Tricuspid regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) (TR) is a valvular defect that allows backflow of blood from the right ventricle to the right atrium during systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle. Tricuspid regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) can develop through a number of cardiac conditions that cause dilation of the right ventricle and tricuspid annulus. A blowing holosystolic murmur Holosystolic Murmur Tricuspid Valve Atresia (TVA) is best heard at the left lower sternal border. Mild TR may be asymptomatic or present with systemic venous congestion due to increased right atrial and venous pressures. Echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) can establish the diagnosis. Treatment focuses on heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) management, and surgery is reserved for severe disease.
Last updated: May 16, 2024
Tricuspid regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD) (TR) is the backflow of blood through the tricuspid valve Tricuspid valve The valve consisting of three cusps situated between the right atrium and right ventricle of the heart. Heart: Anatomy into the right atrium during ventricular systole Ventricular systole Cardiac Cycle.
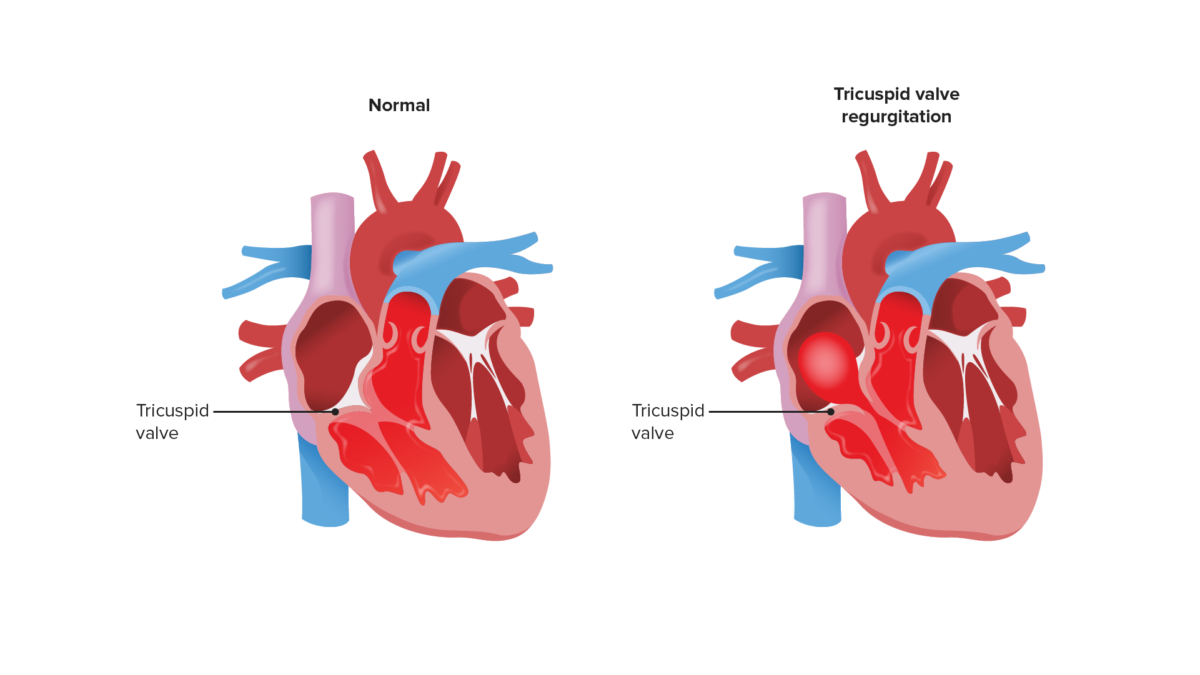
Image shows reflux of blood into the right atrium during systole. This backflow increases right atrial pressures.
