The vertebral column Vertebral column The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy is the most important anatomical and functional axis of the body, consisting of 7 cervical, 12 thoracic, and 5 lumbar vertebrae Lumbar vertebrae Vertebrae in the region of the lower back below the thoracic vertebrae and above the sacral vertebrae. Vertebral Column: Anatomy and limited cranially by the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy and caudally by the sacrum Sacrum Five fused vertebrae forming a triangle-shaped structure at the back of the pelvis. It articulates superiorly with the lumbar vertebrae, inferiorly with the coccyx, and anteriorly with the ilium of the pelvis. The sacrum strengthens and stabilizes the pelvis. Vertebral Column: Anatomy. The vertebral column Vertebral column The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy provides structural support and protection for the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy, which is housed in the spinal canal Spinal Canal The cavity within the spinal column through which the spinal cord passes. Spinal Cord Injuries. The vertebral column Vertebral column The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy and the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy may be affected by various diseases, in which different imaging methods are important for correct diagnosis and management. Radiographs and CT scans are useful in evaluating bony structures, especially in excluding fractures and checking hardware. Additionally, CT scans also provide information on soft tissues. MRI is performed for evaluation of tumors, infection, disk herniations, and other soft tissue Soft Tissue Soft Tissue Abscess abnormalities including acute ligamentous or spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy injury.
