Ankylosing spondylitis (also known as Bechterew’s disease or Marie-Strümpell disease) is a seronegative spondyloarthropathy characterized by chronic and indolent inflammation of the axial skeleton. Severe disease can lead to fusion and rigidity of the spine. Ankylosing spondylitis is most often seen in young men and is strongly associated with HLA-B27. Patients will have progressive back pain (which improves with activity), morning stiffness, and decreased range of motion of the spine. Extra-articular manifestations include fatigue, enthesitis, anterior uveitis, restrictive lung disease, and inflammatory bowel disease. The diagnosis is based on the clinical history, physical exam, and imaging demonstrating sacroiliitis and bridging syndesmophytes. Most patients are managed with physical therapy and nonsteroidal anti-inflammatory drugs (NSAIDs). More severe cases may require tumor necrosis factor-alpha inhibitors or surgery.
Last updated: Mar 4, 2024
Ankylosing spondylitis Ankylosing spondylitis Ankylosing spondylitis (also known as Bechterew’s disease or Marie-Strümpell disease) is a seronegative spondyloarthropathy characterized by chronic and indolent inflammation of the axial skeleton. Severe disease can lead to fusion and rigidity of the spine. Ankylosing Spondylitis (AS) is a seronegative spondyloarthropathy Spondyloarthropathy Ankylosing Spondylitis characterized by chronic and indolent inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the axial Axial Computed Tomography (CT) skeleton.
To remember the seronegative spondyloarthropathies Spondyloarthropathies Examination of the Lower Limbs, use the mnemonic “PAIR.”
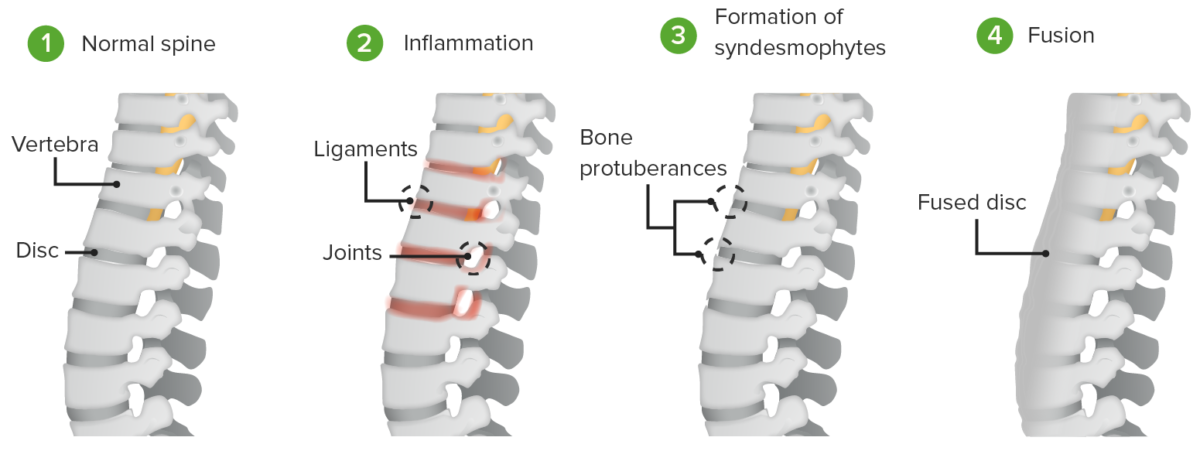
Pathogenesis of ankylosing spondylitis:
Inflammation induces the formation of syndesmophytes and the fusion of the intervertebral discs and vertebral bodies.
