Schwannomas (also known as neurilemmomas) are benign Benign Fibroadenoma nerve sheath tumors in the peripheral nervous system Peripheral nervous system The nervous system outside of the brain and spinal cord. The peripheral nervous system has autonomic and somatic divisions. The autonomic nervous system includes the enteric, parasympathetic, and sympathetic subdivisions. The somatic nervous system includes the cranial and spinal nerves and their ganglia and the peripheral sensory receptors. Nervous System: Anatomy, Structure, and Classification (PNS), arising from Schwann cells that encase the peripheral nerves Peripheral Nerves The nerves outside of the brain and spinal cord, including the autonomic, cranial, and spinal nerves. Peripheral nerves contain non-neuronal cells and connective tissue as well as axons. The connective tissue layers include, from the outside to the inside, the epineurium, the perineurium, and the endoneurium. Nervous System: Histology. Schwannomas are the most common tumors in the PNS. Although schwannomas are typically sporadic Sporadic Selective IgA Deficiency, they can be associated with neurofibromatosis type II and schwannomatosis. The clinical presentation of schwannomas depends on their specific location, but general signs and symptoms include a palpable mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast on the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, and/or paresthesias Paresthesias Subjective cutaneous sensations (e.g., cold, warmth, tingling, pressure, etc.) that are experienced spontaneously in the absence of stimulation. Posterior Cord Syndrome due to nerve compression Nerve Compression Brachial Plexus Injuries. The diagnosis is established primarily based on imaging studies (MRI or CT), and the treatment is usually surgical resection.
Last updated: May 29, 2025
Schwannomas are benign Benign Fibroadenoma, encapsulated Encapsulated Klebsiella nerve sheath tumors in the peripheral nervous system Peripheral nervous system The nervous system outside of the brain and spinal cord. The peripheral nervous system has autonomic and somatic divisions. The autonomic nervous system includes the enteric, parasympathetic, and sympathetic subdivisions. The somatic nervous system includes the cranial and spinal nerves and their ganglia and the peripheral sensory receptors. Nervous System: Anatomy, Structure, and Classification (PNS), arising from Schwann cells.
| Categories | Specific tumors |
|---|---|
| Neuroepithelial tumors in the CNS |
|
| Meningeal tumors |
|
| Sellar region tumors |
|
| Primary CNS lymphoma Lymphoma A general term for various neoplastic diseases of the lymphoid tissue. Imaging of the Mediastinum | Primary CNS lymphoma Lymphoma A general term for various neoplastic diseases of the lymphoid tissue. Imaging of the Mediastinum |
| Metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis to the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification (5x more common than primary brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification tumors) | Most commonly arising from: |
| Peripheral tumors |
|
Schwannomas can be classified into 1 of 4 primary types based on histology.
| Type of schwannoma | Key points |
|---|---|
| Classic schwannoma |
|
| Cellular schwannoma |
|
| Plexiform schwannoma |
|
| Melanotic schwannoma |
|
Aside from acoustic neuromas (which arise from the 8th cranial nerve), schwannomas may form in a variety of locations throughout the body:
When symptoms do occur, they may include:
Following a suggestive history and exam, the diagnosis is primarily established via imaging and can be confirmed on biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma.
