Developmental dysplasia of the hip refers to a range of disorders of the hip joint Hip joint The hip joint is a ball-and-socket joint formed by the head of the femur and the acetabulum of the pelvis. The hip joint is the most stable joint in the body and is supported by a very strong capsule and several ligaments, allowing the joint to sustain forces that can be multiple times the total body weight. Hip Joint: Anatomy characterized by hip instability and resulting in subluxation Subluxation Radial Head Subluxation (Nursemaid’s Elbow) or dislocation that mostly presents during the first few months of life. The condition is often first recognized due to hip laxity on newborn Newborn An infant during the first 28 days after birth. Physical Examination of the Newborn exam. Developmental dysplasia of the hip occurs most commonly in otherwise healthy girls and often does not have an identifiable cause. Treatment is imperative to avoid complications, such as avascular necrosis Avascular Necrosis Hip Fractures of the femoral head and pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways with mobility. Management is dependent on the severity and age at diagnosis, with infants often treated with a Pavlik harness and children > 6 months of age often requiring open or closed surgical reduction.
Last updated: Jan 28, 2025
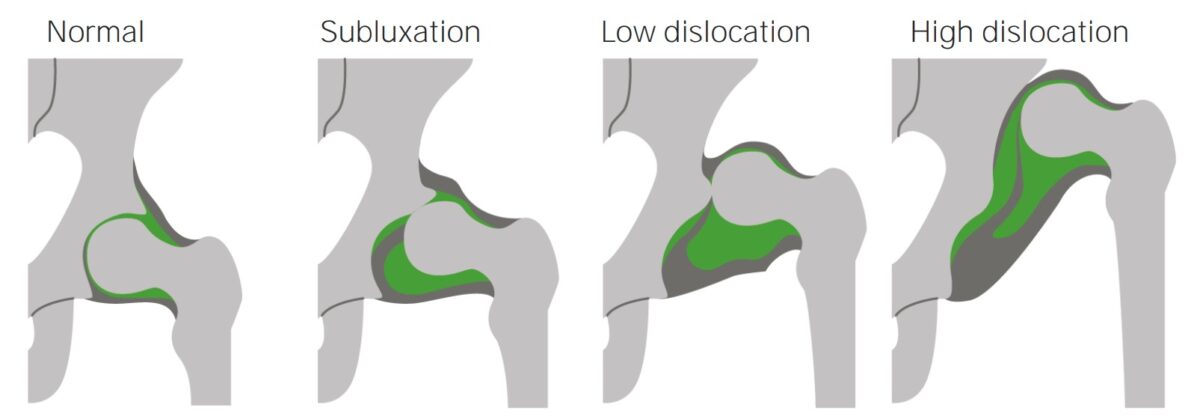
Normal hip joint and hip joints with progressively more severe dislocations
Image by Lecturio.Developmental dysplasia of the hip is caused by an inadequate reduction of the femoral head in the acetabulum. This can occur due to several factors.
