Hematopoietic growth factors are a family of glycoproteins Glycoproteins Conjugated protein-carbohydrate compounds including mucins, mucoid, and amyloid glycoproteins. Basics of Carbohydrates responsible for the proliferation and differentiation of hematopoietic progenitor cells in the bone marrow Bone marrow The soft tissue filling the cavities of bones. Bone marrow exists in two types, yellow and red. Yellow marrow is found in the large cavities of large bones and consists mostly of fat cells and a few primitive blood cells. Red marrow is a hematopoietic tissue and is the site of production of erythrocytes and granular leukocytes. Bone marrow is made up of a framework of connective tissue containing branching fibers with the frame being filled with marrow cells. Bone Marrow: Composition and Hematopoiesis. Pharmacologic erythropoietin Erythropoietin Glycoprotein hormone, secreted chiefly by the kidney in the adult and the liver in the fetus, that acts on erythroid stem cells of the bone marrow to stimulate proliferation and differentiation. Erythrocytes: Histology, thrombopoietin Thrombopoietin A humoral factor that stimulates the production of thrombocytes (blood platelets). Thrombopoietin stimulates the proliferation of bone marrow megakaryocytes and their release of blood platelets. The process is called thrombopoiesis. Platelets: Histology, granulocyte colony-stimulating factor Granulocyte colony-stimulating factor A glycoprotein of mw 25 kda containing internal disulfide bonds. It induces the survival, proliferation, and differentiation of neutrophilic granulocyte precursor cells and functionally activates mature blood neutrophils. Among the family of colony-stimulating factors, G-CSF is the most potent inducer of terminal differentiation to granulocytes and macrophages of leukemic myeloid cell lines. White Myeloid Cells: Histology (G-CSF), and granulocyte macrophage colony-stimulating factor Macrophage colony-stimulating factor A mononuclear phagocyte colony-stimulating factor (M-CSF) synthesized by mesenchymal cells. The compound stimulates the survival, proliferation, and differentiation of hematopoietic cells of the monocyte-macrophage series. M-CSF is a disulfide-bonded glycoprotein dimer with a mw of 70 kda. It binds to a specific high affinity receptor. White Myeloid Cells: Histology ( GM-CSF GM-CSF An acidic glycoprotein of mw 23 kda with internal disulfide bonds. The protein is produced in response to a number of inflammatory mediators by mesenchymal cells present in the hemopoietic environment and at peripheral sites of inflammation. GM-CSF is able to stimulate the production of neutrophilic granulocytes, macrophages, and mixed granulocyte-macrophage colonies from bone marrow cells and can stimulate the formation of eosinophil colonies from fetal liver progenitor cells. GM-CSF can also stimulate some functional activities in mature granulocytes and macrophages. White Myeloid Cells: Histology) are used in certain cases in which normal hematopoiesis Hematopoiesis The development and formation of various types of blood cells. Hematopoiesis can take place in the bone marrow (medullary) or outside the bone marrow (extramedullary hematopoiesis). Bone Marrow: Composition and Hematopoiesis is impaired owing to treatment (e.g., chemotherapy Chemotherapy Osteosarcoma) or underlying disease (e.g., aplastic anemia Aplastic Anemia Aplastic anemia (AA) is a rare, life-threatening condition characterized by pancytopenia and hypocellularity of the bone marrow (in the absence of any abnormal cells) reflecting damage to hematopoietic stem cells. Aplastic anemia can be acquired or inherited, however, most cases of AA are acquired and caused by autoimmune damage to hematopoietic stem cells. Aplastic Anemia). Commonly, erythropoiesis-stimulating agents (ESAs) are given as part of the treatment of chemotherapy-induced anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types and anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types secondary to CKD CKD Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease. G-CSF and GM-CSF GM-CSF An acidic glycoprotein of mw 23 kda with internal disulfide bonds. The protein is produced in response to a number of inflammatory mediators by mesenchymal cells present in the hemopoietic environment and at peripheral sites of inflammation. GM-CSF is able to stimulate the production of neutrophilic granulocytes, macrophages, and mixed granulocyte-macrophage colonies from bone marrow cells and can stimulate the formation of eosinophil colonies from fetal liver progenitor cells. GM-CSF can also stimulate some functional activities in mature granulocytes and macrophages. White Myeloid Cells: Histology are administered to treat chemotherapy-induced neutropenia Neutropenia Neutrophils are an important component of the immune system and play a significant role in the eradication of infections. Low numbers of circulating neutrophils, referred to as neutropenia, predispose the body to recurrent infections or sepsis, though patients can also be asymptomatic. Neutropenia. Thrombopoiesis-stimulating agents are used in the prevention or treatment of thrombocytopenia Thrombocytopenia Thrombocytopenia occurs when the platelet count is < 150,000 per microliter. The normal range for platelets is usually 150,000-450,000/µL of whole blood. Thrombocytopenia can be a result of decreased production, increased destruction, or splenic sequestration of platelets. Patients are often asymptomatic until platelet counts are < 50,000/µL. Thrombocytopenia.