Pathogenesis of ankylosing spondylitis:
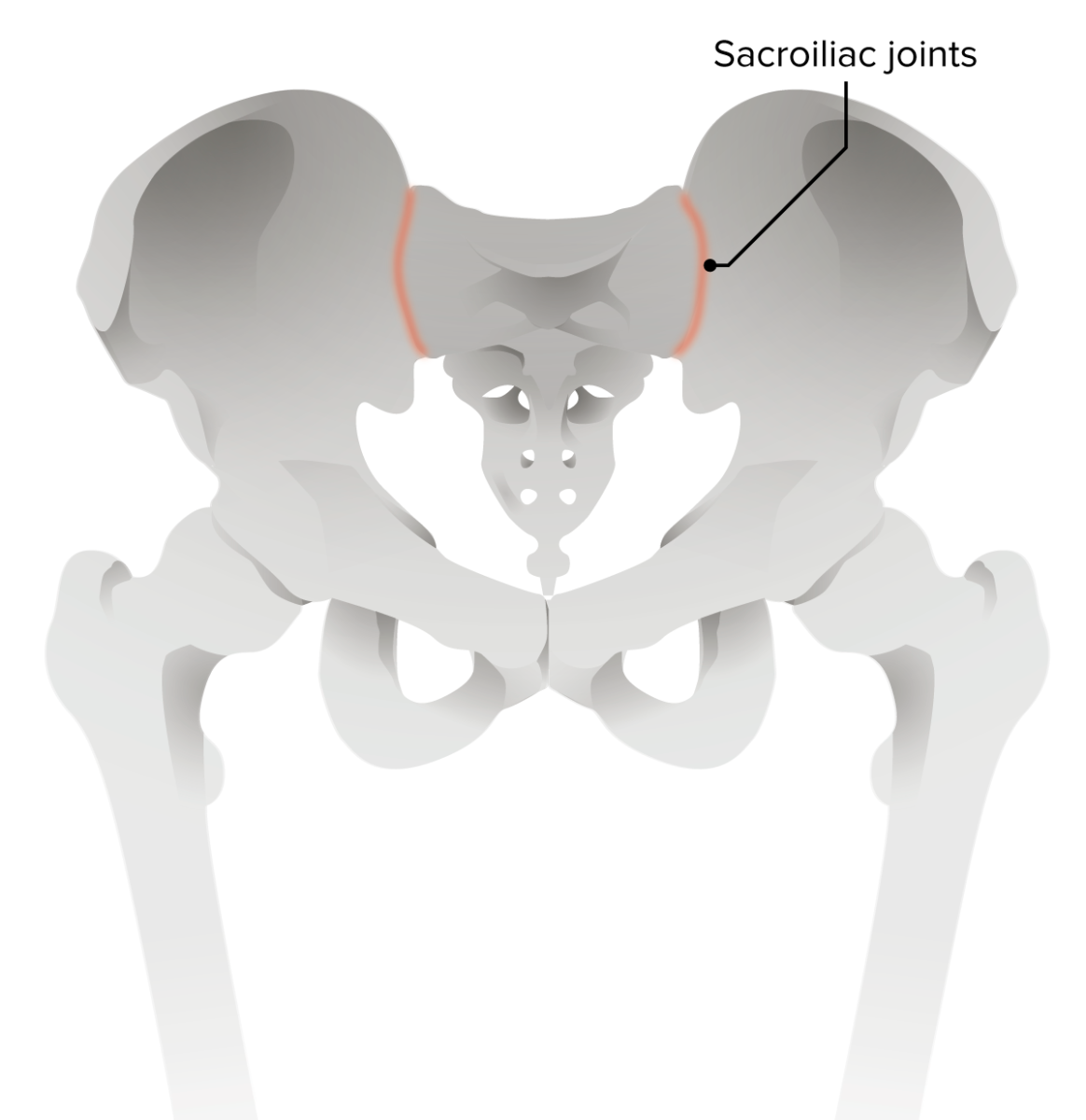
Erosion of the iliac side of sacroiliac joints is the earliest radiologic sign of ankylosing spondylitis.