Normal development of the hip is dependent on contact between the acetabulum and femoral head. However, in DDH:
| Neonates aged 0–2 months | Hip instability |
|---|---|
| Children 2–3 months old |
|
| Children who can walk |
|
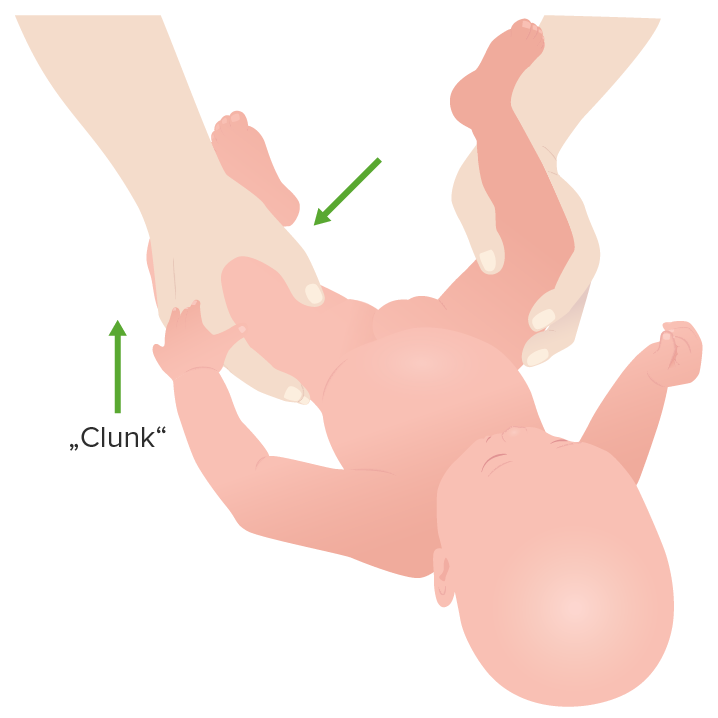
Hip clunk during the Ortolani maneuver
Image by Lecturio.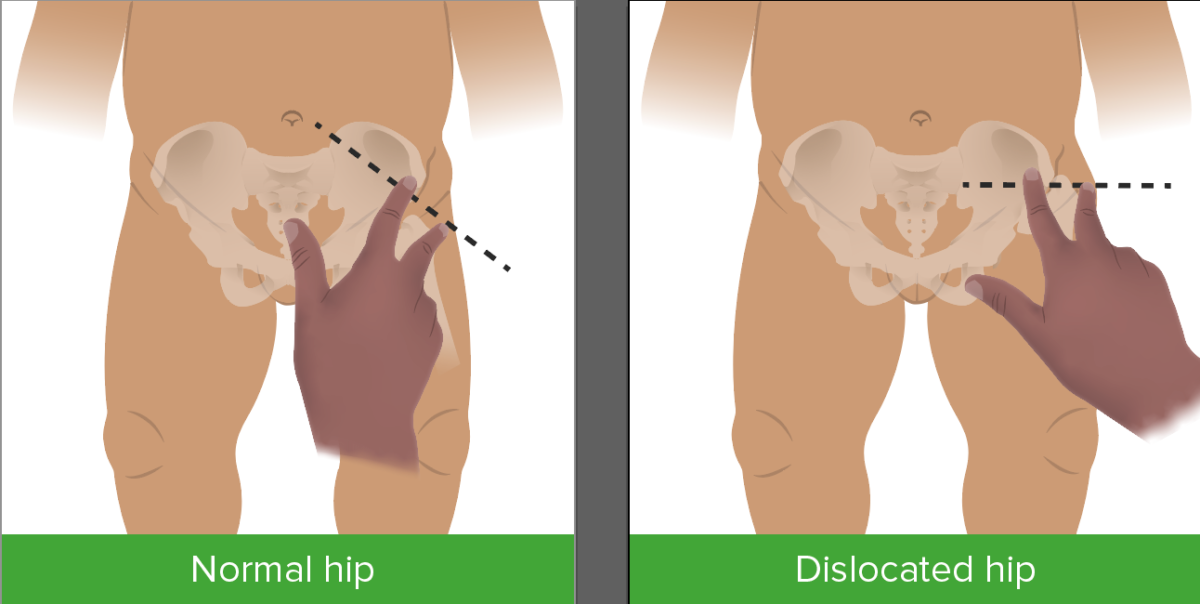
Klisic test for dysplasia of the hip
Image by Lecturio.The diagnosis of DDH is made clinically by demonstrating hip instability, asymmetry Asymmetry Examination of the Upper Limbs, and limited abduction Abduction Examination of the Upper Limbs of the hip.