Last updated: Feb 28, 2023
Before the advent of CT and MRI, X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests imaging was widely used to study the bones of the spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy.
Views and spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy structures:
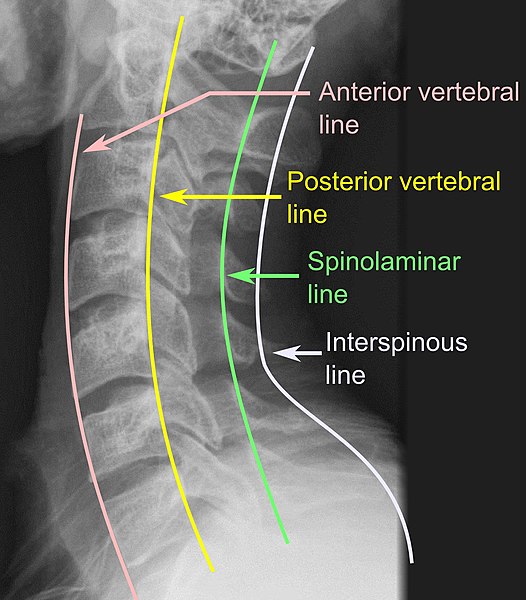
Spinal X-ray showing vertebral lines
Image: “X-ray of vertebral lines” by Mikael Häggström. License: CC0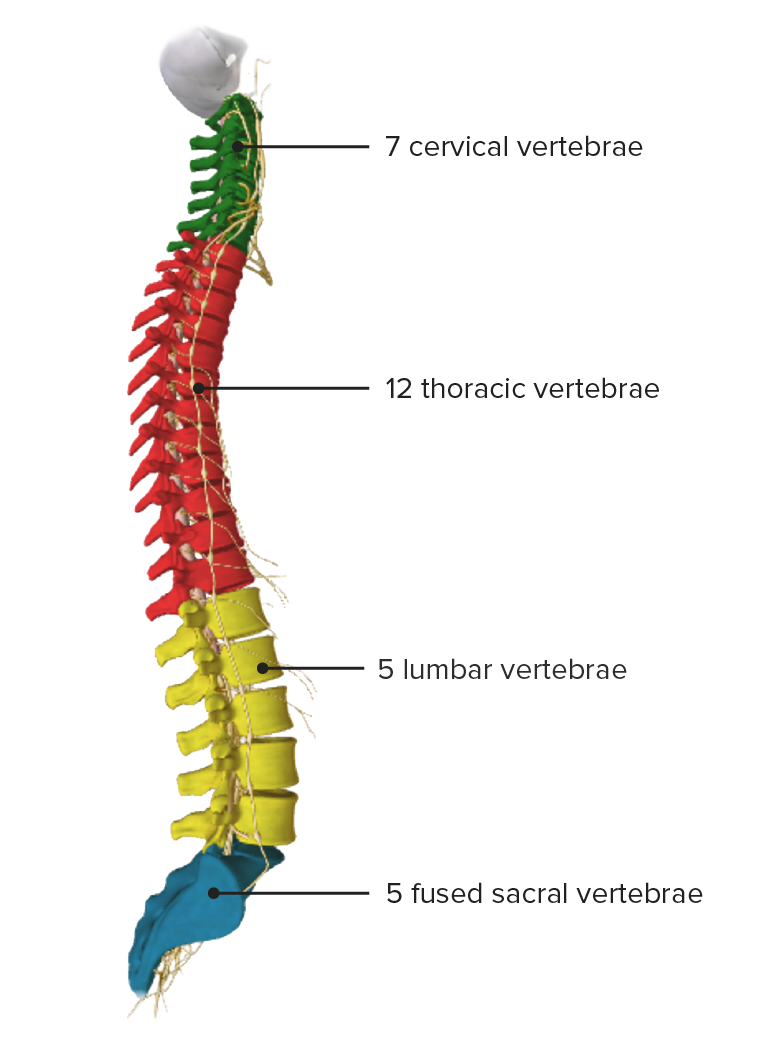
Lateral view of vertebral column showing the normal curvature (cervical and lumbar lordosis; thoracic kyphosis)
Image by Lecturio.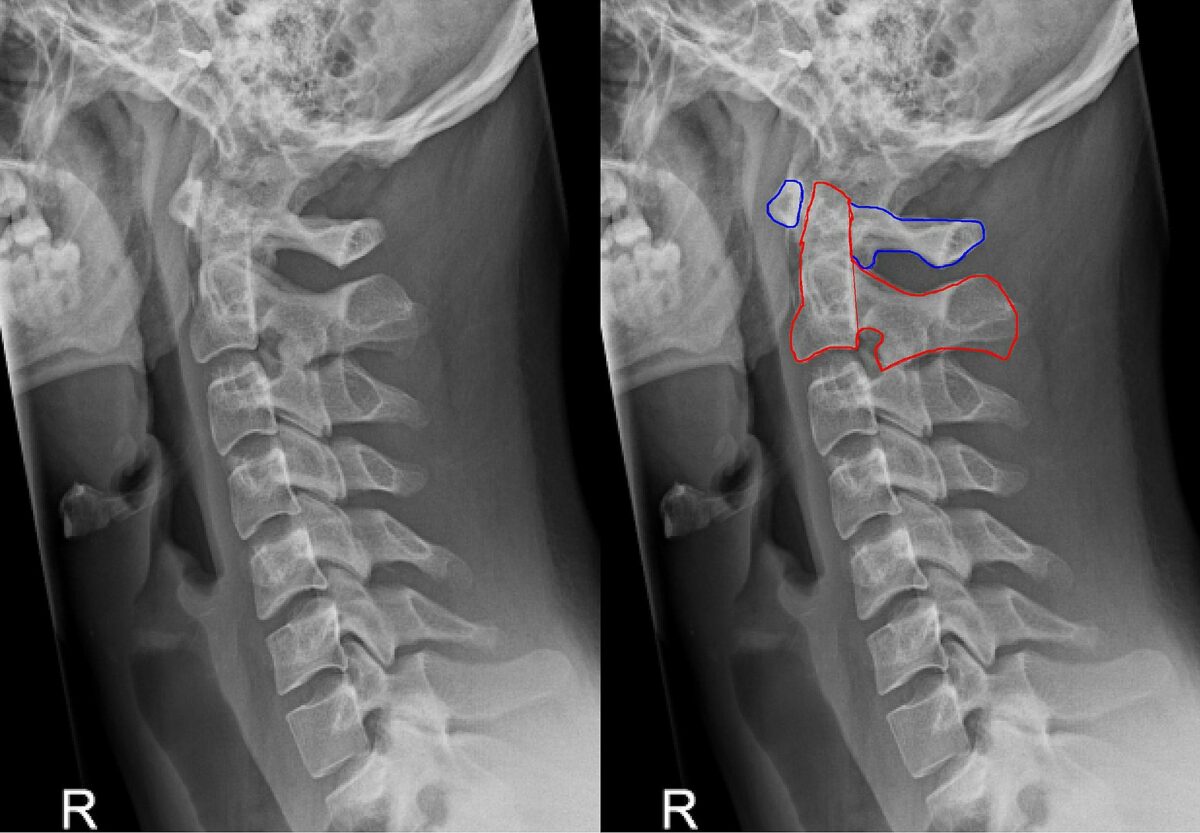
Left: Lateral cervical spine X-ray showing normal alignment at C1–2, no significant prevertebral edema, appropriate alignment of the cervical spine, and normal interspinous distances
Right: Lateral cervical spine x-ray showing C1 (blue outline) and C2 (red outline)
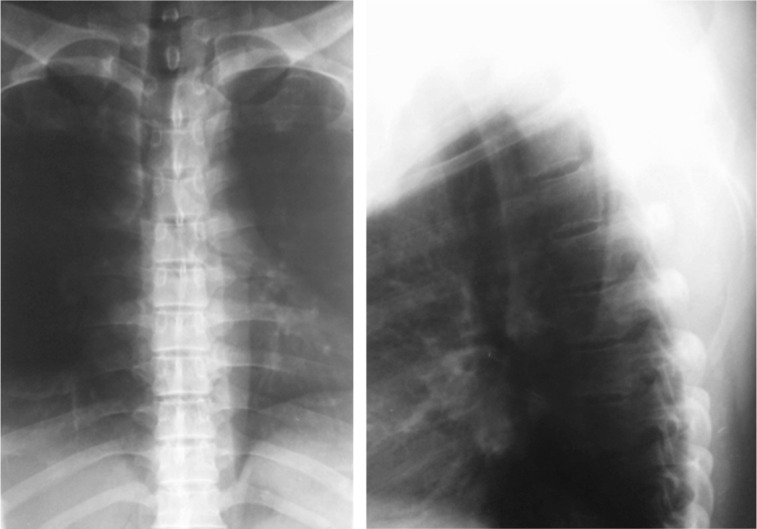
X-ray of thoracic spine (frontal on the left and lateral on the right):
The frontal view demonstrates no significant scoliotic curvature, a normal vertebral body height, and a normal-appearing trachea. The lateral view is slightly limited because of overexposure, which prevents complete visualization of the lower thoracic spine, although the visualized vertebral elements are unremarkable.
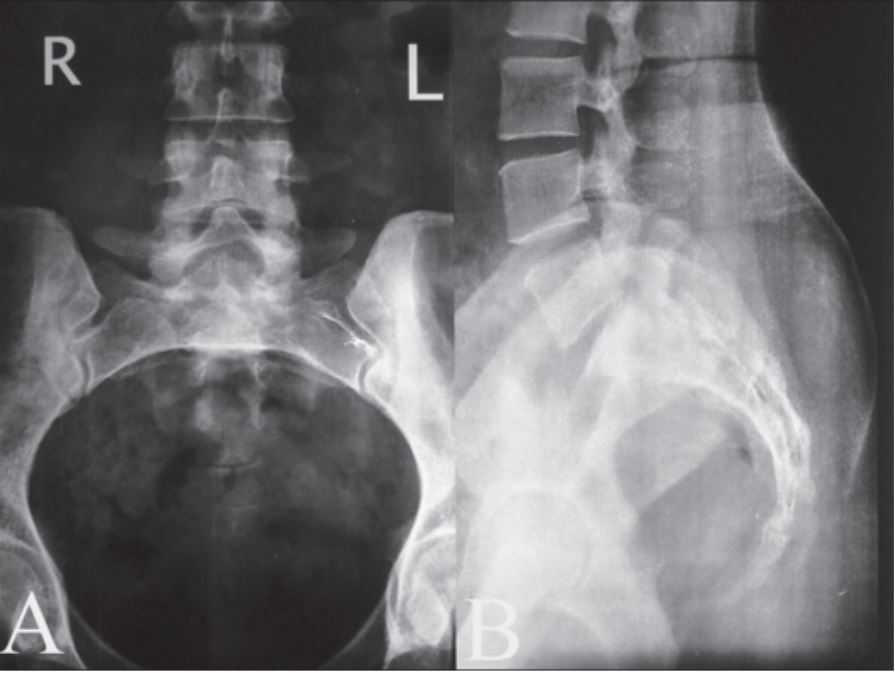
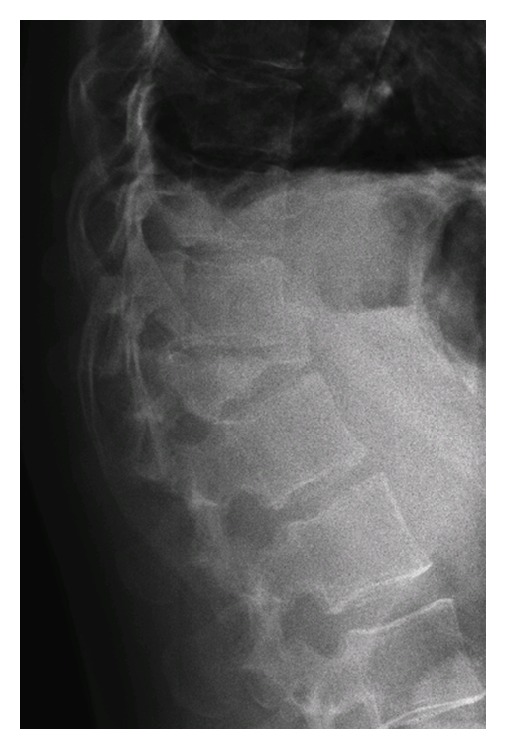
Lumbosacral X-ray:
The lumbosacral area is shown in an anteroposterior X-ray (A) and a lateral X-ray (B).
