Cellulitis is a common infection caused by bacteria that affects the dermis and subcutaneous tissue of the skin. It is frequently caused by Staphylococcus aureus and Streptococcus pyogenes. The skin infection presents as an erythematous and edematous area with warmth and tenderness. The borders are not clearly delineated. The lower extremities are the most frequent site of infection, but cellulitis can occur anywhere on the body. Diagnosis is usually clinical, and management involves oral and/or parenteral antibiotics. Coverage for MRSA may be added, depending on the presence of risk factors.
Last updated: Mar 4, 2024
Cellulitis Cellulitis Cellulitis is a common infection caused by bacteria that affects the dermis and subcutaneous tissue of the skin. It is frequently caused by Staphylococcus aureus and Streptococcus pyogenes. The skin infection presents as an erythematous and edematous area with warmth and tenderness. Cellulitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and subcutaneous tissues. It is often due to infection.

Left lower extremity cellulitis:
Edema and erythema of the skin are noted in the left leg and foot.

Abdominal wall cellulitis:
Image shows marked pitting edema and erythema with poorly demarcated borders due to cellulitis.
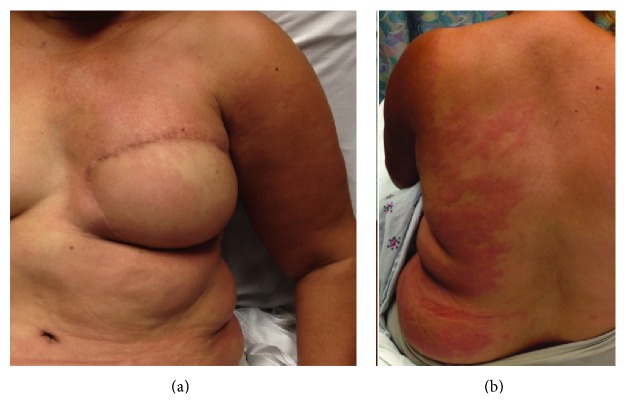
Lymphedema cellulitis:
Stagnant lymph is an ideal medium for bacterial growth, and progression can be rapid owing to a decreased ability to fight infection in the affected area. Infections are commonly caused by gram-positive cocci bacteria.
Antibiotic protocols may vary based on the microbiologic susceptibility of the population of the practice location. The following recommendations are based on US and UK guidelines.
General principles:[6–8]
No MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus risk factors (Table 1):
With MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus risk factors (Table 2):
Other considerations:
| Medication | Pediatric dose | Adult dose | |
|---|---|---|---|
| Oral therapy: no penicillin Penicillin Rheumatic Fever allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction | Flucloxacillin (not available in the US)[7] | 500 mg‒1 g 4 times/day | |
| Dicloxacillin Dicloxacillin One of the penicillins which is resistant to penicillinase. Penicillins[2,6–8] | 25–50 mg/kg/day in 4 divided doses; maximum, 500 mg/dose | 250 mg‒500 mg 4 times/day; maximum, 2 g/day | |
| Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins–clavulanate[1–4,6] | 25 mg/kg/day in 2 divided doses | 875 mg 2 times/day | |
| Cephalexin[6–8] | 25‒50 mg/kg/day in 4 divided doses | 500 mg 4 times/day | |
| Oral therapy: penicillin Penicillin Rheumatic Fever allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction | Clindamycin Clindamycin An antibacterial agent that is a semisynthetic analog of lincomycin. Lincosamides[6-8] | 25–30 mg/kg/day in 3 divided doses | 300‒450 mg 4 times/day |
| Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolidesa[7] | 500 mg 2 times/day | ||
| Erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolidesa[7] | > 8 years old: 250–500 mg 4 times/day | 500 mg 4 times/day | |
| Doxycyclinea[6–8] | |||
| Parenteral therapy: no penicillin Penicillin Rheumatic Fever allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction | Flucloxacillin (not available in the US)[7,8] | 1 month–17 years: 12.5‒25 mg/kg 4 times/day; maximum, 4 g/day | 1‒2 g every 6 hours |
| Nafcillin Nafcillin A semi-synthetic antibiotic related to penicillin. Staphylococcal Scalded Skin Syndrome (SSSS) or oxacillin[6] | 100‒150 mg/kg/day in 4 divided doses | 1‒2 g every 4 hours | |