Special tests have been devised to evaluate hip joint Hip joint The hip joint is a ball-and-socket joint formed by the head of the femur and the acetabulum of the pelvis. The hip joint is the most stable joint in the body and is supported by a very strong capsule and several ligaments, allowing the joint to sustain forces that can be multiple times the total body weight. Hip Joint: Anatomy structure, range of motion Range of motion The distance and direction to which a bone joint can be extended. Range of motion is a function of the condition of the joints, muscles, and connective tissues involved. Joint flexibility can be improved through appropriate muscle strength exercises. Examination of the Upper Limbs, and strength. The choice of which to employ is age-based.
Neonates aged 0–2 months
Children 2–3 months old
Children who can walk
Imaging can be used to confirm the diagnosis in children with risk factors and a normal physical examination, or in children with inconclusive physical examination findings.
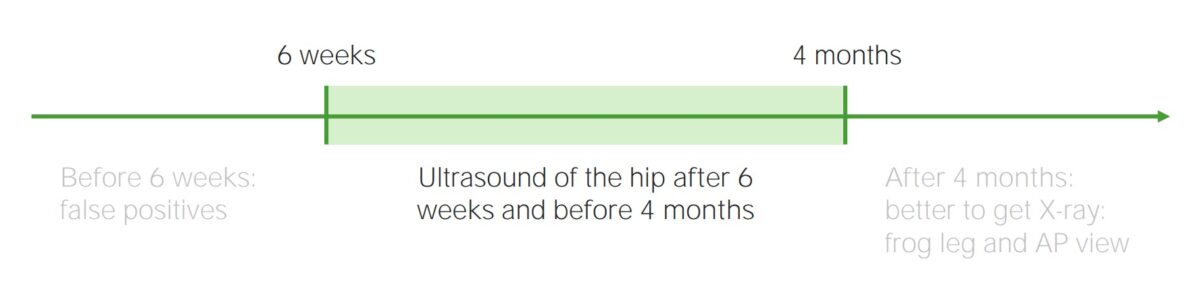
Window of opportunity for an optimal hip ultrasound
Image by Lecturio.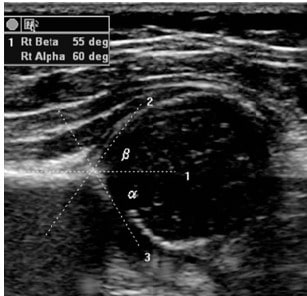
Normal infant hip ultrasound. More than 50% of the femoral head should be covered. A normal α angle is greater than 60°.
Image: “Hip dysplasia screening” by Trauma and Orthopaedics Department, Central Military University Emergency Hospital, Bucharest; “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania. License: CC BY 2.0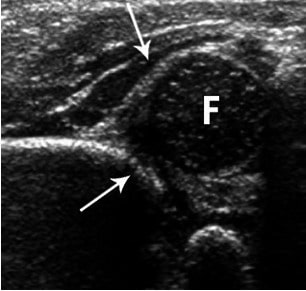
Hip showing moderate dysplasia. Arrows point to the acetabulum.
Image: “Hip showing moderate dysplasia” by Trauma and Orthopaedics Department, Central Military University Emergency Hospital, Bucharest; “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania. License: CC BY 2.0
Anteroposterior pelvic radiograph of an infant with bilateral DDH
Image: “Anteroposterior pelvic radiograph of an infant with bilateral DDH” by US National Library of Medicine. License: CC BY 4.0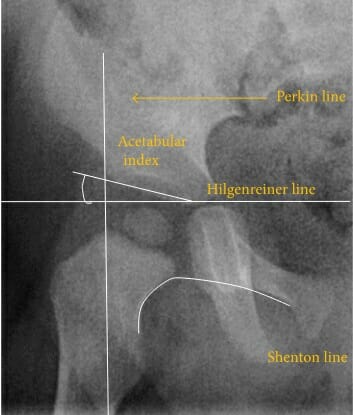
Reference lines and angles used in the evaluation DDH
Image: “X-ray of measurements on a normal hip” by Fernando Ruiz Santiago et al. License: CC BY 4.0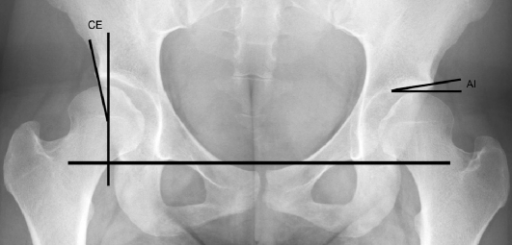
Section of a weight-bearing, anteroposterior, pelvic radiograph showing the assessment of the center-edge angle of Wiberg (CE) and the acetabular index angle of Tönnis (AI):
The teardrop line (the horizontal line interconnecting the hip joints) is the line of reference preceding construction of the angles.
| Newborns 0–4 weeks of age |
|
|---|---|
| Infants 4 weeks to 6 months of age |
|
| Infants between the ages of 6 months and 2 years |
|
| Children from 2–6 years of age | Open reductions are generally required. |
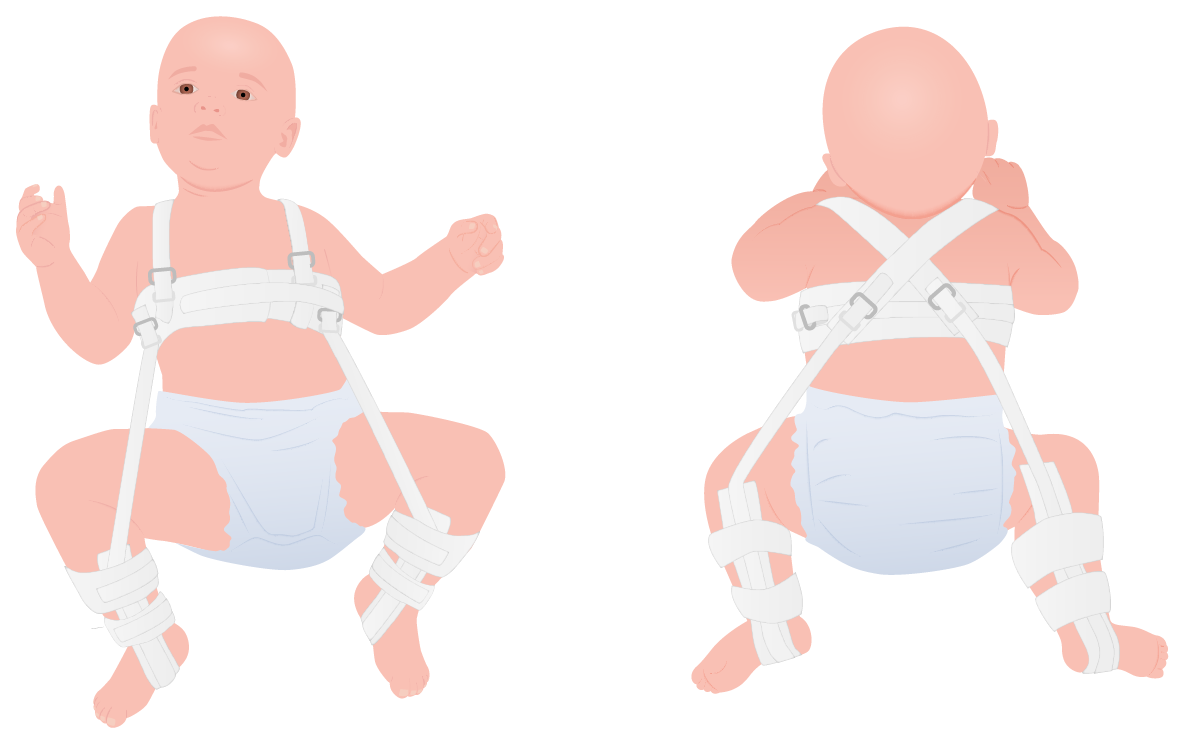
Pavlik harness
Image by Lecturio.