These images demonstrate normal sacroiliac joints, appropriate spinal alignment, and no height loss of the intervertebral disk space.
A CT scan can evaluate both bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types and soft tissue Soft Tissue Soft Tissue Abscess structures.
Anatomy:
Different planes can be used:
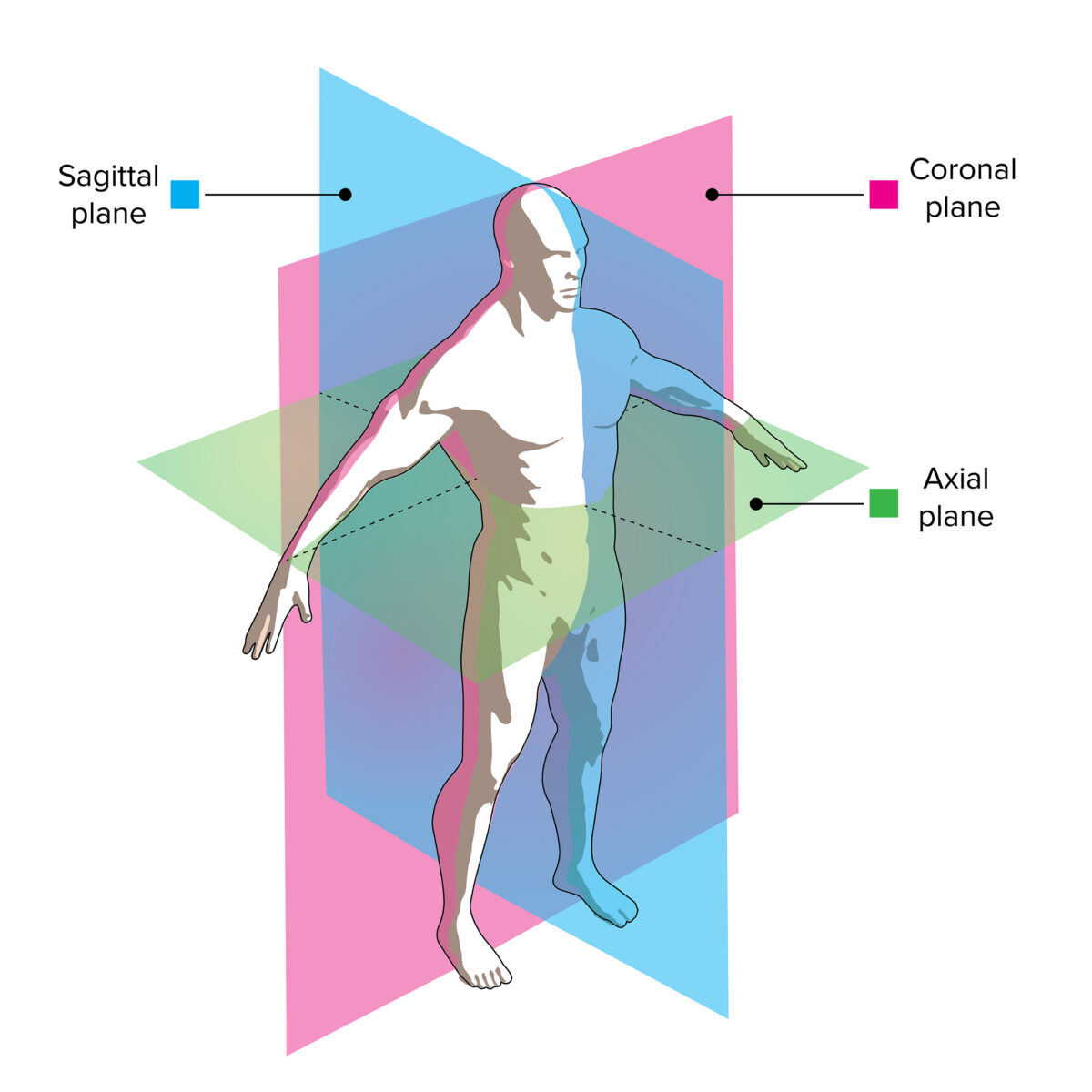
CT image viewing planes:
The slices through this model demonstrate how axial, coronal, and sagittal images correlate with the patient’s anatomy.
