Organ dysfunction resulting from a dysregulated systemic host response to infection separates sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock from uncomplicated infection. The etiology is mainly bacterial and pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia is the most common known source. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship commonly present with fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, tachypnea Tachypnea Increased respiratory rate. Pulmonary Examination, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, and/or altered mentation. Septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock is diagnosed during treatment when vasopressors Vasopressors Sepsis in Children are necessary to control hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension. Sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock and septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock are medical emergencies, and antibiotics are given within an hour of diagnosis.
Last updated: Mar 21, 2024
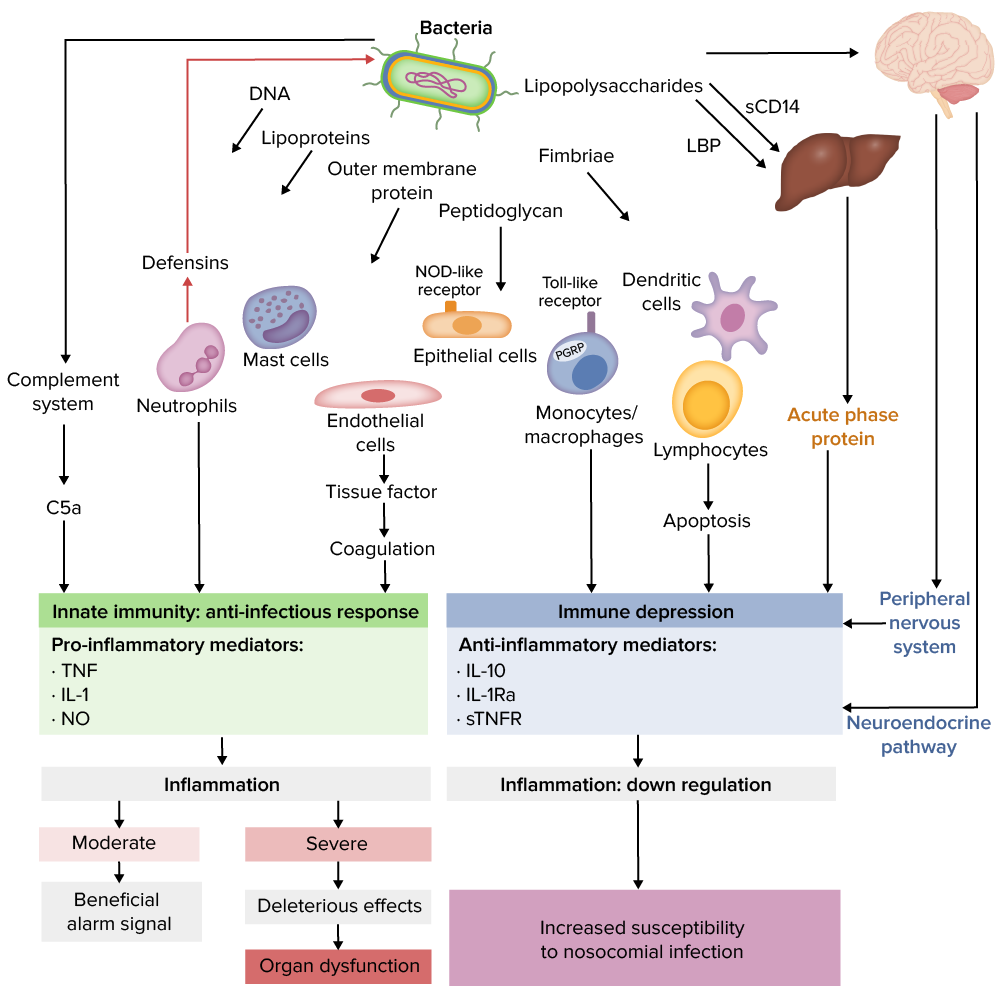
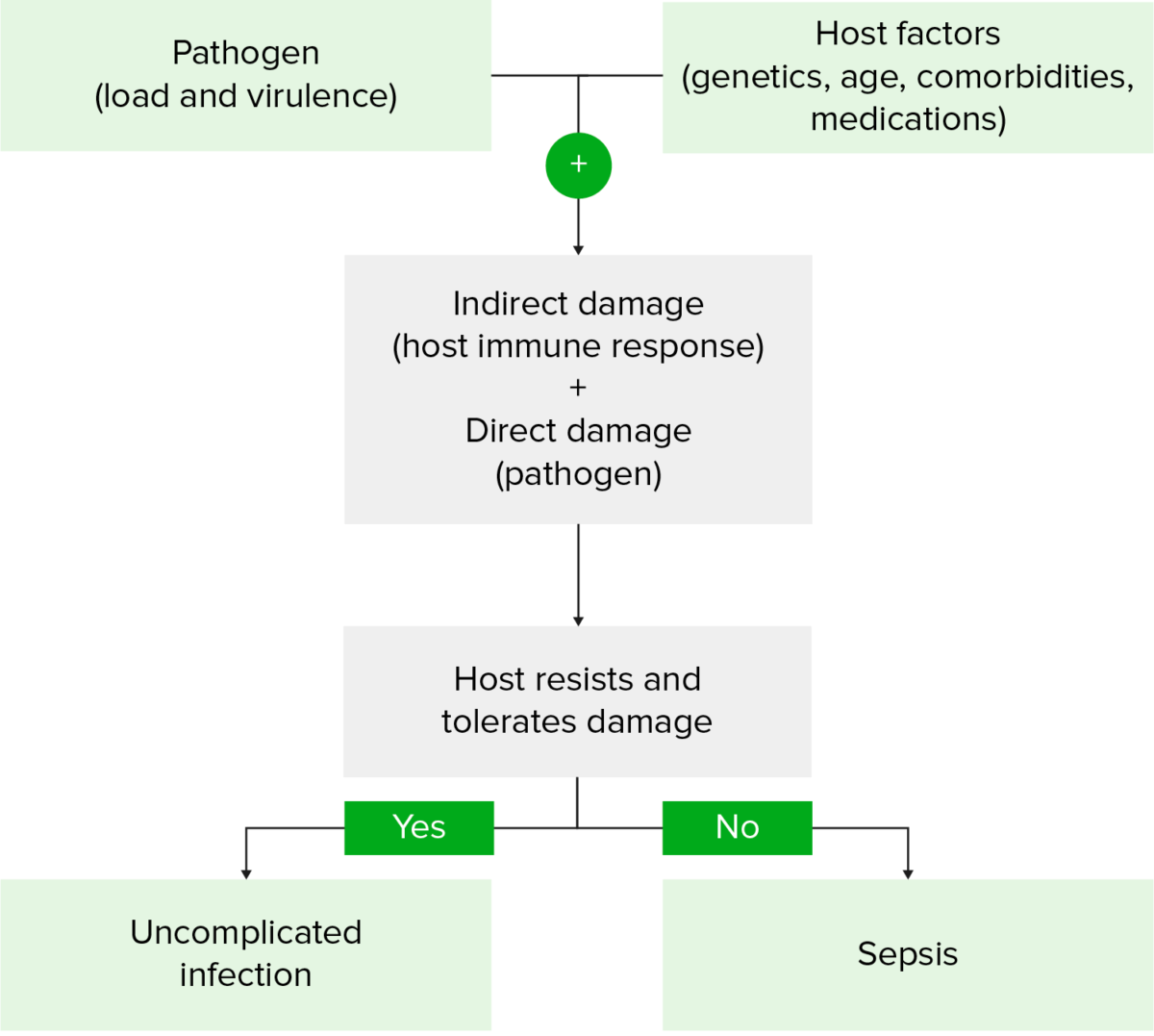
Pathogen load and virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus + host genetic composition and comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus result in a complex, exaggerated, and prolonged host response to infection that evolves over time.
Pathophysiology of septic shock
sTNFR: soluble tumor necrosis factor receptor
LBP: Lipopolysaccharide binding protein
Pathogenesis of sepsis
Image by Lecturio.Criteria for sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock:[9]
Criteria for septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock:[9]
SOFA SOFA Sepsis and Septic Shock score:[6,9]
| Organ/system | SOFA SOFA Sepsis and Septic Shock score | Indication |
|---|---|---|
| Respiratory system: PaO2/FiO2 (mm Hg) | 0 | ≥ 400 |
| + 1 | 300–399 | |
| + 2 | 200–299 | |
| + 3 | 100–199 + mechanically ventilated | |
| + 4 | < 100 + mechanically ventilated | |
| Nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification: Glasgow coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma scale Scale Dermatologic Examination | 0 | 15 |
| + 1 | 13–14 | |
| + 2 | 10–12 | |
| +3 | 6–9 | |
| + 4 | < 6 | |
| Cardiovascular system: MAP OR need for vasopressors Vasopressors Sepsis in Children | 0 | MAP ≥ 70 mm Hg |
| + 1 | MAP < 70 mm Hg | |
| + 2 | Dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS ≤ 5 μg/kg/min or dobutamine Dobutamine A catecholamine derivative with specificity for beta-1 adrenergic receptors. Sympathomimetic Drugs (any dose) | |
