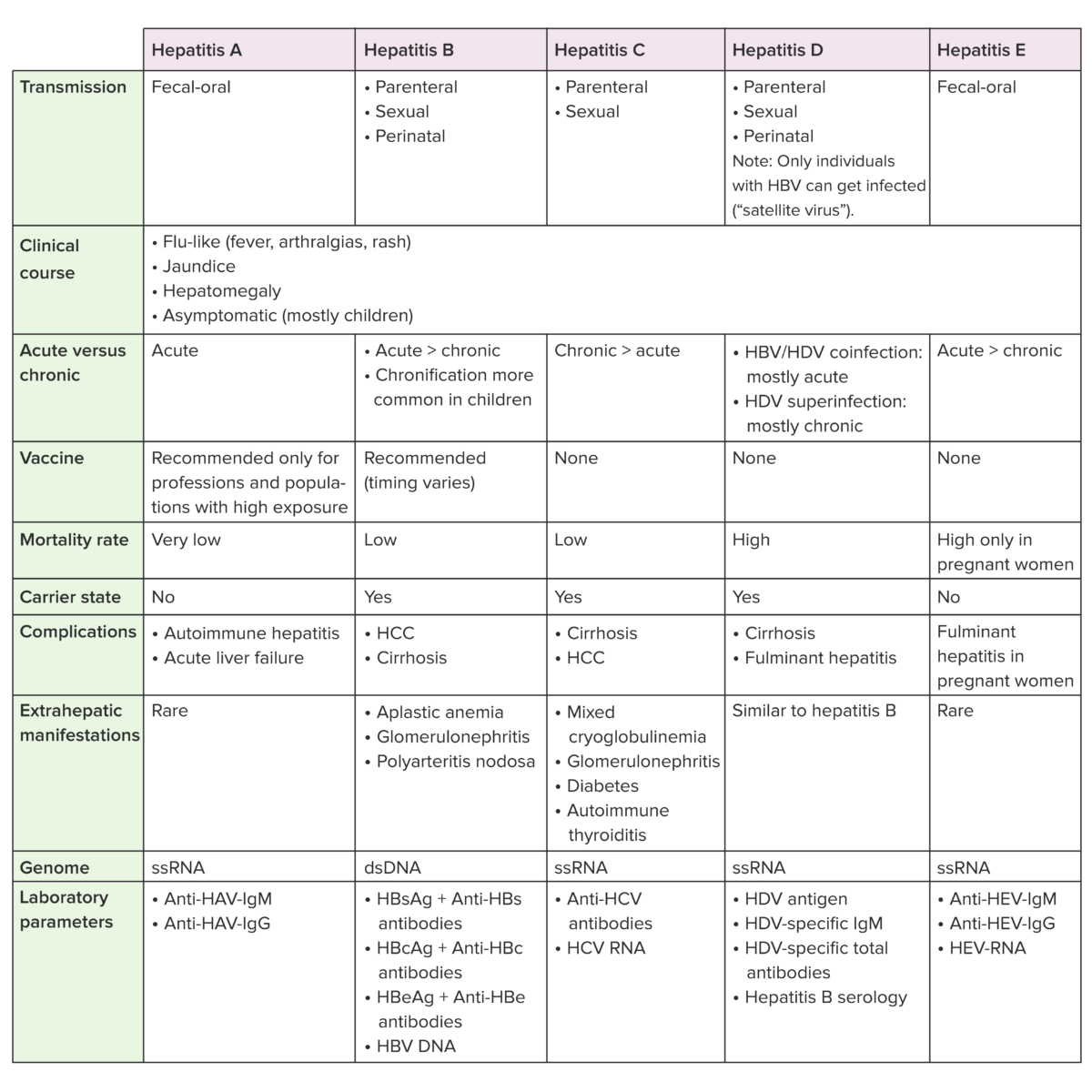
Hepatitis D virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology (HDV) is a small enveloped, single-stranded RNA RNA A polynucleotide consisting essentially of chains with a repeating backbone of phosphate and ribose units to which nitrogenous bases are attached. RNA is unique among biological macromolecules in that it can encode genetic information, serve as an abundant structural component of cells, and also possesses catalytic activity. RNA Types and Structure virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology. Hepatitis D virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology is considered a satellite virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology, as it requires the presence of hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( HBV HBV Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Hepatitis B virus is transmitted by exposure to infectious blood or body fluids. Examples of types of exposure include sexual intercourse, IV drug use, and childbirth. Hepatitis B Virus) for assembly and secretion Secretion Coagulation Studies. Therefore, in order for an individual to contract hepatitis D, coinfection or superinfection with HBV HBV Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Hepatitis B virus is transmitted by exposure to infectious blood or body fluids. Examples of types of exposure include sexual intercourse, IV drug use, and childbirth. Hepatitis B Virus is required. Like HBV HBV Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Hepatitis B virus is transmitted by exposure to infectious blood or body fluids. Examples of types of exposure include sexual intercourse, IV drug use, and childbirth. Hepatitis B Virus, HDV is transmitted parenterally, through unprotected sexual intercourse, or perinatally. Clinical presentation is that of a classical viral hepatitis, including coinfection of HDV and HBV HBV Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Hepatitis B virus is transmitted by exposure to infectious blood or body fluids. Examples of types of exposure include sexual intercourse, IV drug use, and childbirth. Hepatitis B Virus, which is considered the most serious form of hepatitis because of the high mortality Mortality All deaths reported in a given population. Measures of Health Status rate. For acute cases, management is supportive, whereas for chronic cases, pegylated interferon alfa Pegylated interferon alfa Hepatitis B Virus (PEG-IFN-α) is needed.
