Meningiomas are slow-growing tumors that arise from the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy. The vast majority are benign Benign Fibroadenoma. These tumors commonly occur in individuals with a history of high doses of skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma, head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma, and neurofibromatosis type 2 Neurofibromatosis type 2 Neurofibromatosis type 2 is a neurocutaneous disorder that can arise from mutations in the NF2 gene located in chromosome 22 and may be inherited in an autosomal dominant fashion or occur from de novo mutations. The main clinical features are bilateral vestibular schwannomas, intracranial/spinal meningioma, and intramedullary and extramedullary spinal tumors. Neurofibromatosis Type 2. Clinical symptoms of meningioma depend on the location and progression of the tumor Tumor Inflammation, with a large proportion of meningiomas being asymptomatic. When symptoms do develop, they most commonly include headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, visual disturbances, and other focal neurologic deficits Neurologic Deficits High-Risk Headaches. Diagnosis is made based on neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant (MRI is the gold standard) and biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Management involves surveillance Surveillance Developmental Milestones and Normal Growth for asymptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship and, for symptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, surgical resection. Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma is also used in some cases.
Last updated: Mar 25, 2025
A meningioma is a slow-growing tumor Tumor Inflammation that arises from the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy.
| Categories | Specific tumors |
|---|---|
| Neuroepithelial tumors in the CNS |
|
| Meningeal tumors |
|
| Sellar region tumors |
|
| Other primary CNS tumors | Primary CNS lymphoma Lymphoma A general term for various neoplastic diseases of the lymphoid tissue. Imaging of the Mediastinum |
| Metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis to the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification (5x more common than primary brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification tumors) | Most commonly arising from: |
| Peripheral tumors |
|
Meningiomas are classified morphologically by WHO into 3 grades:
The causes of meningioma have not been established. However, certain factors at high risk of causing meningiomas have been identified:
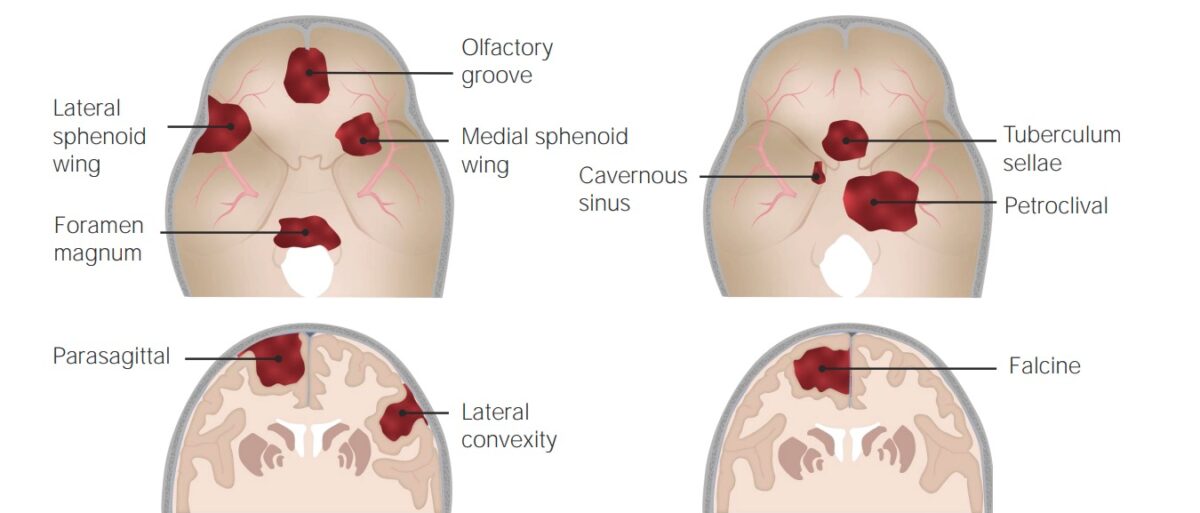
Common sites of occurrence of meningiomas
Image by Lecturio. License: CC BY-NC-SA 4.0Meningiomas commonly arise from the arachnoid cells near the vicinity of the venous sinuses Venous sinuses Veins: Histology. As the tumor Tumor Inflammation enlarges, it can cause symptoms due to:
Some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic. For symptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, the clinical presentation of meningiomas depends on the location of the tumor Tumor Inflammation.
Laboratory studies are of little use in the diagnosis of meningiomas; imaging is a more helpful diagnostic tool. Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is required to confirm the diagnosis.
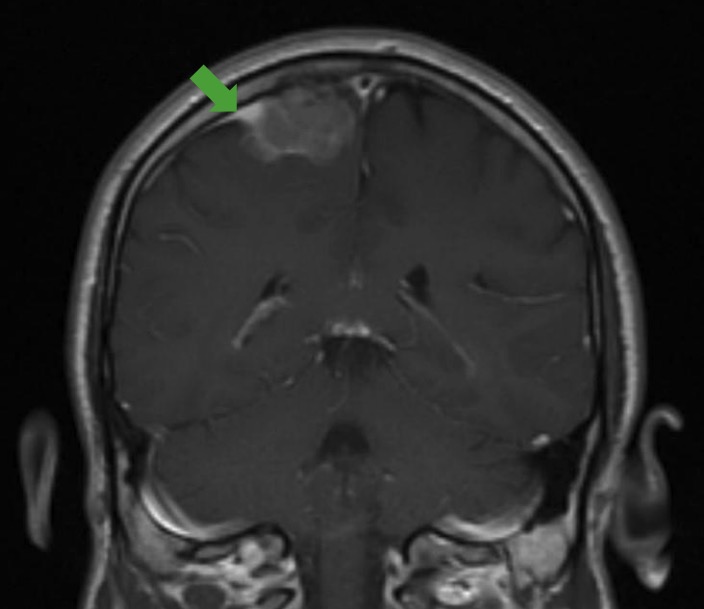
Dural tail sign:
MRI showing the classic dural tail sign (green arrow), which can be seen in imaging of a meningioma.
Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma provides a definitive diagnosis. Histologic findings include:
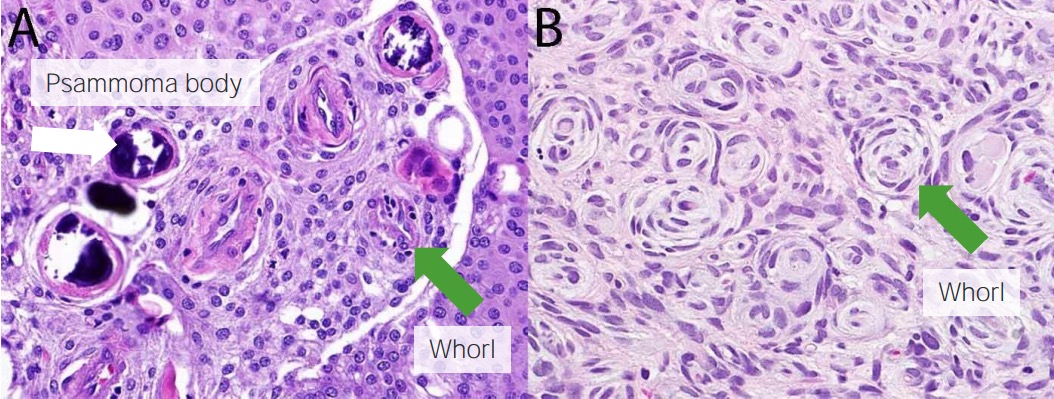
Meningioma histology:
Psammoma bodies (white arrow) and whorls (green arrows) are seen.
The majority of meningiomas can be observed, at least initially.
| Grade | Extent of resection | Recurrence risk (10-year interval) |
|---|---|---|
| I | Macroscopically complete removal of tumor Tumor Inflammation, involved bones, venous sinuses Venous sinuses Veins: Histology, and dural tail | 9% |
| II | Macroscopically complete removal of tumor Tumor Inflammation, coagulation of dural tail | 19% |
| III | Macroscopically complete removal of tumor Tumor Inflammation, resection of dural tail | 29% |
| IV | Partial tumor Tumor Inflammation removal, no resection of dural tail | 44% |
| V | Simple decompression, no resection of dural tail | 100% |
| Grade | Type of surgery | Requirement of radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy |
|---|---|---|
| WHO grade I | Gross total resection | Observe |
| Subtotal resection | Observe versus radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy | |
| No surgery | Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy | |
| WHO grade II | Gross total resection | Observe versus radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy |
| Subtotal resection | Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy | |
| WHO grade III | Any surgery | Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy |