A number of changes normally occur in the aging individual. These changes affect neurocognitive function, organ function, senses, metabolism, sexual function, and sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep patterns. Physicians Physicians Individuals licensed to practice medicine. Clinician–Patient Relationship need to understand the difference between normal cognitive decline associated with aging and pathologic decline. History, physical examination, imaging, laboratory studies, and neuropsychological testing may help determine possible causes of pathologic decline. Many conditions that cause pathologic cognitive decline have no cure, but symptoms may be managed with medications and a strong support system.
Last updated: Apr 28, 2025
Normal changes in the elderly should not impair daily functioning, such as self-care, everyday activities, managing finances, and medication management.
Anatomic and physiologic changes:
Effects:
Anatomic and physiologic changes:
Effects:
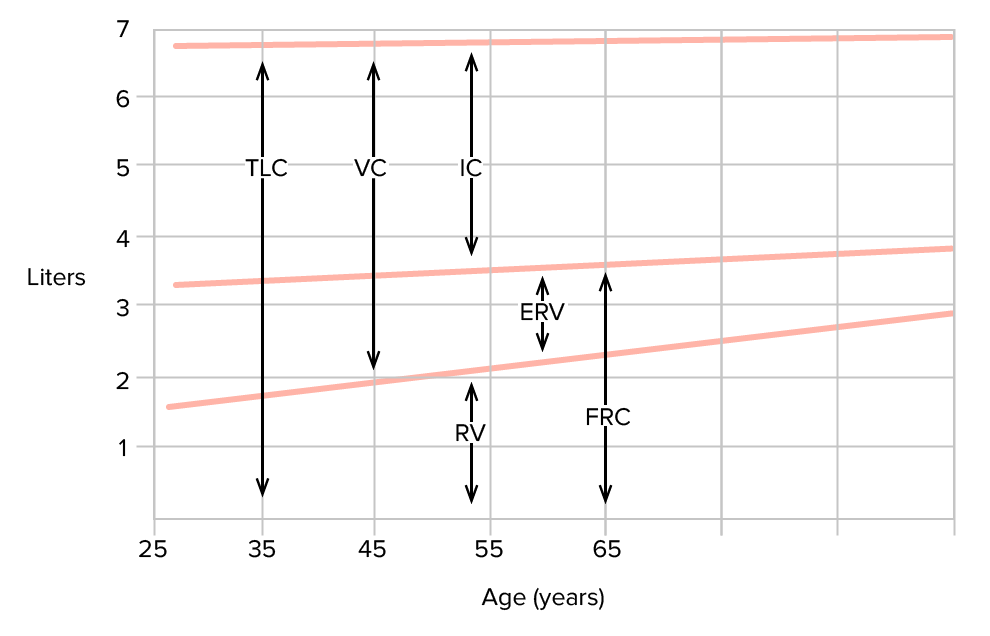
Changes in lung function and lung volumes with age:
Aging creates some predictable changes in lung volumes. Certain compartments are affected more than others, as is illustrated by changes in pulmonary function tests.
ERV: expiratory reserve volume
FRC: functional residual capacity
C: inspiratory capacity
RV: residual volume
TLC: total lung capacity
VC: vital capacity
While some changes in cognition are observed in normal aging, some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may experience more cognitive impairment than expected, which affects intellectual performance or daily functioning. This unexpected impairment should prompt an evaluation.