Last updated: Sep 12, 2024
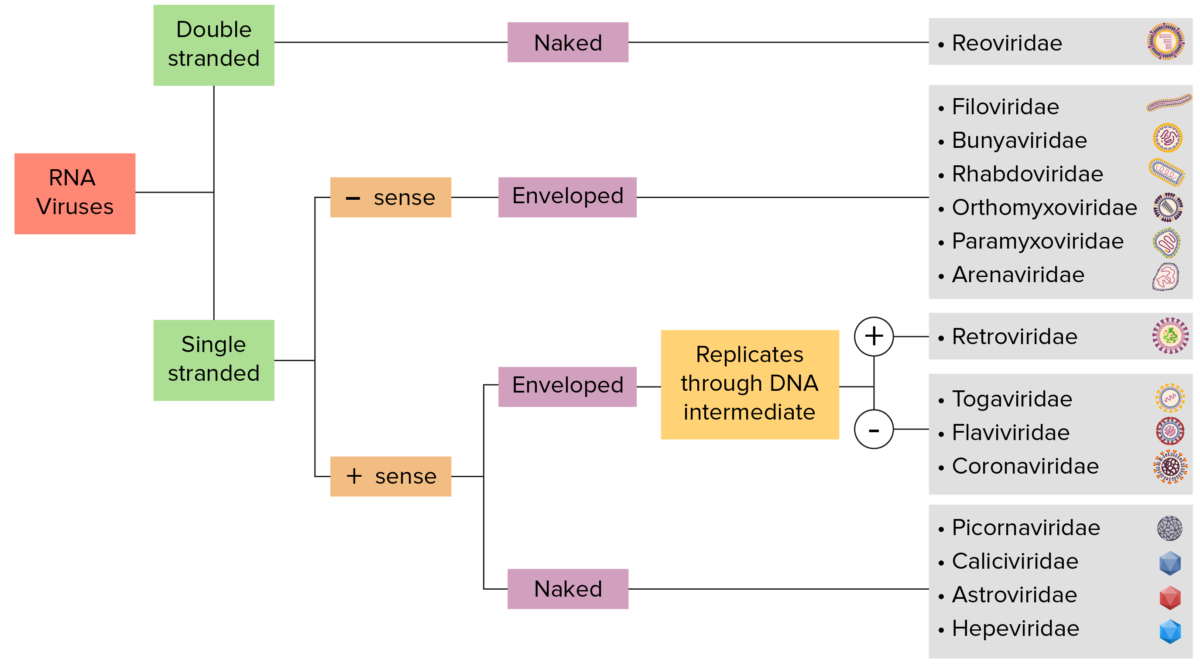
RNA virus identification:
Viruses can be classified in many ways. Most viruses have a genome formed by either DNA or RNA. Viruses of the RNA genome can be further characterized by either a single- or double-stranded RNA. “Enveloped” viruses are covered by a thin coat of cell membrane (usually taken from the host cell). If the coat is absent, the viruses are called “naked” viruses. Viruses with single-stranded genomes are “positive-sense” viruses if the genome is directly employed as mRNA, which is translated into proteins. “Negative-sense,” single-stranded viruses employ RNA-dependent RNA polymerase, a viral enzyme, to transcribe the genome into mRNA.
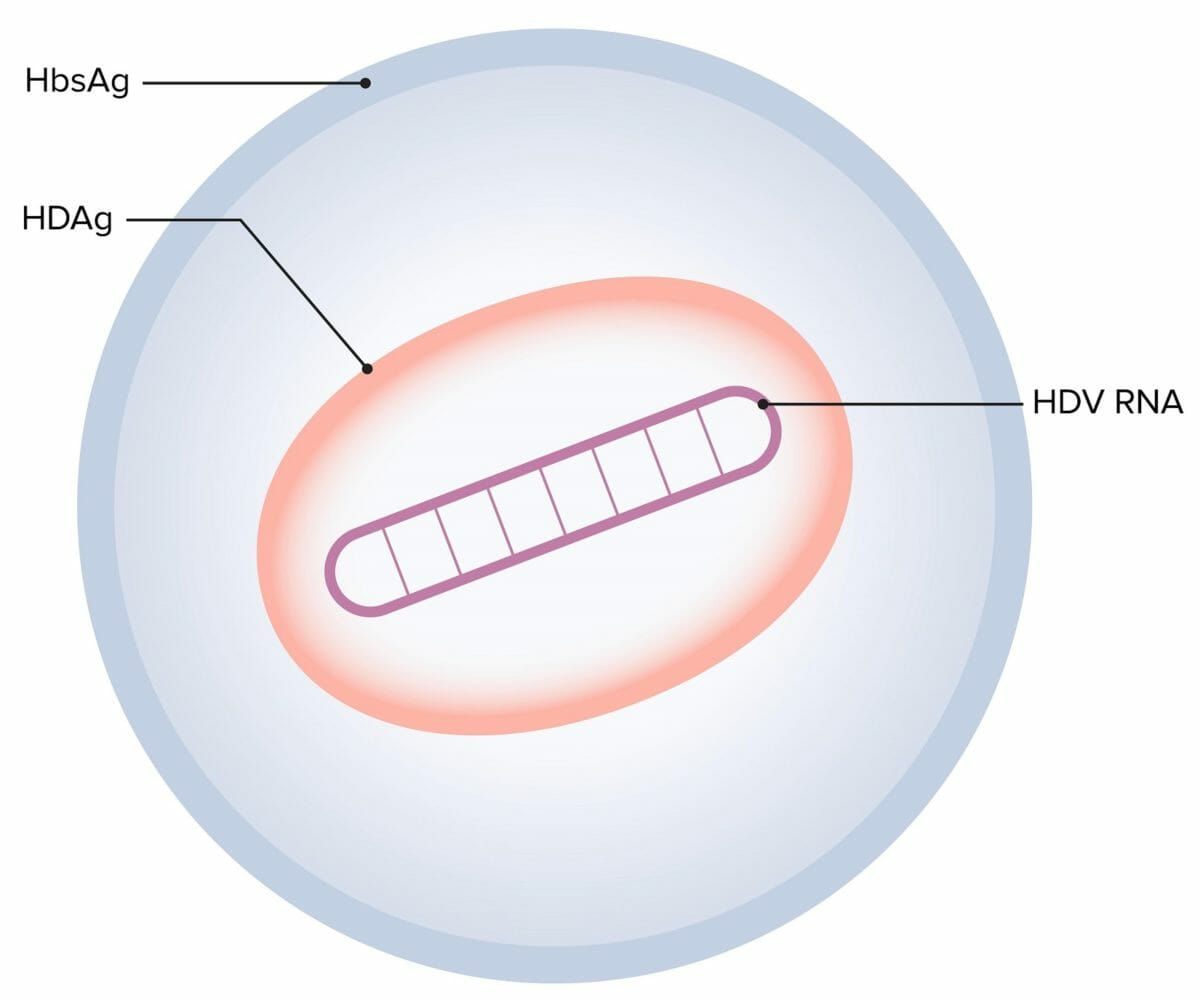
Hepatitis D virus (HDV):
The hepatitis D virion consists of single-stranded circular RNA (HDV RNA), a single HDV-encoded antigen (HDAg), and a lipoprotein envelope (HbsAg), which is provided by the hepatitis B virus (HBV).
Transmission of hepatitis D is similar to that of hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus.
| Serum markers | Acute HBV HBV Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Hepatitis B virus is transmitted by exposure to infectious blood or body fluids. Examples of types of exposure include sexual intercourse, IV drug use, and childbirth. Hepatitis B Virus/HDV coinfection | Acute HDV superinfection | Chronic HDV infection |
|---|---|---|---|
| HBsAg | Positive | Positive | Positive |
| Anti-HBc anti-HBc Hepatitis B Virus IgM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions | Positive | Negative | Negative |
| Serum HDV RNA RNA A polynucleotide consisting essentially of chains with a repeating backbone of phosphate and ribose units to which nitrogenous bases are attached. RNA is unique among biological macromolecules in that it can encode genetic information, serve as an abundant structural component of cells, and also possesses catalytic activity. RNA Types and Structure | Early, transient | Early, persistent | Positive |
| Serum HDAg* | Positive (transient) | Positive (transient) | Negative |
| Anti-HDV IgM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions | Positive (transient) | Positive (persistent and increasing titers) | Positive (high titers) |
| Anti-HDV IgG IgG The major immunoglobulin isotype class in normal human serum. There are several isotype subclasses of igg, for example, igg1, igg2a, and igg2b. Hypersensitivity Pneumonitis | Positive (late) | Positive (late) | Positive (high titers) |
Anti-HBc: hepatitis B core antibody
Anti-HBs: hepatitis B surface antibody
HBcAg: hepatitis B core antigen
HBsAg: hepatitis B surface antigen
HBV: hepatitis B virus
HCC: hepatocellular carcinoma
HAV: hepatitis A virus
HCV: hepatitis C virus
HDV: hepatitis D virus