| Cefazolin Cefazolin A semisynthetic cephalosporin analog with broad-spectrum antibiotic action due to inhibition of bacterial cell wall synthesis. It attains high serum levels and is excreted quickly via the urine. Cephalosporinsb[6] | 50 mg/kg/day in 3 divided doses | 1 g every 8 hours | |
| Parenteral therapy (given for 7 days): penicillin Penicillin Rheumatic Fever allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction | Clindamycin Clindamycin An antibacterial agent that is a semisynthetic analog of lincomycin. Lincosamides[6–8] | 25–40 mg/kg/day in 3 divided doses | 600 mg every 8 hours |
| Medication | Pediatric dose | Adult dose | |
|---|---|---|---|
| Oral therapy | Trimethoprim Trimethoprim The sulfonamides are a class of antimicrobial drugs inhibiting folic acid synthesize in pathogens. The prototypical drug in the class is sulfamethoxazole. Although not technically sulfonamides, trimethoprim, dapsone, and pyrimethamine are also important antimicrobial agents inhibiting folic acid synthesis. The agents are often combined with sulfonamides, resulting in a synergistic effect. Sulfonamides and Trimethoprim– sulfamethoxazole Sulfamethoxazole A bacteriostatic antibacterial agent that interferes with folic acid synthesis in susceptible bacteria. Its broad spectrum of activity has been limited by the development of resistance. Sulfonamides and Trimethoprim[6] | 8–12 mg/kg/day in 2 divided doses (based on trimethoprim Trimethoprim The sulfonamides are a class of antimicrobial drugs inhibiting folic acid synthesize in pathogens. The prototypical drug in the class is sulfamethoxazole. Although not technically sulfonamides, trimethoprim, dapsone, and pyrimethamine are also important antimicrobial agents inhibiting folic acid synthesis. The agents are often combined with sulfonamides, resulting in a synergistic effect. Sulfonamides and Trimethoprim component) | 1–2 double-strength tablets 2 times daily |
| Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins plus doxycycline[[7,8] | See individual dosing in Table 1. | See individual dosing in Table 1. | |
| Clindamycin Clindamycin An antibacterial agent that is a semisynthetic analog of lincomycin. Lincosamides[6-8] | See individual dosing in Table 1. | See individual dosing in Table 1. | |
| Parenteral therapy | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides[6–8] | 10–15 mg/kg 4 times a day, adjusted to vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides concentration | 15–20 mg/kg 2–3 times a day, adjusted to vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides concentration |
| Daptomycin Daptomycin A cyclic lipopeptide antibiotic that inhibits gram-positive bacteria. Lipopeptides and Lipoglycopeptides[6] | Not approved for children | 4 mg/kg once a day | |
| Teicoplanin Teicoplanin Lipoglycopeptide antibiotic from actinoplanes teichomyceticus active against gram-positive bacteria. It consists of five major components each with a different fatty acid moiety. Glycopeptidesa[7,8] | 6 mg/kg every 12 hours for 3 doses, then every 24 hours | ||
| Linezolid Linezolid An oxazolidinone and acetamide derived anti-bacterial agent and protein synthesis inhibitor that is used in the treatment of gram-positive bacterial infections of the skin and respiratory tract. Oxazolidinones[6-8] | 10 mg/kg every 12 hours | 600 mg 2 times/day |
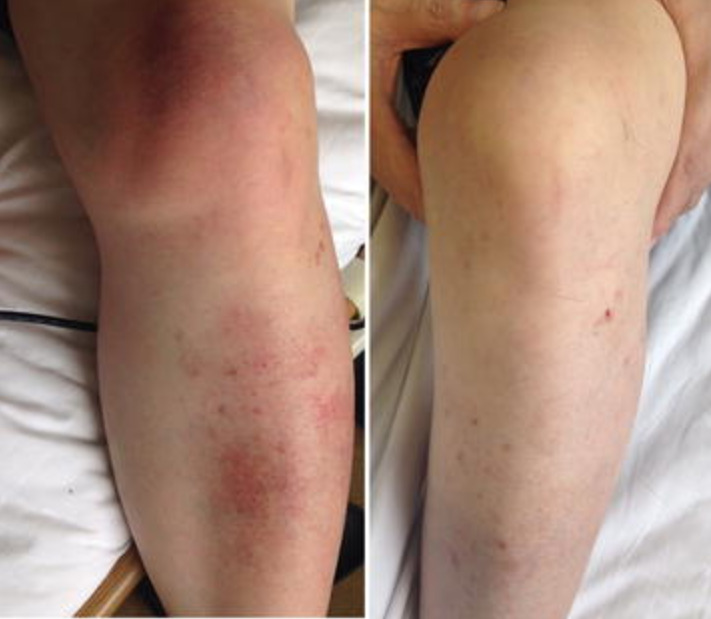
Cellulitis in the left lower leg and knee:
Left: Local swelling with salmon-pink skin discoloration and local warmth is evident.
Right: leg after 6 weeks of antibiotic therapy