| + 3 | Dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS > 5 μg/kg/min OR epinephrine Epinephrine The active sympathomimetic hormone from the adrenal medulla. It stimulates both the alpha- and beta- adrenergic systems, causes systemic vasoconstriction and gastrointestinal relaxation, stimulates the heart, and dilates bronchi and cerebral vessels. Sympathomimetic Drugs ≤ 0.1 μg/kg/min OR norepinephrine Norepinephrine Precursor of epinephrine that is secreted by the adrenal medulla and is a widespread central and autonomic neurotransmitter. Norepinephrine is the principal transmitter of most postganglionic sympathetic fibers, and of the diffuse projection system in the brain that arises from the locus ceruleus. Receptors and Neurotransmitters of the CNS ≤ 0.1 μg/kg/min | |
| + 4 | Dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS > 15 μg/kg/min OR epinephrine Epinephrine The active sympathomimetic hormone from the adrenal medulla. It stimulates both the alpha- and beta- adrenergic systems, causes systemic vasoconstriction and gastrointestinal relaxation, stimulates the heart, and dilates bronchi and cerebral vessels. Sympathomimetic Drugs > 0.1 μg/kg/min OR norepinephrine Norepinephrine Precursor of epinephrine that is secreted by the adrenal medulla and is a widespread central and autonomic neurotransmitter. Norepinephrine is the principal transmitter of most postganglionic sympathetic fibers, and of the diffuse projection system in the brain that arises from the locus ceruleus. Receptors and Neurotransmitters of the CNS > 0.1 μg/kg/min | |
| Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy: bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism (mg/dL) | 0 | < 1.2 |
| + 1 | 1.2–1.9 | |
| + 2 | 2–5.9 | |
| + 3 | 6–11.9 | |
| + 4 | ≥ 12 | |
| Coagulation: platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology × 1000/μL | 0 | ≥ 150 |
| + 1 | 100–149 | |
| + 2 | 50–99 | |
| + 3 | 20–49 | |
| + 4 | < 20 | |
| Kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy: creatinine (mg/dL) or urine output | 0 | < 1.2 |
| + 1 | 1.2–1.9 | |
| + 2 | 2–3.4 | |
| + 3 | 3.4–4.9 or < 500 mL/day | |
| + 4 | > 5.0 or < 200 mL/day |
National Early Warning Score (NEWS):[6,8]
| Clinical parameter | Result | Score |
|---|---|---|
| Respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination | ≤ 8 breaths/minute | 3 |
| 9–11 breaths/minute | 1 | |
| 12–20 breaths/minute | 0 | |
| 21–24 breaths/minute | 2 | |
| ≥ 25 breaths/minute | 3 | |
| Oxygen saturations | ≤ 91% | 3 |
| 92%–93% | 2 | |
| 94%–95% | 1 | |
| ≥ 96% | 0 | |
| Use of supplemental oxygen Supplemental Oxygen Respiratory Failure | No | 0 |
| Yes | 2 | |
| Temperature | ≤ 35℃ | 3 |
| 35.1–36℃ | 1 | |
| 36.1–38℃ | 0 | |
| 38.1–39℃ | 1 | |
| ≥ 39℃ | 2 | |
|
Systolic blood pressure
|
≤ 90 mm Hg | 3 |
| 91–100 mm Hg | 2 | |
| 101–110 mm Hg | 1 | |
| 111–219 mm Hgg | 0 | |
| ≥ 220 mm H | 3 | |
| Heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology | ≤ 40/min | 3 |
| 41–50/min | 1 | |
| 51–90 bpm | 0 | |
| 91–110/min | 1 | |
| 111–130/min | 2 | |
| ≥ 131/min | 3 | |