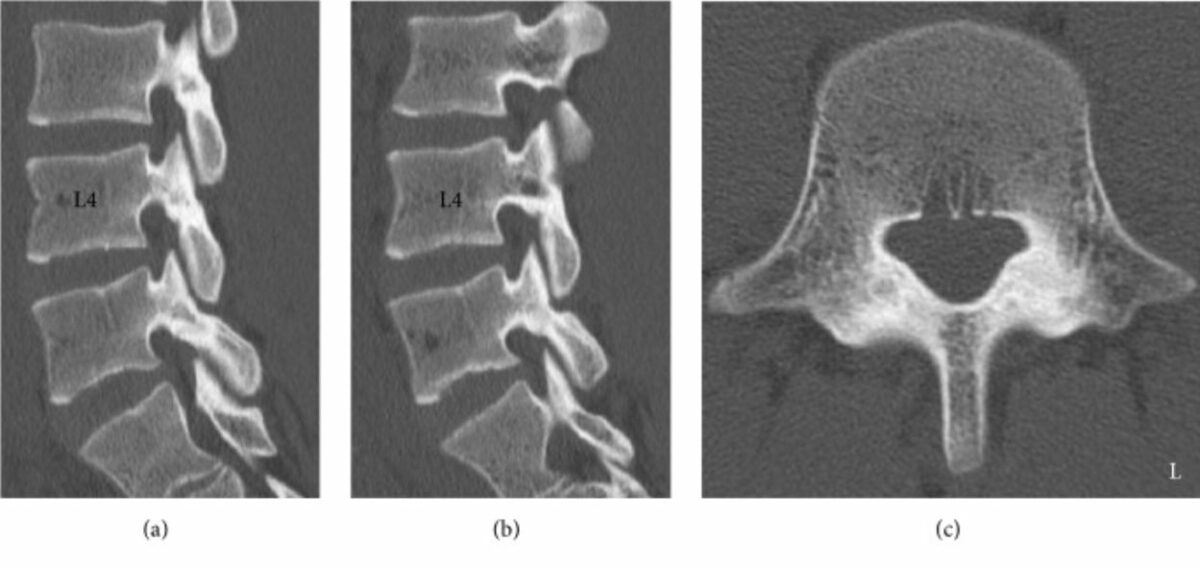
Spinal CT views:
Right (a) and left (b) parasagittal reconstructed CT image of the lumbar spine
(c): Axial CT image at L5 level, which shows a displaced fracture of the left/inferior vertebral body of C5.

Coronal view of the spine
Image: “Figure 1” by Clemente, M.A., et al. License: CC BY 4.0, cropped by Lecturio.MRI provides superior visualization of intraspinal anatomy.
Anatomy:
On T2-weighted images T2-Weighted Images Imaging of the Head and Brain:
Different planes can be used:
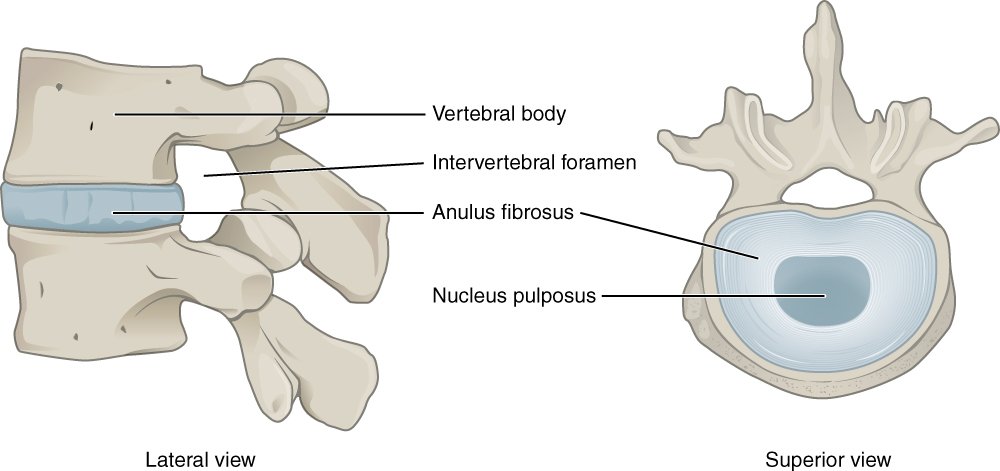
Intervertebral disk
Image: “Intervertebral disc” by Phil Schatz. License: CC BY 4.0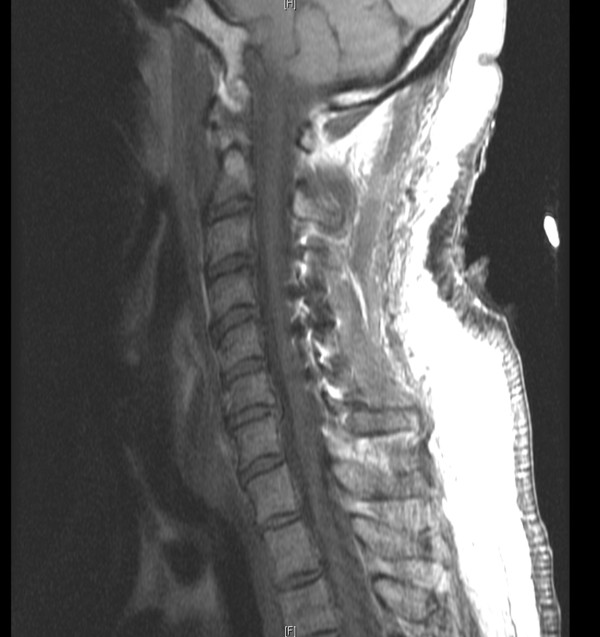
Sagittal T1-weighted MRI of the cervical spine
Image: “Possible gabapentin and ketamine interaction causing prolonged central nervous system depression during post-operative recovery following cervical laminoplasty: a case report” by Elyassi AR, Long RP, Bejnarowicz RP, Schoneboom BA. License: CC BY 2.0
Coronal T2-weighted MRI of the cervical spine shows defective ossification of vertebral bodies.