Last updated: Mar 6, 2023
Hematopoietic growth factors are glycoproteins Glycoproteins Conjugated protein-carbohydrate compounds including mucins, mucoid, and amyloid glycoproteins. Basics of Carbohydrates that regulate the proliferation, differentiation, and maturation of progenitor cells, as well as the function of the mature cells.
| Cytokines Cytokines Non-antibody proteins secreted by inflammatory leukocytes and some non-leukocytic cells, that act as intercellular mediators. They differ from classical hormones in that they are produced by a number of tissue or cell types rather than by specialized glands. They generally act locally in a paracrine or autocrine rather than endocrine manner. Adaptive Immune Response/growth factors | Activities | Pharmacologic agent(s) |
|---|---|---|
| Erythropoietin Erythropoietin Glycoprotein hormone, secreted chiefly by the kidney in the adult and the liver in the fetus, that acts on erythroid stem cells of the bone marrow to stimulate proliferation and differentiation. Erythrocytes: Histology ( EPO EPO Glycoprotein hormone, secreted chiefly by the kidney in the adult and the liver in the fetus, that acts on erythroid stem cells of the bone marrow to stimulate proliferation and differentiation. Erythrocytes: Histology) | Stimulates erythropoiesis Erythropoiesis The production of red blood cells (erythrocytes). In humans, erythrocytes are produced by the yolk sac in the first trimester; by the liver in the second trimester; by the bone marrow in the third trimester and after birth. In normal individuals, the erythrocyte count in the peripheral blood remains relatively constant implying a balance between the rate of erythrocyte production and rate of destruction. Erythrocytes: Histology, including differentiation |
|
| Granulocyte macrophage colony-stimulating factor Macrophage colony-stimulating factor A mononuclear phagocyte colony-stimulating factor (M-CSF) synthesized by mesenchymal cells. The compound stimulates the survival, proliferation, and differentiation of hematopoietic cells of the monocyte-macrophage series. M-CSF is a disulfide-bonded glycoprotein dimer with a mw of 70 kda. It binds to a specific high affinity receptor. White Myeloid Cells: Histology ( GM-CSF GM-CSF An acidic glycoprotein of mw 23 kda with internal disulfide bonds. The protein is produced in response to a number of inflammatory mediators by mesenchymal cells present in the hemopoietic environment and at peripheral sites of inflammation. GM-CSF is able to stimulate the production of neutrophilic granulocytes, macrophages, and mixed granulocyte-macrophage colonies from bone marrow cells and can stimulate the formation of eosinophil colonies from fetal liver progenitor cells. GM-CSF can also stimulate some functional activities in mature granulocytes and macrophages. White Myeloid Cells: Histology) | Stimulates myeloid progenitor cells Myeloid progenitor cells Stem cells derived from hematopoietic stem cells. Derived from these myeloid progenitor cells are the megakaryocytes; erythroid cells; myeloid cells; and some dendritic cells. Acute Myeloid Leukemia | Sargramostim |
| Granulocyte colony-stimulating factor Granulocyte colony-stimulating factor A glycoprotein of mw 25 kda containing internal disulfide bonds. It induces the survival, proliferation, and differentiation of neutrophilic granulocyte precursor cells and functionally activates mature blood neutrophils. Among the family of colony-stimulating factors, G-CSF is the most potent inducer of terminal differentiation to granulocytes and macrophages of leukemic myeloid cell lines. White Myeloid Cells: Histology (G-CSF) | Stimulates neutrophil precursor cells |
|
| Thrombopoietin Thrombopoietin A humoral factor that stimulates the production of thrombocytes (blood platelets). Thrombopoietin stimulates the proliferation of bone marrow megakaryocytes and their release of blood platelets. The process is called thrombopoiesis. Platelets: Histology (TPO) | Stimulates thrombopoiesis Thrombopoiesis The process of generating thrombocytes (blood platelets) from the pluripotent hematopoietic stem cells in the bone marrow via the megakaryocytes. The humoral factor with thrombopoiesis-stimulating activity is designated thrombopoietin. Platelets: Histology |
|
| IL-11 | Stimulates thrombopoiesis Thrombopoiesis The process of generating thrombocytes (blood platelets) from the pluripotent hematopoietic stem cells in the bone marrow via the megakaryocytes. The humoral factor with thrombopoiesis-stimulating activity is designated thrombopoietin. Platelets: Histology | Oprelvekin |
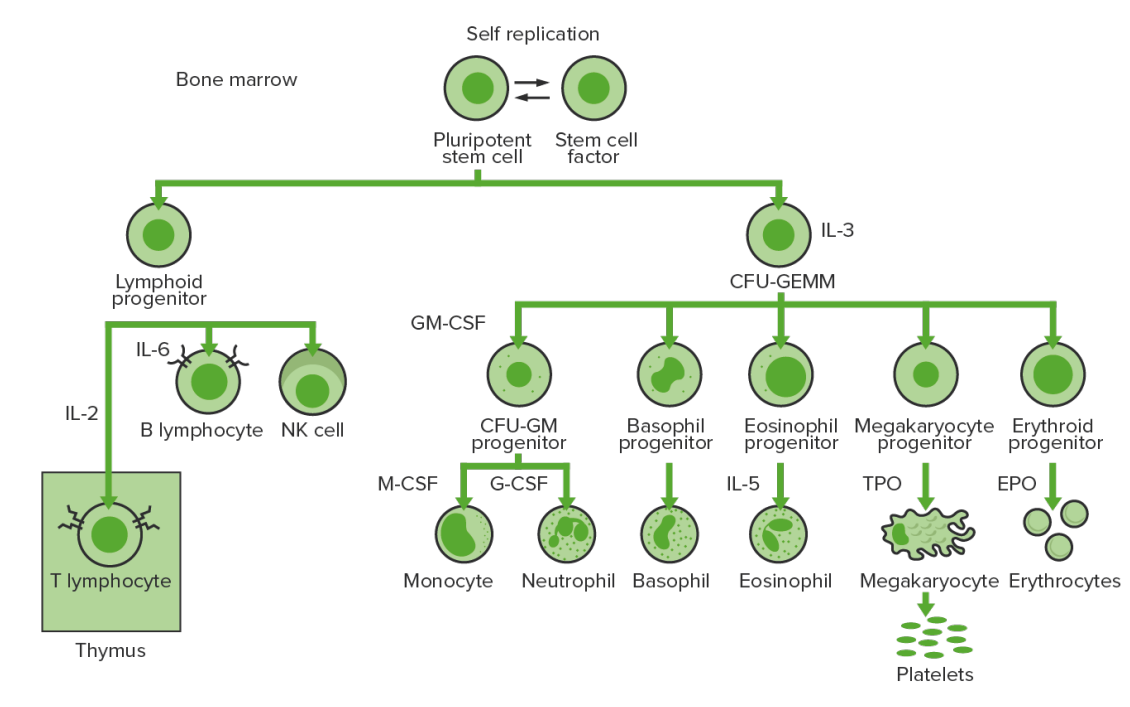
Bone marrow hematopoiesis: proliferation and differentiation of the formed elements of blood.
IL-3: interleukin-3
CFU-GEMM: colony-forming unit–granulocyte, erythrocyte, monocyte, megakaryocyte
IL-2: interleukin-2
IL-6: interleukin-6
CFU-GM: colony-forming unit–granulocyte-macrophage
GM-CSF: granulocyte-macrophage colony-stimulating factor
M-CSF: macrophage colony-stimulating factor
G-CSF: granulocyte colony-stimulating factor
IL-5: interleukin-5
NK: natural killer
TPO: thrombopoietin
EPO: erythropoietin
Erythropoiesis-stimulating agents (ESAs) are pharmacologic substances that stimulate the production of RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology and are used to treat anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types due to a variety of conditions.
| Agent | Mechanism of action | Pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics | Indications |
|---|---|---|---|
| Epoetin alfa |
|
|
|
| Darbepoetin alfa |
|
Anemia
Anemia
Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology.
Anemia: Overview and Types 2 degrees to:
|
|
| Methoxy polyethylene glycol Polyethylene Glycol Laxatives–epoetin beta |
|
Anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types 2 degrees to CKD CKD Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease |
Myeloid growth factors are agents that stimulate proliferation and differentiation of ≥ 1 myeloid cell types and are used to treat low neutrophil counts.
| Agent | Mechanism of action | Pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics | Indications |
|---|---|---|---|
| Filgrastim |
|
|
|
| Pegfilgrastim |
|
|
|
| Sargramostim |
|
|
|
Thrombopoietic growth factors stimulate thrombopoiesis Thrombopoiesis The process of generating thrombocytes (blood platelets) from the pluripotent hematopoietic stem cells in the bone marrow via the megakaryocytes. The humoral factor with thrombopoiesis-stimulating activity is designated thrombopoietin. Platelets: Histology via the action of IL-11 or through the activation of TPO receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors.
| Agent | Mechanism of action | Pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics | Indications |
|---|---|---|---|
| Oprelvekin | Stimulates megakaryocytopoiesis and thrombopoiesis Thrombopoiesis The process of generating thrombocytes (blood platelets) from the pluripotent hematopoietic stem cells in the bone marrow via the megakaryocytes. The humoral factor with thrombopoiesis-stimulating activity is designated thrombopoietin. Platelets: Histology |
|
Prevent severe thrombocytopenia Severe Thrombocytopenia Thrombocytopenia in those undergoing chemotherapy Chemotherapy Osteosarcoma for nonmyeloid cancer |
| Romiplostim | ↑ Platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology by binding TPO receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors |
|
|
| Eltrombopag |
|
|
For all agents, hypersensitivity to drug or components is a contraindication.