The term “persistent vegetative state,” also called unresponsive wakefulness, describes the condition of individuals with severe anoxic brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification injury who have progressed to a state of wakefulness without any meaningful response to their environment. A persistent vegetative state is distinguished from a coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma in that individuals in a persistent vegetative state have intermittent sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep–wake cycles. The individual's eyes may be open and there may be some yawning, grunting Grunting Physical Examination of the Newborn, or other vocalizations. In both cases, the individual is alive, but the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification does not function fully. Persistent vegetative state is most commonly associated with anoxic brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification injury due to cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest, trauma, metabolic causes, or infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Diagnosis is made by fulfilling specific diagnostic criteria. Treatment is controversial and ethically challenging. Recovery of consciousness from a posttraumatic persistent vegetative state is unlikely after 12 months, while recovery from a nontraumatic persistent vegetative state after 3 months is exceedingly rare.
Last updated: Oct 17, 2022
Persistent vegetative state, also called unresponsive wakefulness, describes the condition of individuals with severe anoxic brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification injury who have progressed to a state of wakefulness without any meaningful response to their environment.
Arousal and wakefulness are supported by neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology that project to both thalamic and cortical neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology.
Individuals may present with persistent vegetative state several months after a traumatic or anoxic brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification injury.
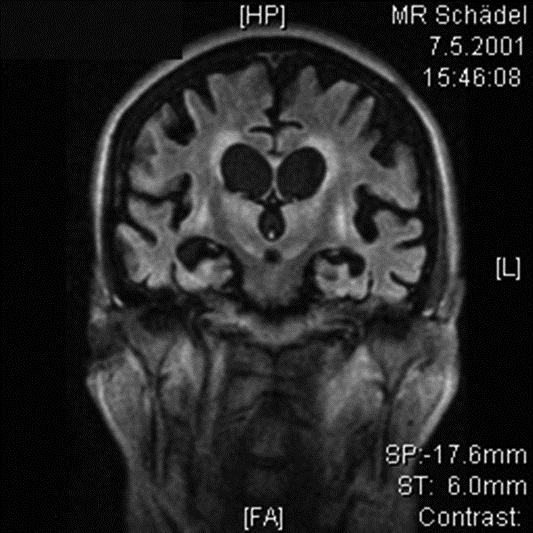
Fluorodeoxyglucose–positron emission tomography (FDG–PET) scan to evaluate brain metabolism in a 66-year-old woman in a persistent vegetative state 10 months after intraoperative cardiac arrest and severe cerebral hypoxemia:
Scan shows massive cortical and subcortical brain atrophy with dilated ventricles (normal intracranial pressure).
Individuals in a persistent vegetative state require ongoing supportive care for the prevention of complications as well as treatment of seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures if they occur.