Image: “Significant traumatic atrophy of the spinal cord in connection with severe cervical vertebral body hypoplasia in a boy with Larsen syndrome: a case report and review of the literature” by Al Kaissi A, Altenhuber J, Grill F, Klaushofer K. License: CC BY 3.0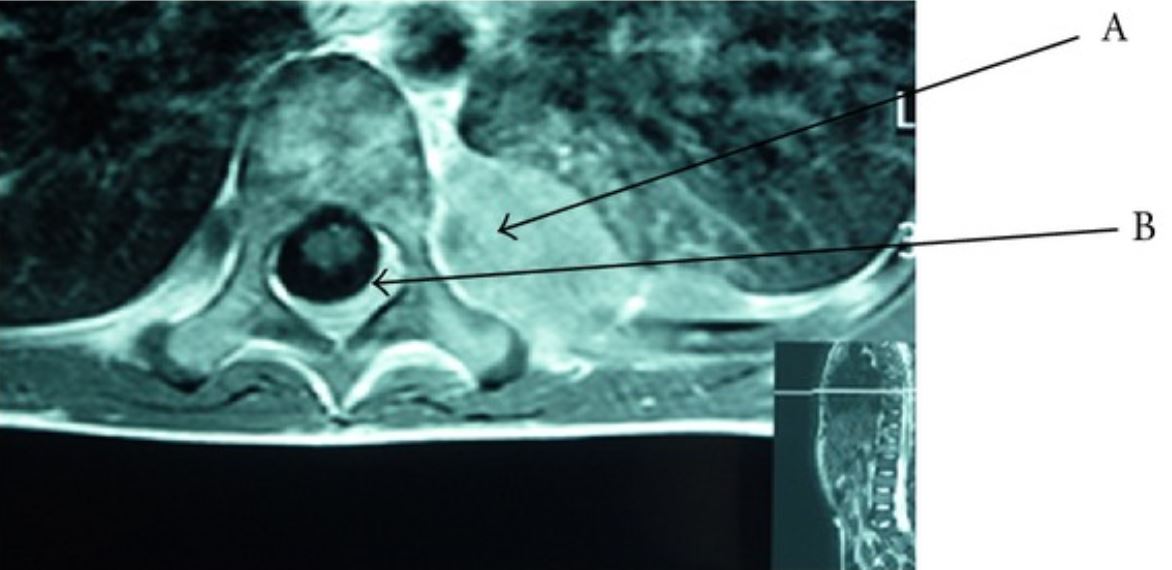
Axial T1-weighted MRI:
In this image, A points to a dorsal paravertebral mass and B points to tumor spread.
| Tissue | T1-weighted images T1-Weighted Images Imaging of the Head and Brain | T2-weighted images T2-Weighted Images Imaging of the Head and Brain |
|---|---|---|
| Fluid (e.g., CSF) | Dark | Bright |
| White matter White Matter The region of central nervous system that appears lighter in color than the other type, gray matter. It mainly consists of myelinated nerve fibers and contains few neuronal cell bodies or dendrites. Brown-Séquard Syndrome | Light gray | Dark gray |
| Gray matter Gray matter Region of central nervous system that appears darker in color than the other type, white matter. It is composed of neuronal cell bodies; neuropil; glial cells and capillaries but few myelinated nerve fibers. Cerebral Cortex: Anatomy | Gray | Light gray |
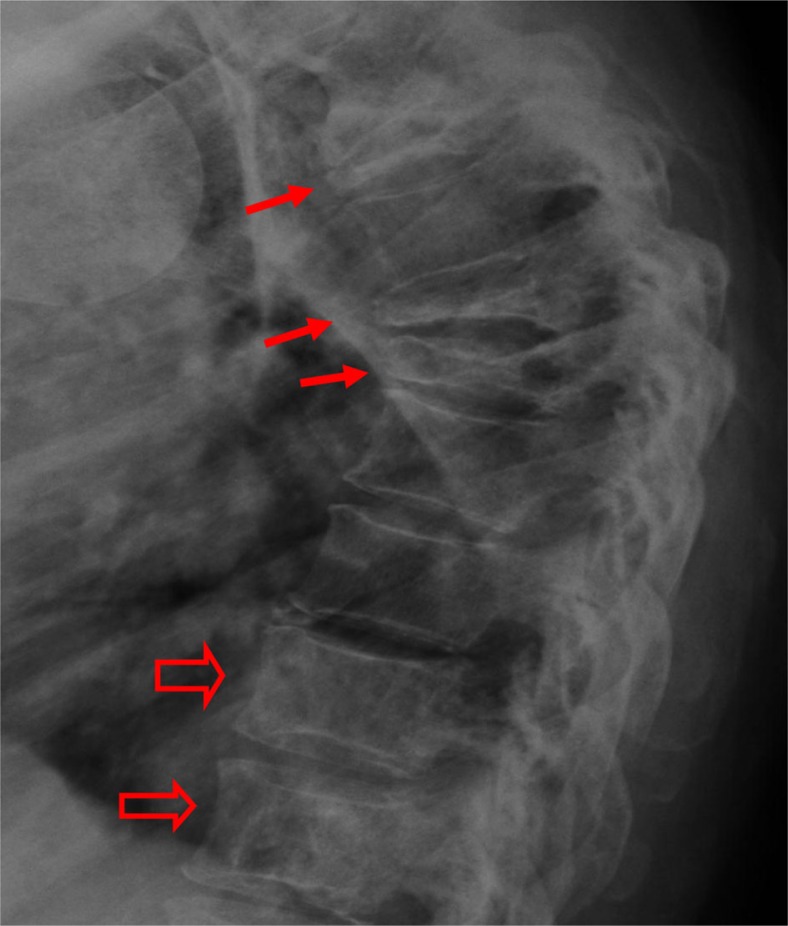
Compression fractures:
A lateral thoracic spine radiograph shows multiple severe vertebral body compression fractures (vertebra plana; small arrows) characteristic of multiple myeloma (among other etiologies). At T11 and T12 (open arrows), mild vertebral sclerosis is a result of treatment and healing.