Image by Lecturio.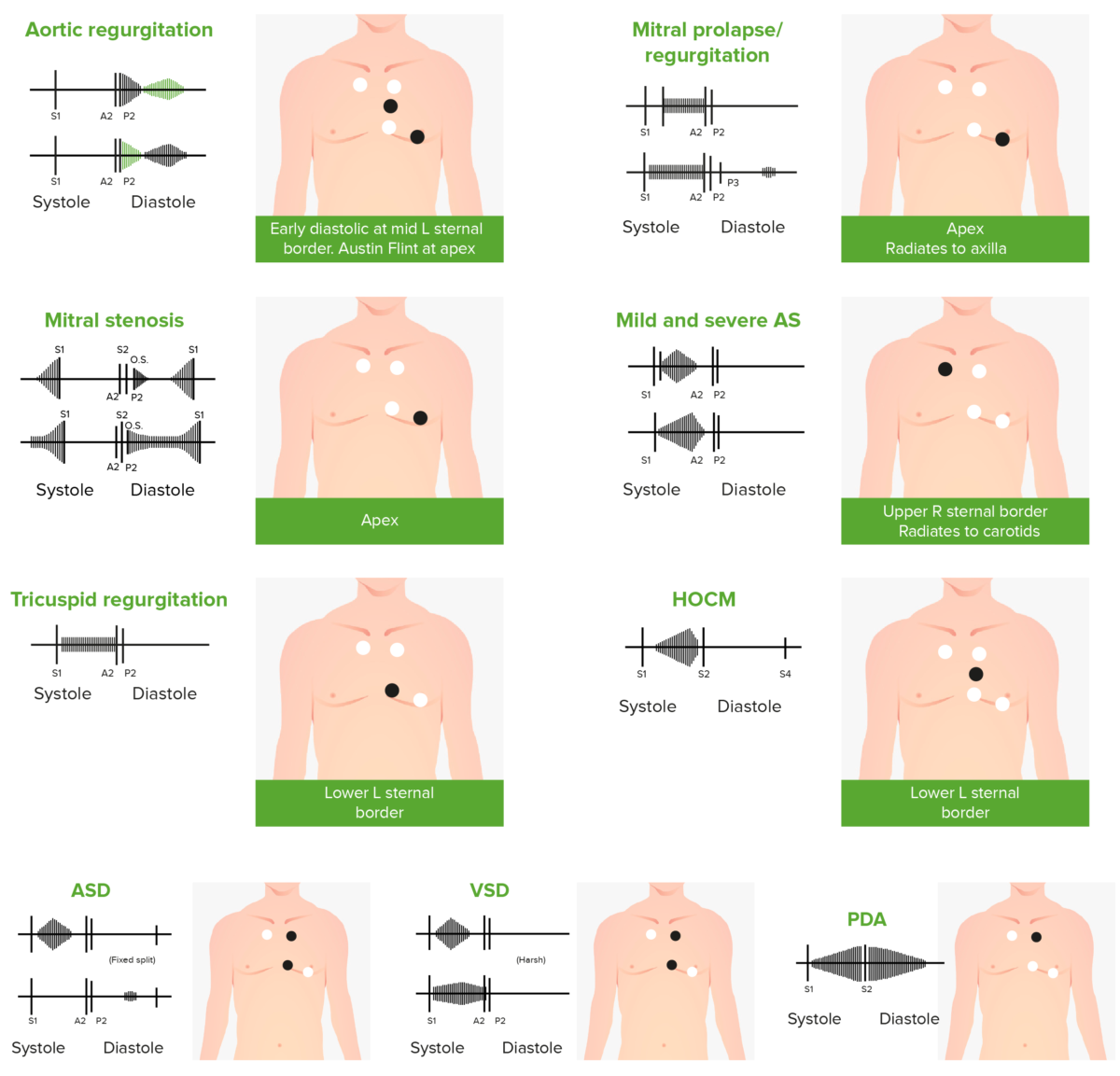
Phonocardiograms of abnormal heart sounds caused by the following cardiac defects:
aortic regurgitation, mitral valve prolapse, mitral stenosis (MS), aortic stenosis (AS), tricuspid regurgitation, hypertrophic obstructive cardiomyopathy (HOCM), atrial septal defect (ASD), ventricular septal defect (VSD), and patent ductus arteriosus (PDA)
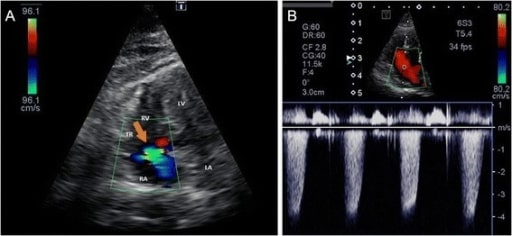
Color Doppler image of tricuspid regurgitation (a) and continuous Doppler (CW) image (b) from the left apical 4-chamber view optimized for the right ventricle
LA: left atrium, LV: left ventricle, RA: right atrium, RV: right ventricle, TR: tricuspid regurgitation (orange arrow)
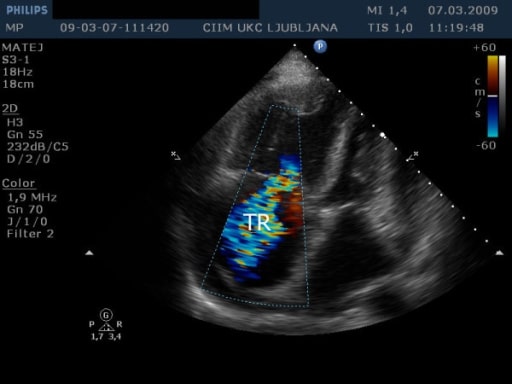
Transthoracic echocardiography from apical 4-chamber view shows massive tricuspid regurgitation (TR).
Image: “Transthoracic echocardiography” by Institute of Pathophysiology, Faculty of Medicine, University of Ljubljana, Slovenia. License: CC BY 2.0