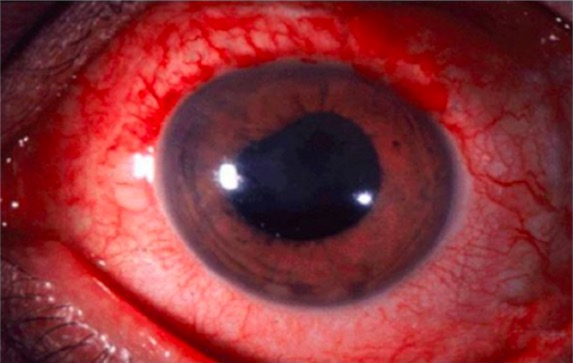
Anterior uveitis is a common extra-articular manifestation of ankylosing spondylitis.
Image: “Anterior uveitis” by Christopher J. Gilani et al. License: CC BY 4.0
Dactylitis of the 3rd digit in ankylosing spondylitis
Image: “Involvement of the feet in patients with SpA” by Department of Rheumatology, Hospital General de México, Faculty of Medicine, Universidad Nacional Autónoma de México, Dr, Balmis 148, Colonia Doctores, México, DF 06720, Mexico. License: CC BY 2.0, cropped by Lecturio.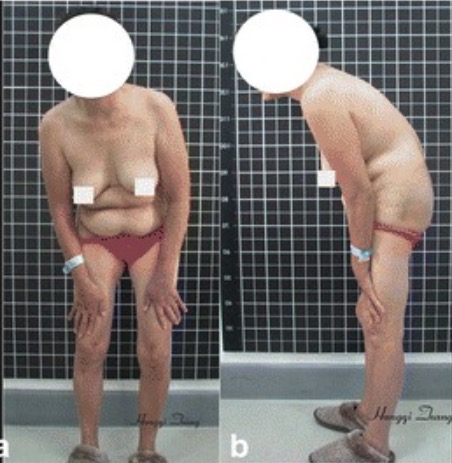
Stooped, forward-flexed position in a patient with ankylosing spondylitis
Image: “Preoperative imaging” by Hongqi Zhang et al. License: CC BY 4.0, cropped by Lecturio.Refer patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with the following clinical features to a rheumatologist:
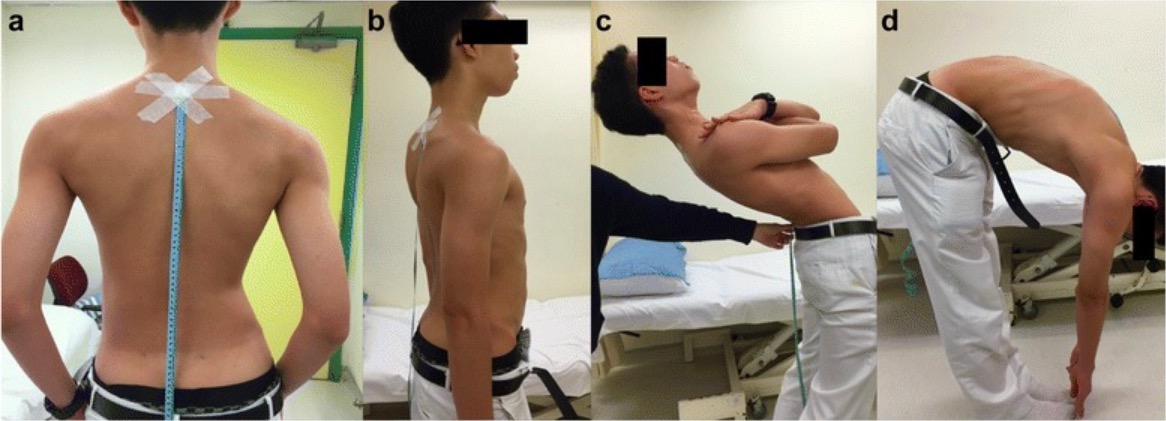
The Schober test: a photograph of a patient demonstrating the Schober test for spinal mobility. After the marks are placed 10 cm and 5 cm away from the spinal process of L5, the patient is asked to bend over. If distance does not increase by > 5 cm, the patient has reduced lumbar flexion indicative of ankylosing spondylitis.
Image: “Schober test” by Kamil Eyvazov et al. License: CC BY 4.0
The FABER test:
This test may be used to detect hip, lumbar, or sacroiliac joint pathology. These signs are often positive in ankylosing spondylitis.
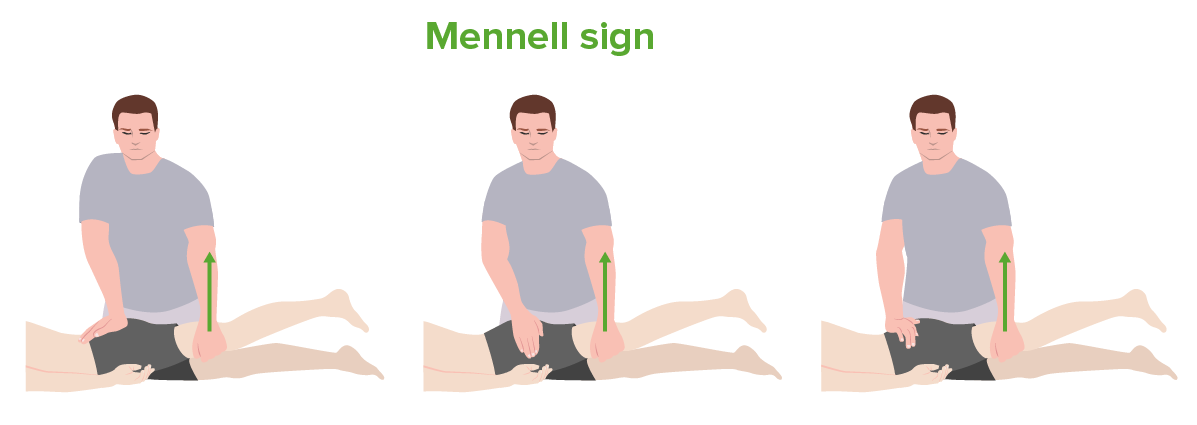
The Mennell sign:
From left to right: testing of the sacroiliac joint, hip joint, and lumbar spine. This test may be used in the evaluation for ankylosing spondylitis.
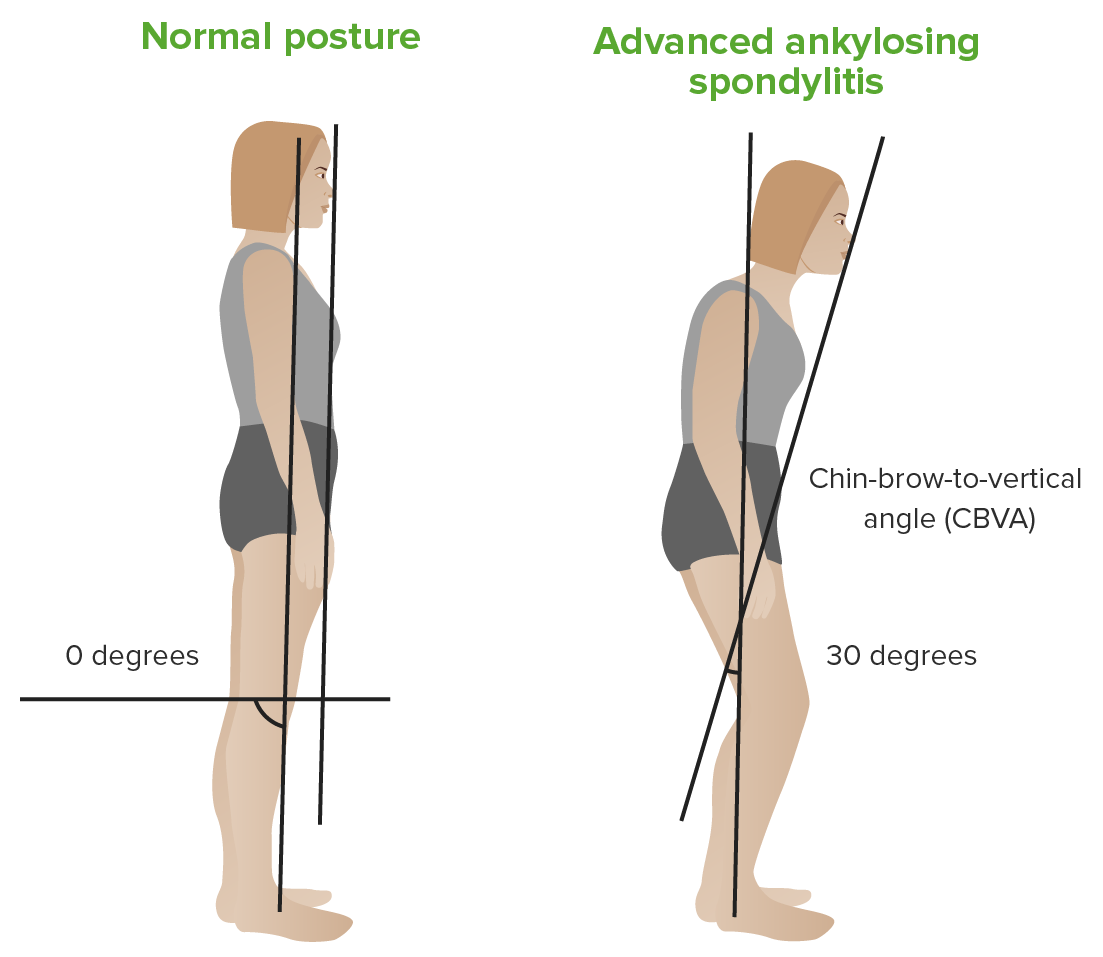
Chin–brow vertical angle:
Left: patient with a normal back
Right: patient with ankylosing spondylitis

Lateral lumbar spine radiograph in ankylosing spondylitis:
This image demonstrates squaring of the vertebrae with a “bamboo stick” appearance due to bridging syndesmophytes.

MRI of the sacroiliac joint in ankylosing spondylitis:
The arrows point to enhancement of the right sacroiliac joint, indicating sacroiliitis.
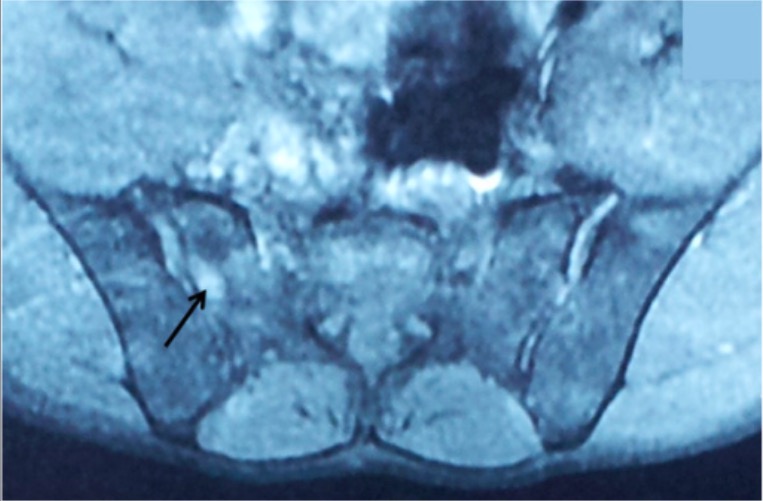
MRI of the sacroiliac joints in ankylosing spondylitis:
This image shows bilateral sacroiliitis with a hyperintense signal on T2 (arrow) at the SI joint.
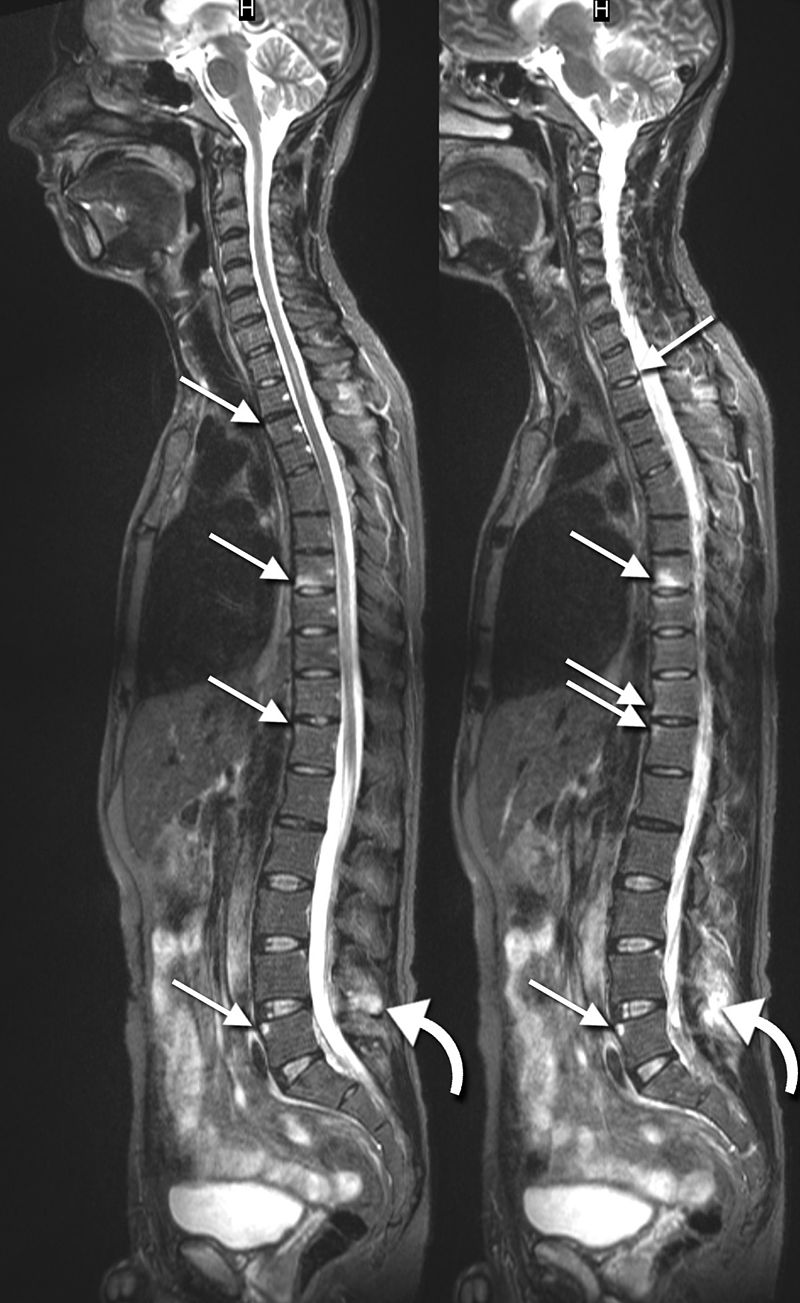
Sagittal MRIs in ankylosing spondylitis:
These images show inflammatory lesions in the thoracic and lumbar spine (arrows). Inflammatory lesions of the spinous process are also shown at L4 (curved arrows).

Radiograph of the pelvis in ankylosing spondylitis:
This image demonstrates advanced sacroiliitis with fusion of the SI joints.
Management requires a multidisciplinary approach to reduce pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, increase range of motion Range of motion The distance and direction to which a bone joint can be extended. Range of motion is a function of the condition of the joints, muscles, and connective tissues involved. Joint flexibility can be improved through appropriate muscle strength exercises. Examination of the Upper Limbs, decrease inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, and improve quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement of life.
Management by a rheumatologist, in coordination Coordination Cerebellar Disorders with a multidisciplinary team, is recommended.
Initial therapy:[13–15,20]
2nd line:
3rd line (unresponsive to TNFi): use another TNFi or use IL-17 inhibitors IL-17 inhibitors Ankylosing Spondylitis[14,15]