| AVPU score | Alert | 0 |
| Voice | 3 | |
| Pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 3 | |
| Unresponsive | 3 |
The following are often ordered in the evaluation of sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock and septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock. Workup should be guided by the clinical presentation.
Sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock and septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock are medical emergencies and treatment should begin immediately!
Ideally, the following steps should begin within the 1st hour after the diagnosis of sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock.
| Patient’s immune status | Choice of antibiotic |
|---|---|
| Immunocompetent | Any of the following:
Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides (or linezolid Linezolid An oxazolidinone and acetamide derived anti-bacterial agent and protein synthesis inhibitor that is used in the treatment of gram-positive bacterial infections of the skin and respiratory tract. Oxazolidinones) if risk of MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus is high or if in septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock |
| Neutropenic (< 500 neutrophils Neutrophils Granular leukocytes having a nucleus with three to five lobes connected by slender threads of chromatin, and cytoplasm containing fine inconspicuous granules and stainable by neutral dyes. Innate Immunity: Phagocytes and Antigen Presentation/μL) | Any of the following:
Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides (or linezolid Linezolid An oxazolidinone and acetamide derived anti-bacterial agent and protein synthesis inhibitor that is used in the treatment of gram-positive bacterial infections of the skin and respiratory tract. Oxazolidinones), tobramycin, and caspofungin Caspofungin A cyclic lipopeptide echinocandin and beta-(1, 3)-d-glucan synthase inhibitor that is used to treat internal or systemic mycoses. Echinocandins |
| Splenectomy Splenectomy Surgical procedure involving either partial or entire removal of the spleen. Rupture of the Spleen | Any of the following:
Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides (or linezolid Linezolid An oxazolidinone and acetamide derived anti-bacterial agent and protein synthesis inhibitor that is used in the treatment of gram-positive bacterial infections of the skin and respiratory tract. Oxazolidinones) |
| Associated with pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia | Refer to the treatment of community- and ventilator-acquired pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia. |
| Associated with severe intra-abdominal infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease | Any of the following:
Metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess |