Abdominal injuries are classified according to their mechanism of injury as blunt or penetrating. In blunt abdominal trauma, the bowel, spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy, and pelvic organs can be injured. The extent and specific type of abdominal traumatic injury can be identified by a proper history and physical examination and confirmed by appropriate imaging studies. Management depends on the patient’s stability and specific type of injury.
Last updated: Dec 5, 2022
Blunt abdominal injury is defined as damage to the abdomen and/or abdominal organs secondary to impact with a blunt (not penetrating) object or surface.
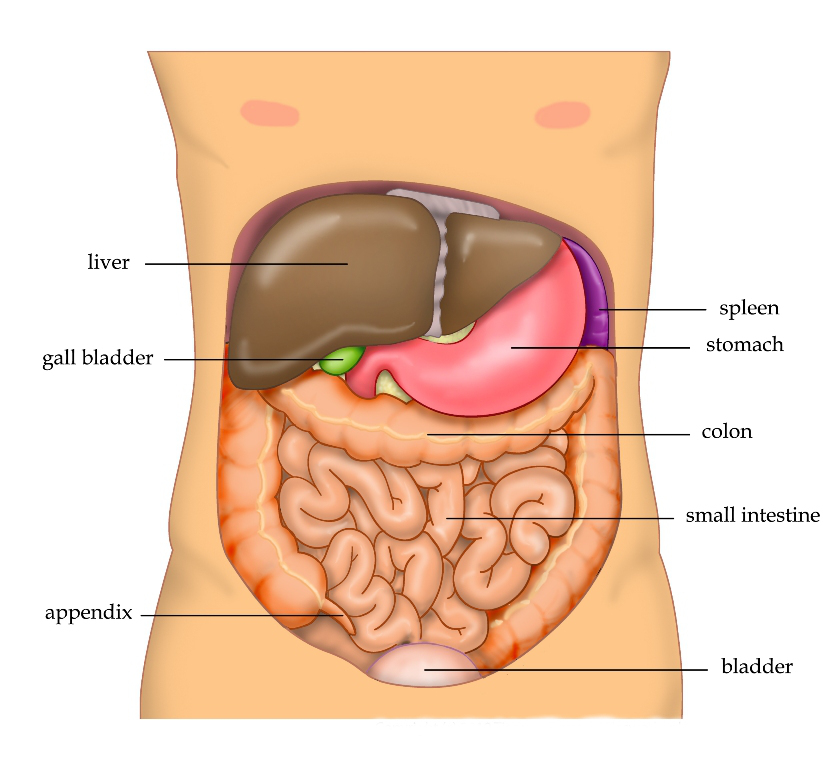
Intra-abdominal organs:
The abdomen contains many organs that may become injured in the setting of blunt trauma. Most commonly, the liver and spleen are injured.

Retroperitoneal organs:
Organs in the retroperitoneal space include the kidneys and ureters, and portions of the duodenum, colon, aorta, vena cava, and pancreas.
Blunt abdominal trauma can occur due to several pathologic processes:
Because of the wide variety and severity of injuries associated with blunt abdominal trauma, a prompt but careful history and physical exam are necessary to direct investigation with imaging studies.
| Injured organ | Features |
|---|---|
| Duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy |
|
| Spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy |
|
| Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy |
|
| Pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy |
|
| Kidney |
|

Seat belt sign:
Cutaneous injury or bruising in the pattern of a seat belt suggests significant forces at play in an MVC and may imply serious underlying injury.
Careful investigation will yield evidence of injured organs, directing further management.
| Injured organ | Management |
|---|---|
| Duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy |
|
| Spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy |
|
| Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy |
|
| Pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy |
|
| Kidney |
|