X-ray of burst fracture of T12
Image: “Figure 1” by Akiki Alian. License: Public Domain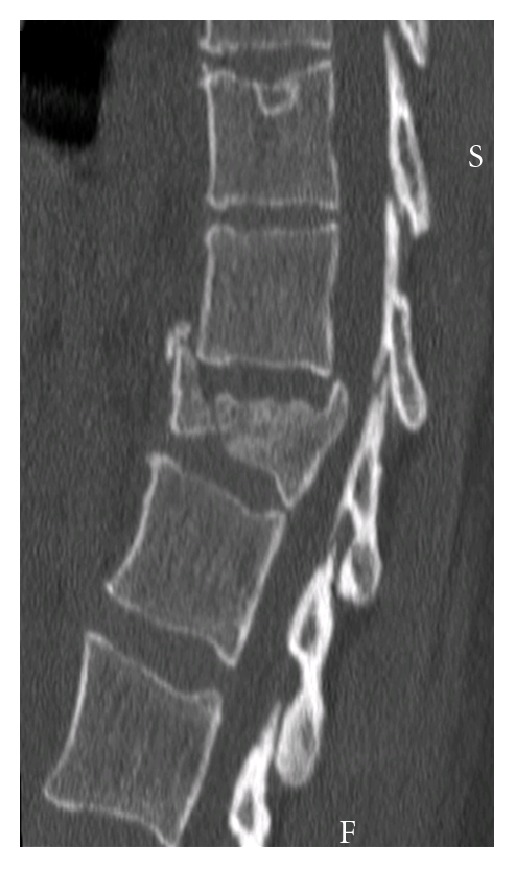
Sagittal CT of burst fracture of T12
Image: “Figure 1” by Akiki Alian. License: Public Domain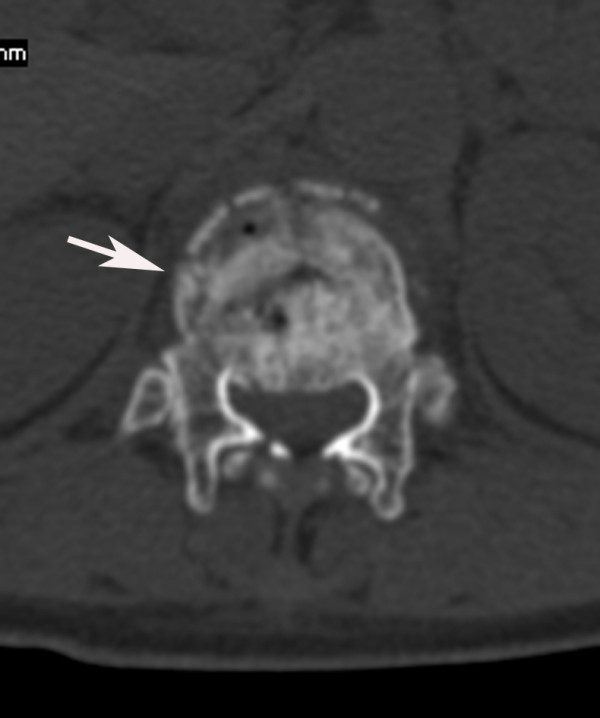
Burst fracture on CT:
Cross-sectional image shows burst fracture of T12 (arrow) and spinal canal narrowing.
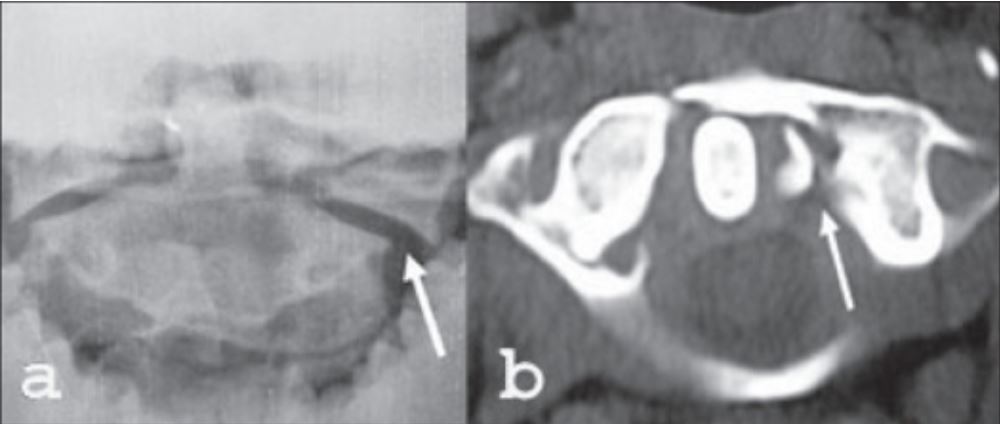
Jefferson fracture:
a: Open-mouth X-ray shows lateral subluxation of C1–C2 (arrow).
b: Axial CT scan with fracture on the left side (arrow)
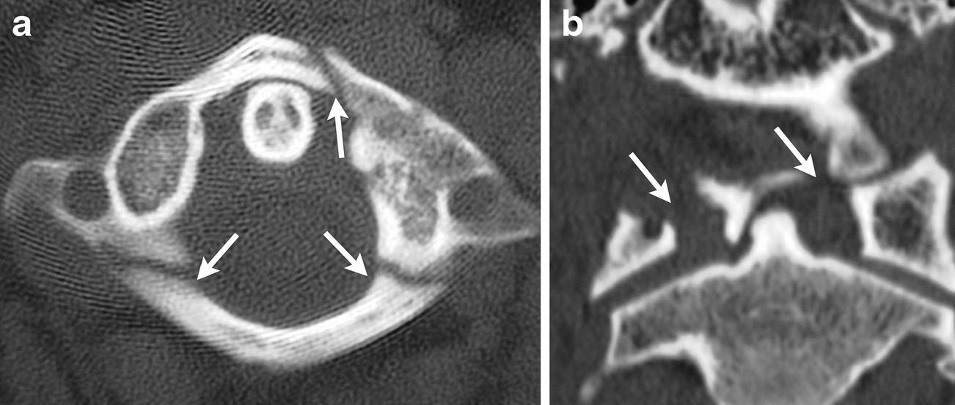
Jefferson fracture on CT:
Multiple fractures involving the anterior and posterior arches of C1 are seen on axial (a) and coronal (b) CT scans.

Radiography shows dens fracture on C2 (type III Hangman’s fracture):
There is also significant anterior subluxation of C2 on the C3 vertebral body.
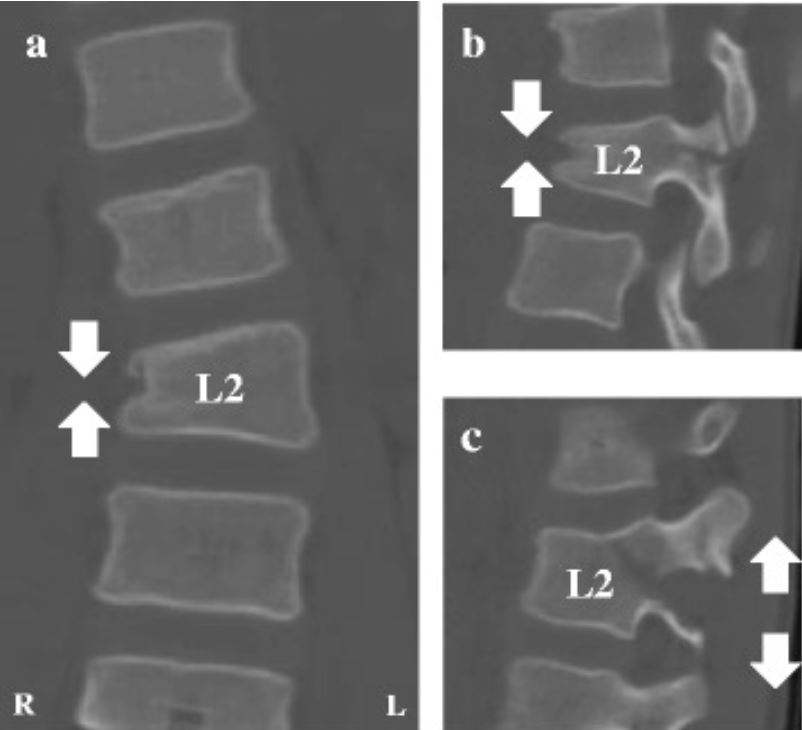
Chance fracture on CT (images at the time of injury):
Images reveal a Chance-type injury with an associated L2 compression fracture of the right vertebral body (a), a horizontal split of the right L2 pedicle (b), and the splitting and distraction of the left L2 transverse processes, left L2 pedicle, and L2 middle column (c), resulting in asymmetrical kyphoscoliosis.

Spondylolisthesis of L5 on S1 on radiography:
Lateral X-ray showing disruption of the center line and anterior displacement of the lumbar spine over sacral vertebrae

Spondylolysis on X-ray:
A break in the pars interarticularis (arrow) with associated anterior spondylolisthesis
Image: “Image-guided lumbar facet joint infiltration in nonradicular low back pain” by Chaturvedi A, Chaturvedi S, Sivasankar R. License: CC BY 2.0, cropped by Lecturio.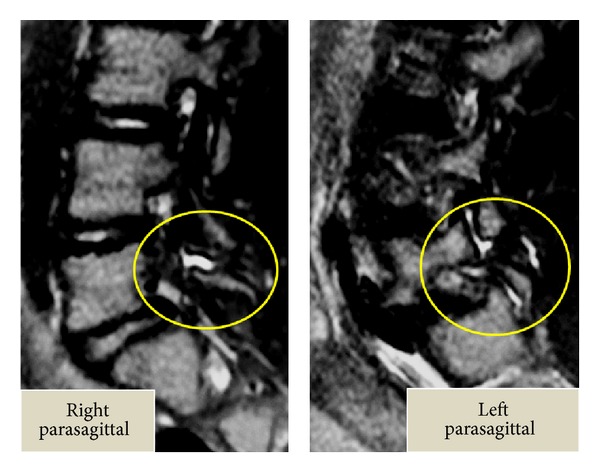
Lumbar spondylolysis in MRI:
Note the effusion within the pars defects and within the adjacent facet joints.

Disk herniation on MRI:
T2-weighted MRI showing L5–S1 disk herniation into the spinal canal and degenerative disk changes (loss of T2 signal intensity and loss of disk-space height)
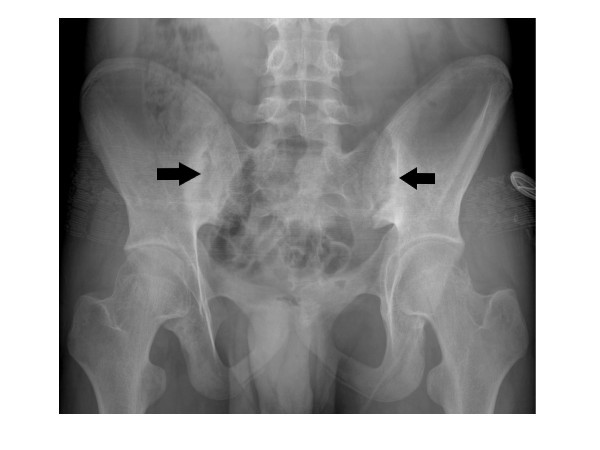
Bilateral sacroiliitis on radiography (arrows):
There is subchondral sclerosis of the iliac bone, joint surface irregularities, which include some erosions on both sides, and joint space narrowing of the hips.
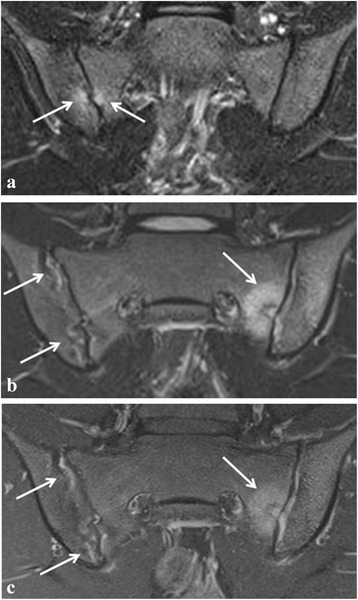
Sacroiliitis on MRI:
a: Arrows point to focal spots of bone marrow edema (BME) on the right sacroiliac (SI) joint
b: Arrows show active sacroiliitis with bilateral high signal in the joint space and BME on the sacral side of the SI joint
c: Fat-saturated T1-weighted image showing bilateral synovitis and active lesion on the left side (arrows)

Metastasis seen as an osteolytic lesion on X-ray:
Thoracic spine X-ray in a patient with hepatocellular carcinoma showing osteolytic left L1 lesion with missing pedicle (blue line)

Metastatic disease (affecting the spine) on MRI:
MRI sagittal T1-weighted image reveals scattered foci of decreased signal intensity reflective of metastatic disease affecting the cervical and thoracic spine regions.
MRI is the study of choice for spinal tumors.

Meningioma on MRI:
A and B: The T1- and T2-weighted images both show slightly lower intensity than that of the cord, revealing a homogeneous lesion.
C: Contrast-enhanced MRI shows the high homogeneous signal intensity of the tumor.
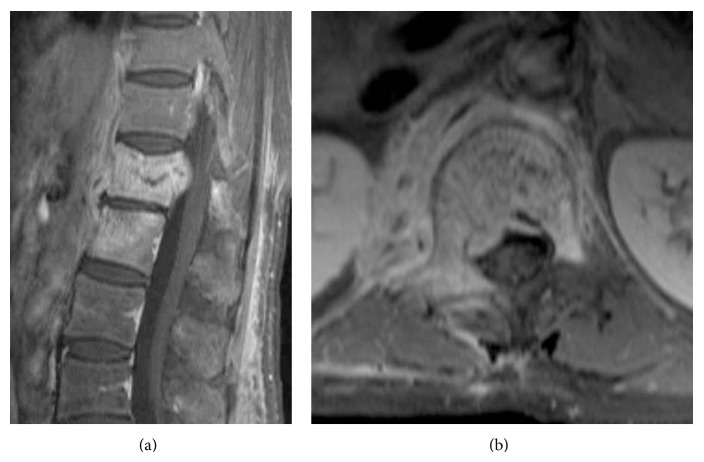
Vertebral osteomyelitis on MRI:
Enhanced T1-weighted MRI showing vertebral osteomyelitis involving the L1 and L2 vertebral bodies. Of note, the relative sparing of the intervertebral disk space can typically be seen with mycobacterial infection.
(a): Sagittal view
(b): Axial view
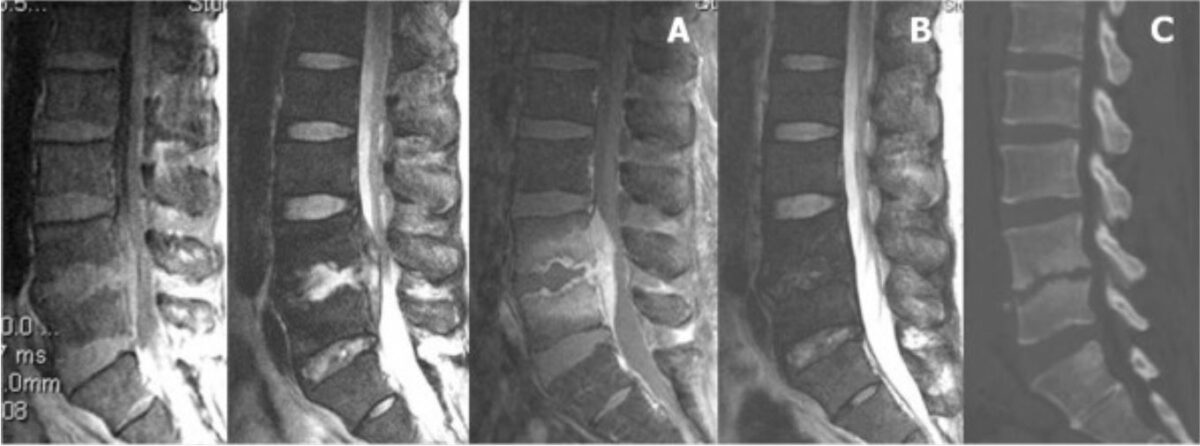
Epidural abscess on MRI: L4–5 infectious spondylitis in a male patient:
A: Sagittal T1- and T2-weighted and contrast MRI shows L4–5 epidural abscess with compression of neural elements.
B: After treatment, sagittal T2-weighted MRI at 6-month follow-up demonstrates the disappearance of the abscess.
C: Sagittal CT reveals L4–5 disk space narrowing leading to spontaneous fusion.

MRI of spinal cord injury:
Spinal cord transection at the T6 injury level (arrow) noted in a patient who had a fall from 300 feet.
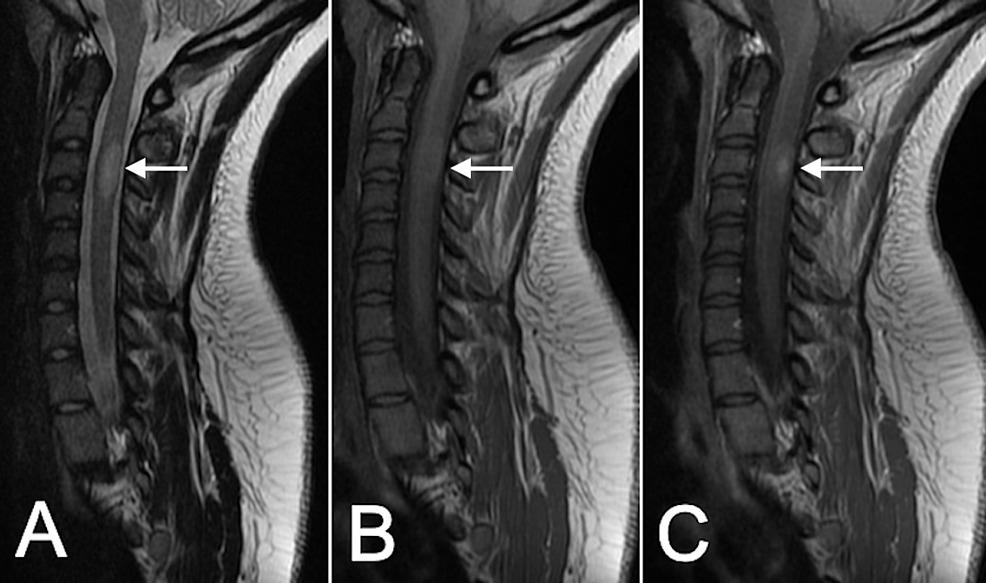
Tumefactive multiple sclerosis on MRI:
C3 cervical intramedullary lesion (arrow) that is hyperintense on T2-weighted images (A), is isointense on T1-weighted images (B), and has areas of contrast enhancement (C).