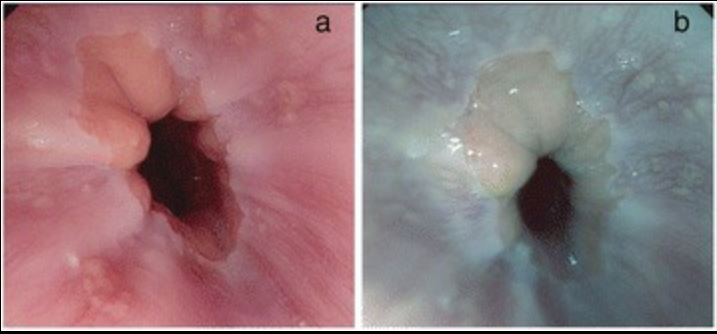
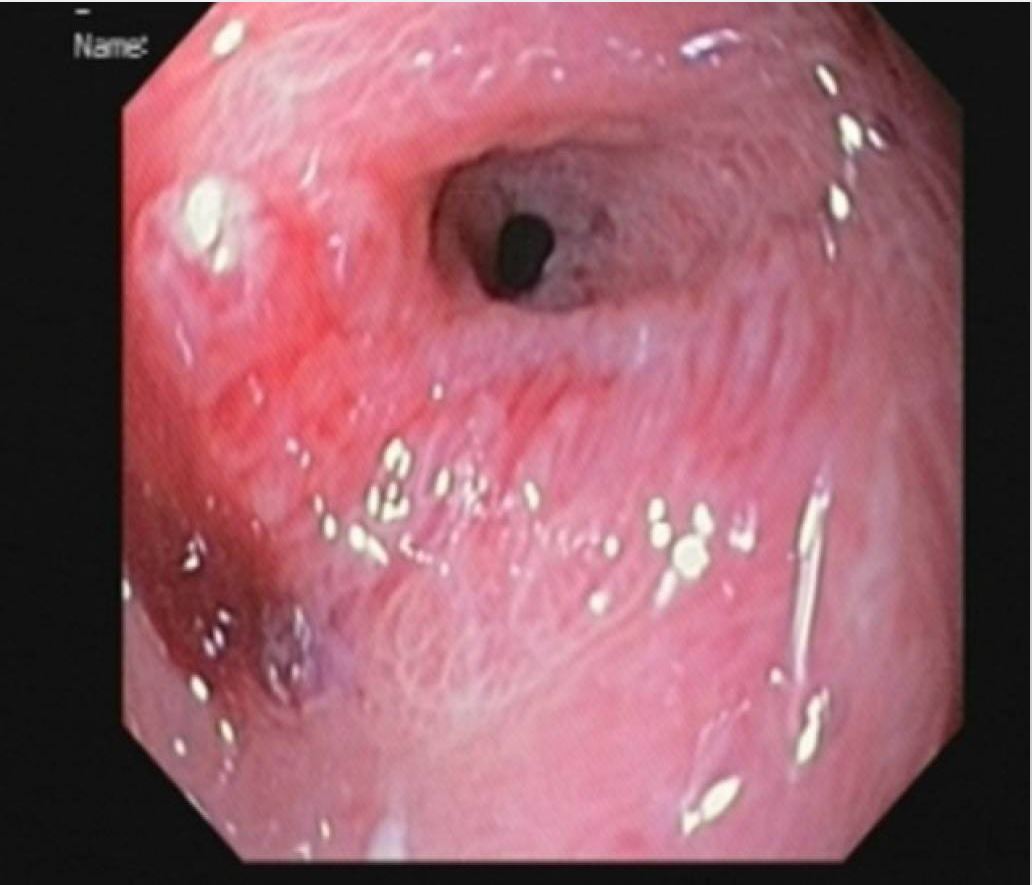
Esofagite de refluxo na endoscopia digestiva alta:
A: imagem de alta definição das alterações esofágicas na DRGE
B: imagem de DRGE com melhoria da tonalidade