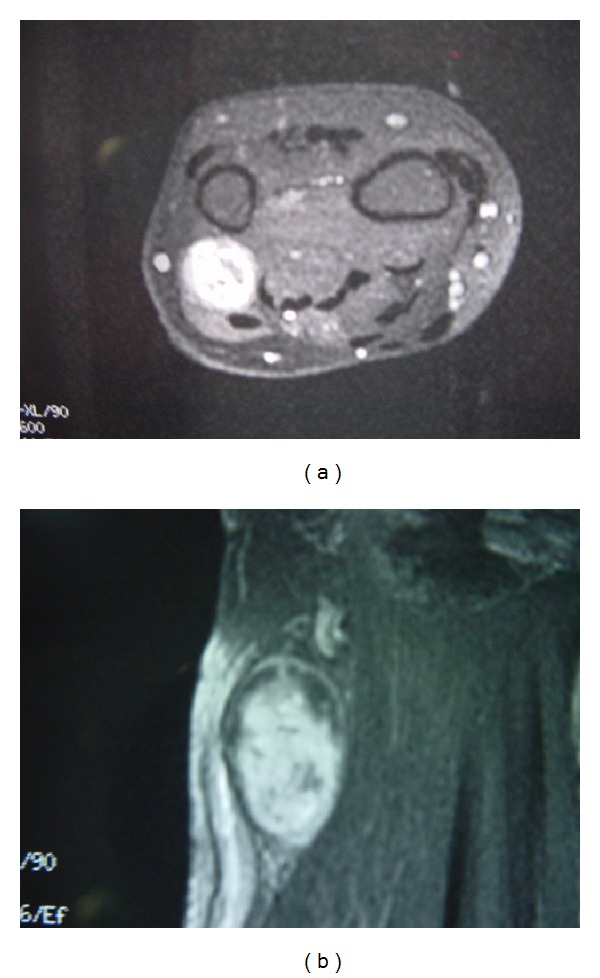
MRI showing schwannoma involving dorsal cutaneous branch of ulnar nerve
Image: “Schwannoma in the upper limbs” by Tang CY, Fung B, Fok M, Zhu J. License: CC BY 3.0Classic schwannomas:
Distinctive features of other types:
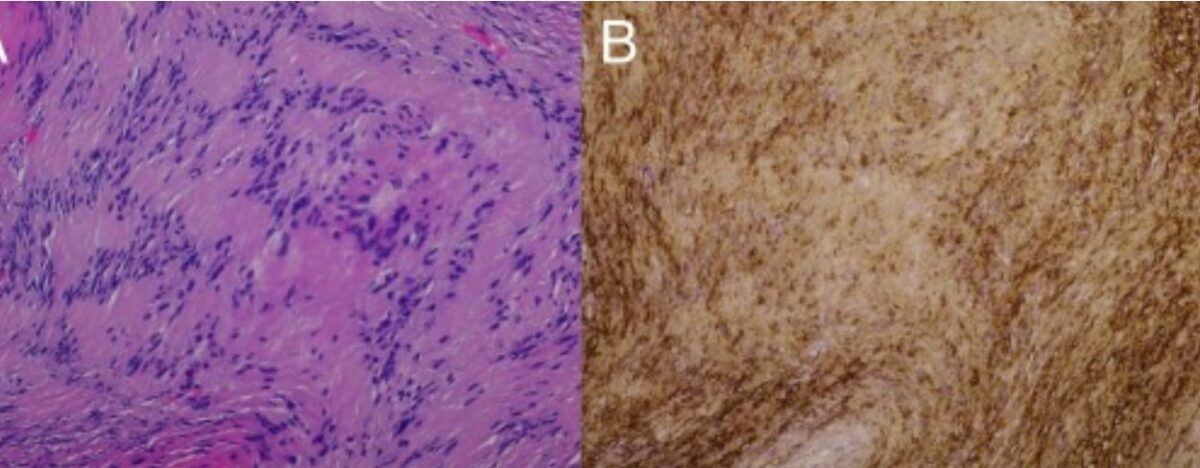
Pathology slides demonstrating schwannoma:
A: H&E slide at 20x showing the classic biphasic pattern (Antoni A and Antoni B) of schwannoma.
