Lung cancer Lung cancer Lung cancer is the malignant transformation of lung tissue and the leading cause of cancer-related deaths. The majority of cases are associated with long-term smoking. The disease is generally classified histologically as either small cell lung cancer or non-small cell lung cancer. Symptoms include cough, dyspnea, weight loss, and chest discomfort. Lung Cancer is the leading cause of cancer-related death in the United States, with 90% of cases being fatal. The vast majority of cases are associated with smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, and thus smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases cessation is encouraged to reduce a patient’s lifetime risk. Annual screening Screening Preoperative Care with low-dose computed tomography is recommended for early detection in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship 50–80 years of age with a significant smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases history. This screening Screening Preoperative Care program has been shown to significantly reduce mortality Mortality All deaths reported in a given population. Measures of Health Status.
Last updated: Mar 2, 2025
Lung cancer Lung cancer Lung cancer is the malignant transformation of lung tissue and the leading cause of cancer-related deaths. The majority of cases are associated with long-term smoking. The disease is generally classified histologically as either small cell lung cancer or non-small cell lung cancer. Symptoms include cough, dyspnea, weight loss, and chest discomfort. Lung Cancer is a malignant tumor Tumor Inflammation of the lung originating from the respiratory epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology of the bronchi Bronchi The larger air passages of the lungs arising from the terminal bifurcation of the trachea. They include the largest two primary bronchi which branch out into secondary bronchi, and tertiary bronchi which extend into bronchioles and pulmonary alveoli. Bronchial Tree: Anatomy, bronchioles Bronchioles The small airways branching off the tertiary bronchi. Terminal bronchioles lead into several orders of respiratory bronchioles which in turn lead into alveolar ducts and then into pulmonary alveoli. Bronchial Tree: Anatomy, and alveoli Alveoli Small polyhedral outpouchings along the walls of the alveolar sacs, alveolar ducts and terminal bronchioles through the walls of which gas exchange between alveolar air and pulmonary capillary blood takes place. Acute Respiratory Distress Syndrome (ARDS).
Smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases cessation reduces the risk of lung cancer Lung cancer Lung cancer is the malignant transformation of lung tissue and the leading cause of cancer-related deaths. The majority of cases are associated with long-term smoking. The disease is generally classified histologically as either small cell lung cancer or non-small cell lung cancer. Symptoms include cough, dyspnea, weight loss, and chest discomfort. Lung Cancer.
| Category | Assessment | Follow-up |
|---|---|---|
| 0 | Incomplete | Awaiting prior CT images or images were technically inadequate |
| 1 | Negative (no lung nodules) | Continue normal annual screening Screening Preoperative Care. |
| 2 | Benign-appearing nodule Nodule Chalazion(s) | Continue normal screening Screening Preoperative Care. |
| 3 | Probably benign Benign Fibroadenoma nodule Nodule Chalazion(s) | Repeat LDCT in 6 months. |
| 4 | Suspicious | Varies and includes short-term follow-up LDCT, diagnostic CT, positron emission tomography, biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma, or surgery |
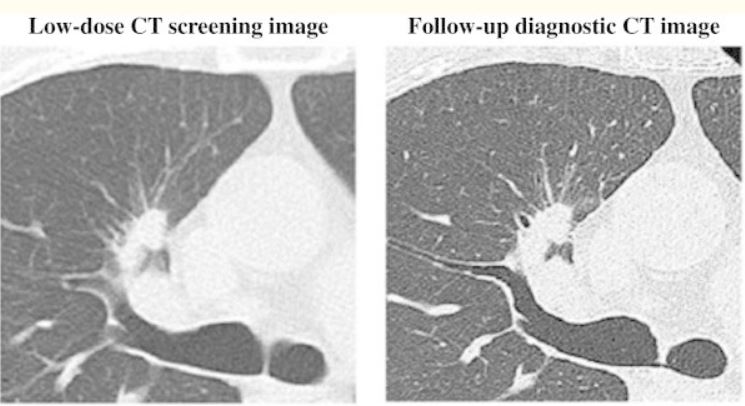
Low-dose CT screening image (left) and follow-up diagnostic CT image (right) for a patient diagnosed with adenocarcinoma
Image: “Low-dose CT scan screening for lung cancer: comparison of images and radiation doses between low-dose CT and follow-up standard diagnostic CT” by Ono K, Hiraoka T, Ono A, Komatsu E, Shigenaga T, Takaki H, Maeda T, Ogusu H, Yoshida S, Fukushima K, Kai M. License: CC BY 2.0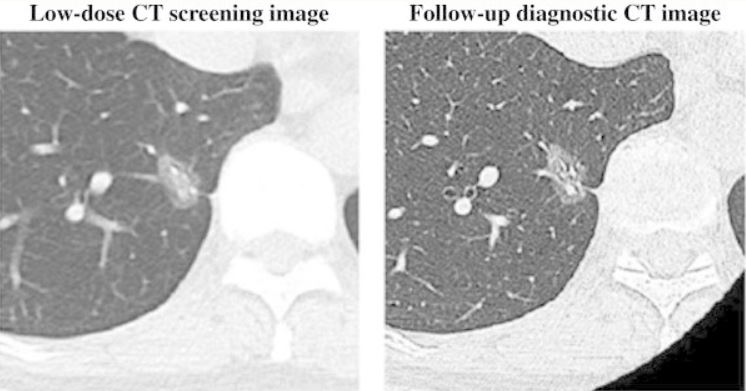
Low-dose CT screening (left) and follow-up diagnostic CT image (right) for a patient diagnosed with bronchoalveolar carcinoma
Image: “Low-dose CT scan screening for lung cancer: comparison of images and radiation doses between low-dose CT and follow-up standard diagnostic CT” by Ono K, Hiraoka T, Ono A, Komatsu E, Shigenaga T, Takaki H, Maeda T, Ogusu H, Yoshida S, Fukushima K, Kai M. License: CC BY 2.0
Chest radiograph showing a large mass in the right mid-zone, which turned out to be a bronchogenic squamous cell carcinoma
Image: “Pulmonary effects of passive smoking: the Indian experience” by Tobacco Induced Diseases. License: CC BY 2.0