B: positive S100 stain
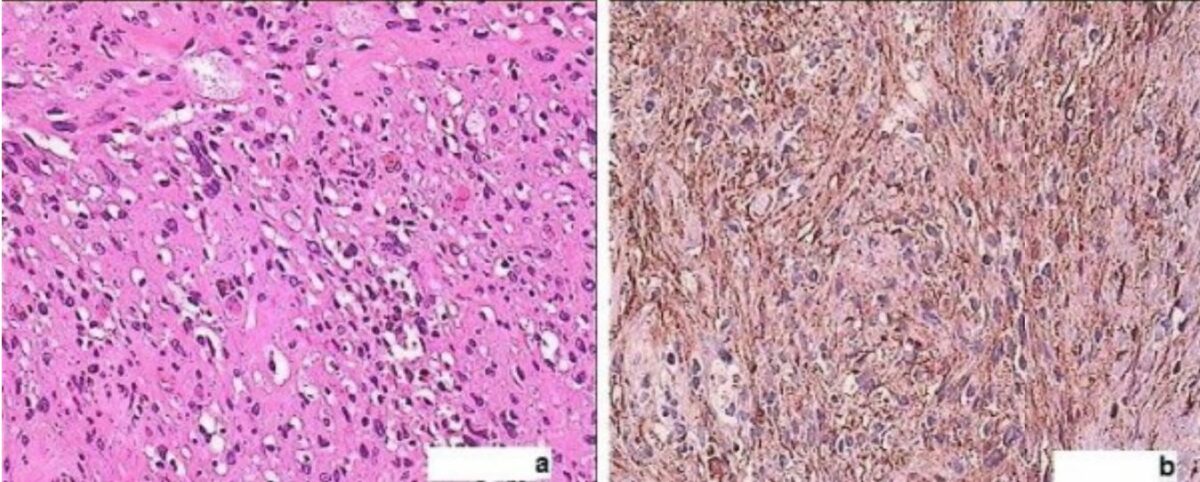
a: H&E-stained sections (40x) reveal an ancient schwannoma demonstrating a circumscribed spindle-cell tumor, cellular atypia but no mitotic activity, myxoid degeneration, and vessels with hyalinized walls.
b: strongly positive S100 immunohistochemistry in ancient schwannoma
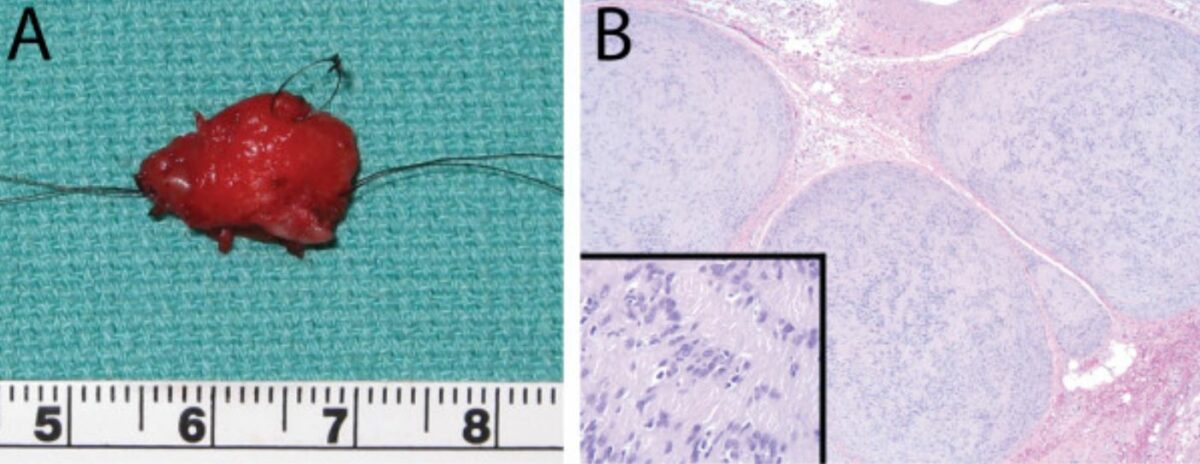
Plexiform cellular schwannoma:
A: gross pathology of excised mass measuring 15 mm by 12 mm
B: histopathology (H&E) revealing schwannoma; original magnification 50x and 200x (inset)
Schwannomas are commonly classified according to the Enneking system of benign Benign Fibroadenoma lesions. There are 3 grades, and most schwannomas are grade II or III lesions.
For patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with functional deficits and/or pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways due to nerve compression Nerve Compression Brachial Plexus Injuries, treatment is recommended.